Risk-adjusted mortality has been successfully used to assess the quality of inpatient medical and surgical care
(1,
2). Although report cards have been developed for the assessment of mental health care
(3–
5), mortality has not been used as an indicator of the quality of mental health care, perhaps because there are few instances in which the delivery of mental health care can be directly linked to the death of a patient. One clear exception, and the focus of this paper, is the rate of death by suicide.
Suicide rates after discharge from inpatient care can be hypothesized to be associated with the quality of mental health care. The literature suggests that suicide rates are highest immediately after discharge from hospital treatment
(6–
8), that inadequate medication regimens may contribute to suicide risk
(9,
10), that most patients who commit suicide have had recent contact with a health professional
(11,
12), and that inadequate follow-up care or discharge planning may put people at greater risk for suicide
(13). Although these findings have received relatively limited empirical study thus far, they suggest that mental health service delivery may be associated with suicide risk.
This paper explores the potential value of using suicide rates as a measure of quality in large mental health care systems. First, we determine, after adjustment for case mix, whether significant variation in suicide rates exists across facilities in a large national network of hospitals (the U.S. Department of Veterans Affairs [VA]). Second, we explore the relationship of patients’ sociodemographic and diagnostic characteristics, as well as individual patterns of mental health service use, to the risk for suicide. Third, we explore whether facility-level measures of mental health care delivery or other facility characteristics (e.g., size, academic affiliation) are related to suicide risk after adjustment for several social environment factors, including the population suicide rate in the state, mean income in the state, the proportion of racial minority group members in the state population, and state-level measures of social capital.
Although the VA health care system is a national system, it is not centrally administered. Therefore, facility directors and mental health care line managers in VA facilities have discretion over facility-level policies on admissions, length of stay, and methods of aftercare. We hypothesized that shorter lengths of stay, poorer aftercare, and readmission to inpatient units would be associated with a higher risk of suicide, both at the individual level and at the facility level. Because social environment variables, such as state suicide rates, have been found to be correlated with suicide risk at the population level, we adjusted for those factors in facility-level analyses. This paper thus examines the association of suicide and factors from three domains: 1) individual patient characteristics and mental health care utilization (e.g., age, diagnosis, individual length of stay), 2) facility-level measures of delivery of mental health care (e.g., facility average length of stay), and 3) other facility characteristics (e.g., size and academic affiliation).
Method
Sample
The sample included all patients discharged with a diagnosis of major affective disorder, bipolar affective disorder, posttraumatic stress disorder (PTSD), or schizophrenia from psychiatric inpatient units in the VA health care system over the 4-year period from January 1, 1994, to December 31, 1998. The VA system is the largest health care system in the world, treating poor and disabled American military veterans for a complete array of medical and psychiatric illnesses. The four disorders we considered were chosen for their severity and prevalence within the VA inpatient system. Together, schizophrenia, other psychoses, and PTSD account for about 60% of VA inpatient stays
(14). Because as many as 80% of VA inpatient substance abuse beds were closed starting in 1996, we did not include patients discharged from substance abuse beds in these data. However, the majority of patients with both psychiatric and substance abuse diagnoses are discharged from general psychiatry beds (not substance abuse beds)
(14) and were thus eligible for inclusion in the sample. Acute care inpatient psychiatric units were defined by VA bed section codes 70–71, 75–79, 89, and 91–93.
Observations were unduplicated by including only the first discharge for each patient. The Patient Treatment File, a VA administrative database of all episodes of inpatient care delivered within the VA system, was used to identify the sample and unduplicate the data. The final sample consisted of 121,933 unique individuals. Because this was a secondary data analysis, informed consent was not obtained; however, the project was reviewed and approved by a human investigations committee.
Identification of Deaths
Once the sample was identified, Social Security numbers were used to merge data into the National Death Index to determine whether a patient was deceased within 1 year of discharge. Previous work with the National Death Index and VA data indicated that the Social Security number was the most valid matching criterion and that its use resulted in low false positive rates
(15). The cause of death was coded as suicide if it fell into the range of ICD-9 codes 950–959 (deaths before 1999) or ICD-10 codes X60-X84 (deaths in 1999).
Individual Risk Factors
Administrative data available from the Patient Treatment File were used to identify the sociodemographic and clinical characteristics of the sample, including age, race, marital status, service-connected disability status (none, <50%, >50%), year of inpatient discharge, whether discharge was to the community or to another institution, distance from home residence to the nearest VA hospital, and psychiatric diagnoses. Diagnoses, which were nonexclusive to allow for comorbidity, included PTSD, major depression, bipolar disorder, and schizophrenia (all subjects had at least one of those four diagnoses), as well as drug abuse/dependence, alcohol abuse/dependence, and other diagnoses (primarily other anxiety disorders and personality disorders). The measure of distance was determined as the distance between the geographic center of a subject’s home zip code and the center of the zip code of the nearest VA hospital and was used as a measure of geographic proximity to VA care.
It should be noted that, for this sample, no administrative data were available on history of suicide attempts, on whether the reason for admission was suicidal ideation, and on inpatient or outpatient medication regimens.
Delivery-of-Care Variables
Six variables reflected the delivery of mental health care: length of stay of the index hospitalization; readmission within 14, 30, or 180 days after discharge; whether the patient had an outpatient visit within 30 days after discharge; the total number of outpatient visits in the 6 months after discharge; the total number of inpatient days in the 6 months after discharge; and a measure of continuity of outpatient care after discharge—the number of 2-month periods in the 6 months after discharge in which the patient had at least two outpatient visits for his or her primary discharge diagnosis (range=0–3). The Patient Treatment File and the Outpatient Care File, a database of all VA outpatient care, were used to construct these variables.
Facility-Level Variables
Facility-level measures included mean values for the delivery-of-care variables described in the previous section, for example, the average length of stay of all psychiatric patients or the proportion of psychiatric patients who were readmitted within 14 days. In addition to examining facility-level measures of service delivery, we also explored other facility-level characteristics, including the proportion of the mental health budget spent on research and education (a measure of academic affiliation), the number of patients treated (a measure of facility size), and the proportion of budget spent on inpatient care (a measure of the emphasis on inpatient versus outpatient care).
Social Environment Variables
Four measures of social environment were included as potential confounders: 1) the statewide age-adjusted suicide rate (determined from Centers for Disease Control and Prevention mortality reports)
(16), 2) the statewide per capita income, 3) the percentage of racial minority group members in the population (from Census Bureau statistics)
(17), and 4) the statewide social capital index, a measure of social cohesion and trust in the community
(18). Social capital is not a new concept, but it has been reconceptualized by Robert Putnam
(18) in a way that allows measurement of the level of social cohesiveness and trust in a community. Putnam’s concept of social capital encompasses several domains: community organizational life (e.g., the level of membership in local organizations), engagement in public affairs (e.g., voting rates), community volunteerism, informal sociability (e.g., social contacts with neighbors), and social trust (i.e., the belief that other people are trustworthy). He combined measures of these domains into a single social capital index that has been shown to be strongly associated at the state level with a number of public health measures
(18–
21). We used this index in our statistical models.
Statistical Analyses
Analyses were conducted in two stages. First we calculated the suicide rate for each facility. Facilities were then compared to look for outliers by using methods described in detail by Selim and colleagues
(22). Expected mortality rates were calculated by using a multivariate logistic regression model that adjusted for age, gender, race, disability, distance to the VA, year of discharge, diagnosis, and discharge to the community. Outliers were identified as those facilities whose observed suicide rate was more than two standard deviations away from the case-mix-adjusted (i.e., expected) rate. Suicide rates were analyzed by collapsing data across all 5 years of the study period.
The second set of analyses examined the relationship of individual, facility, and social environment factors to the risk of suicide. First, we fit multivariate Poisson models to determine which individual characteristics (e.g., sociodemographic characteristics, diagnosis) were statistically significant predictors of suicide risk. Poisson models were used to more accurately model the nonuniform distribution of deaths across the 1-year follow-up. This nonuniformity of deaths over time is not reflected in logistic regression, which is more commonly used for these types of analyses but which sums all events without consideration of time to event
(22). In addition to fitting Poisson regression models, we used generalized estimated equations procedures
(23) to cluster data for patients within the same facility, in order to account for the reduction in intersubject variation within facilities and to allow for the analysis of facility- and state-level measures.
We next examined the association of suicide and patient-level measures of service delivery. Multivariate Poisson models were fit separately for each delivery-of-care variable, for two reasons. First, a number of factors were highly correlated with each other and could not be included in the models together. Second, different variables were observed over different lengths of time, depending on how they were calculated. For example, the measure of whether a patient received an outpatient visit within 30 days of discharge could only be calculated among those patients who survived at least 30 days. Therefore, we fit models for such variables only among subjects who had survived long enough for the delivery-of-care variable to be an informative predictor.
After exploring individual measures of delivery of care, we explored facility-level measures of delivery of care and other facility characteristics such as size and academic affiliation while controlling for social environment measures. Analyses proceeded as described earlier, with each variable adjusted for important indicators of case mix. Generalized estimated equations models were used to adjust for the high correlation of observations within states.
Results
Of 121,933 unique patients included in the sample, 3,588 (2.9%) died within 1 year of discharge. Of those, 481 (0.4% of the total sample, 13.4% of deaths) died of suicide. Suicide deaths were concentrated in the first 6 months after discharge, with 46% in the first 3 months, 18.3% in months 4–6, 20.4% in months 6–9, and 15.4% in months 9–12.
Comparisons of Facilities
The sample was derived from a total of 128 VA facilities. Facilities were compared on the suicide rates of patients treated over all 5 years of the study period. The average observed rate across facilities was 44.53 suicide deaths per 10,000 person-years (SD=31.99).
When we ranked facilities separately based on the observed and case-mix-adjusted mortality rates, ranking changed dramatically from the observed to the adjusted rates, indicating that adjustment for case mix significantly altered rankings (only 16 facilities retained their rank from one method to the other). In addition, investigations for outliers yielded significant variation in suicide rates across facilities: 15 facilities (10.1%) had rates that were significantly lower than expected, and 20 facilities (13.5%) had significantly higher-than-expected rates, given their patients’ characteristics.
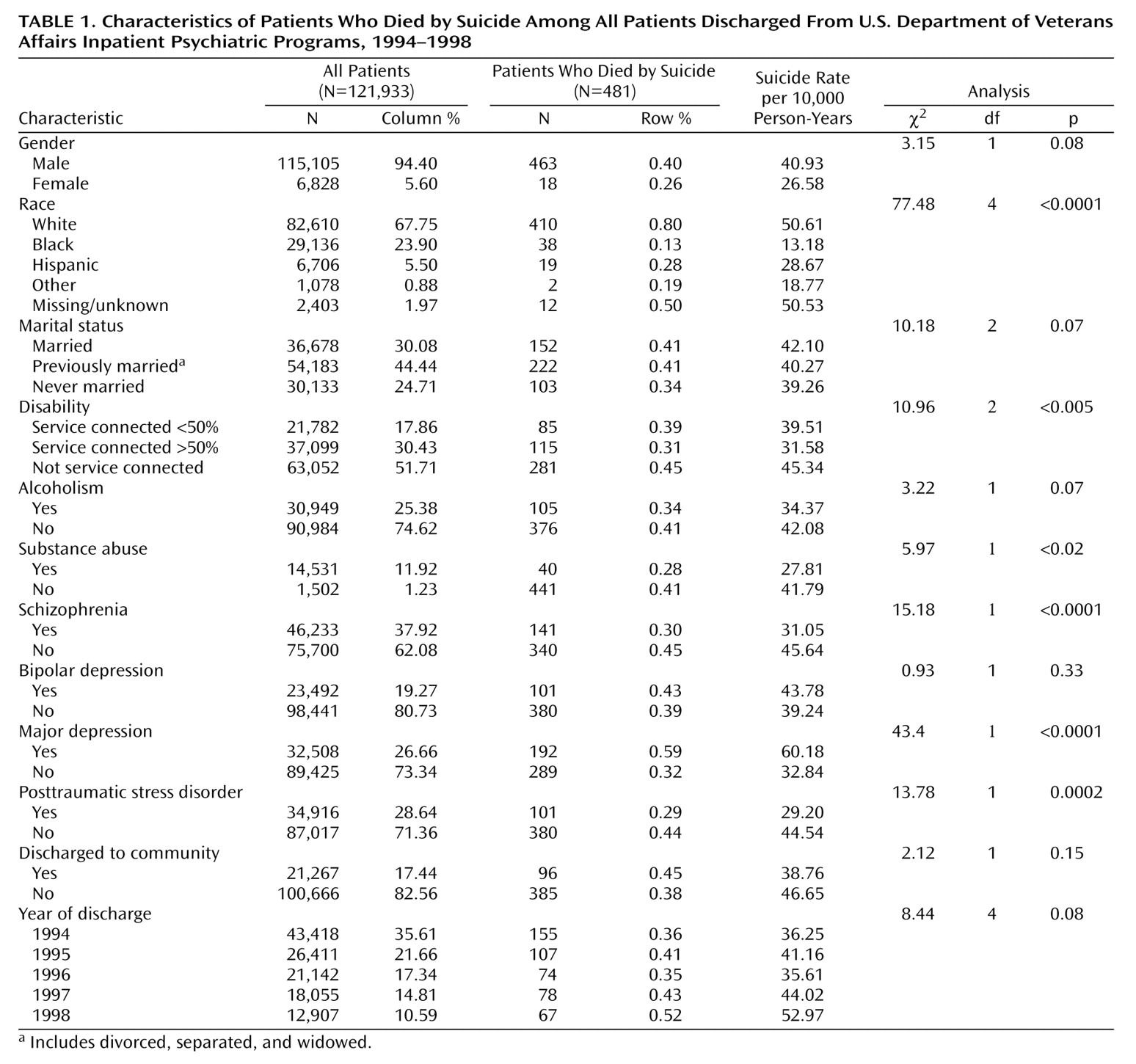
Service Delivery and Suicide
Table 1 summarizes the characteristics of the sample and the bivariate associations between demographic variables, diagnostic variables, and suicide mortality. The mean age of the sample was 48.17 years (SD=11.68), and the average distance between subjects’ homes and the nearest VA hospital was 12.96 miles (SD=17.32) (data not shown). The diagnostic variables listed in
Table 1 are not mutually exclusive, and patients with more than one diagnosis are represented. Suicide rates were significantly higher among white patients and those for whom data on race were missing or unknown (p<0.0001) and significantly lower among those with service-connected disability (p<0.005) (
Table 1). Rates were higher with increasing age (F=8.81, df=1, 120579, p<0.005) and increasing distance from the VA (F=7.89, df=1, 120579, p<0.005) (data not shown). There was no association with marital status or discharge to the community. Suicide rates were significantly lower among those with a diagnosis of drug abuse/dependence, schizophrenia, and PTSD, compared to patients without those disorders, but significantly higher among those with unipolar depression. The relationship of year of discharge and suicide was not significant (p=0.08).
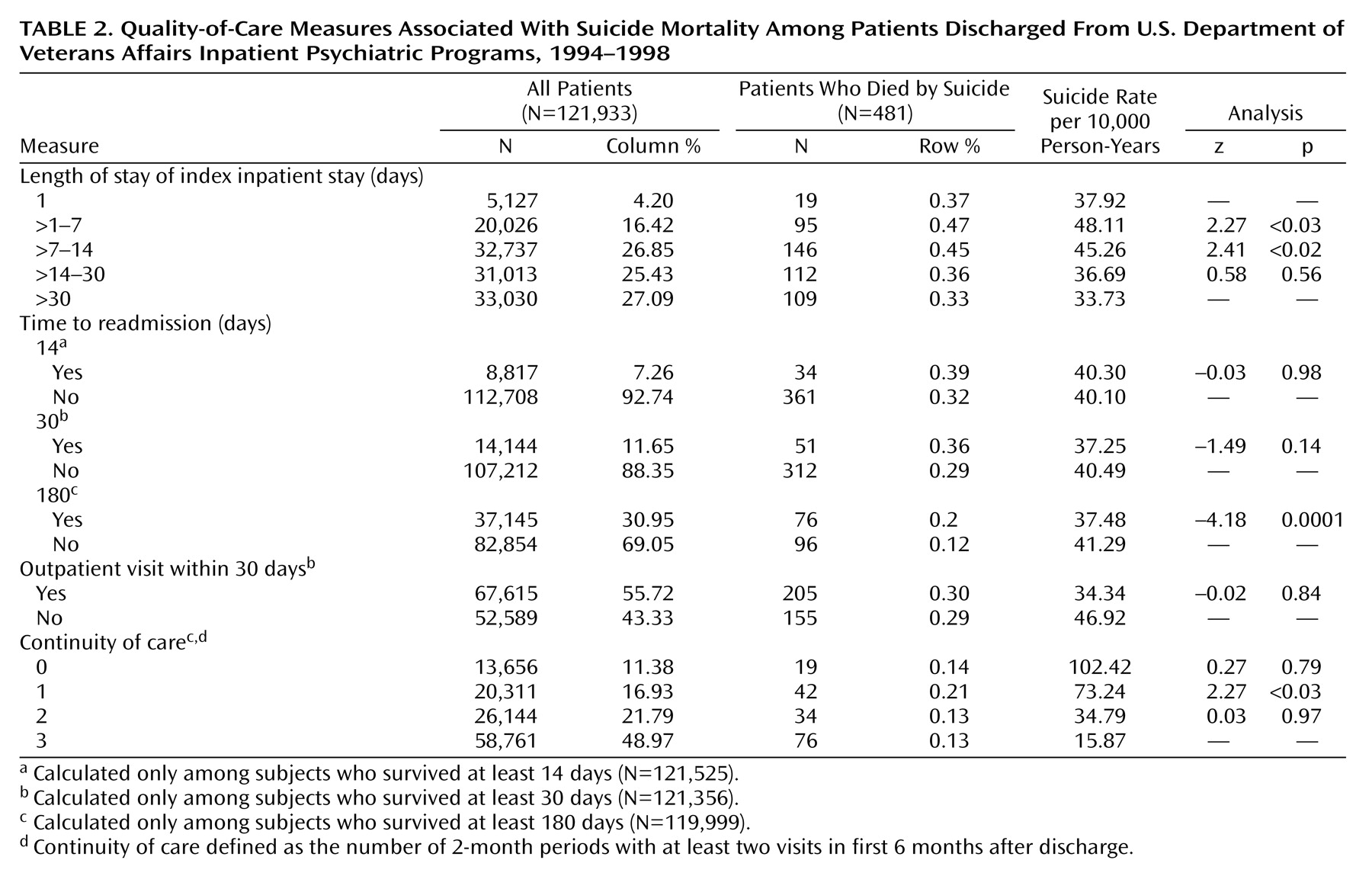
Table 2 presents the distribution of categorical delivery-of-care variables. Unadjusted mortality rates indicate that patients with lengths of stay less than 14 days and those with poor continuity of care were at significantly higher risk for suicide, and those who were readmitted within the first 6 months after discharge were at significantly lower risk.
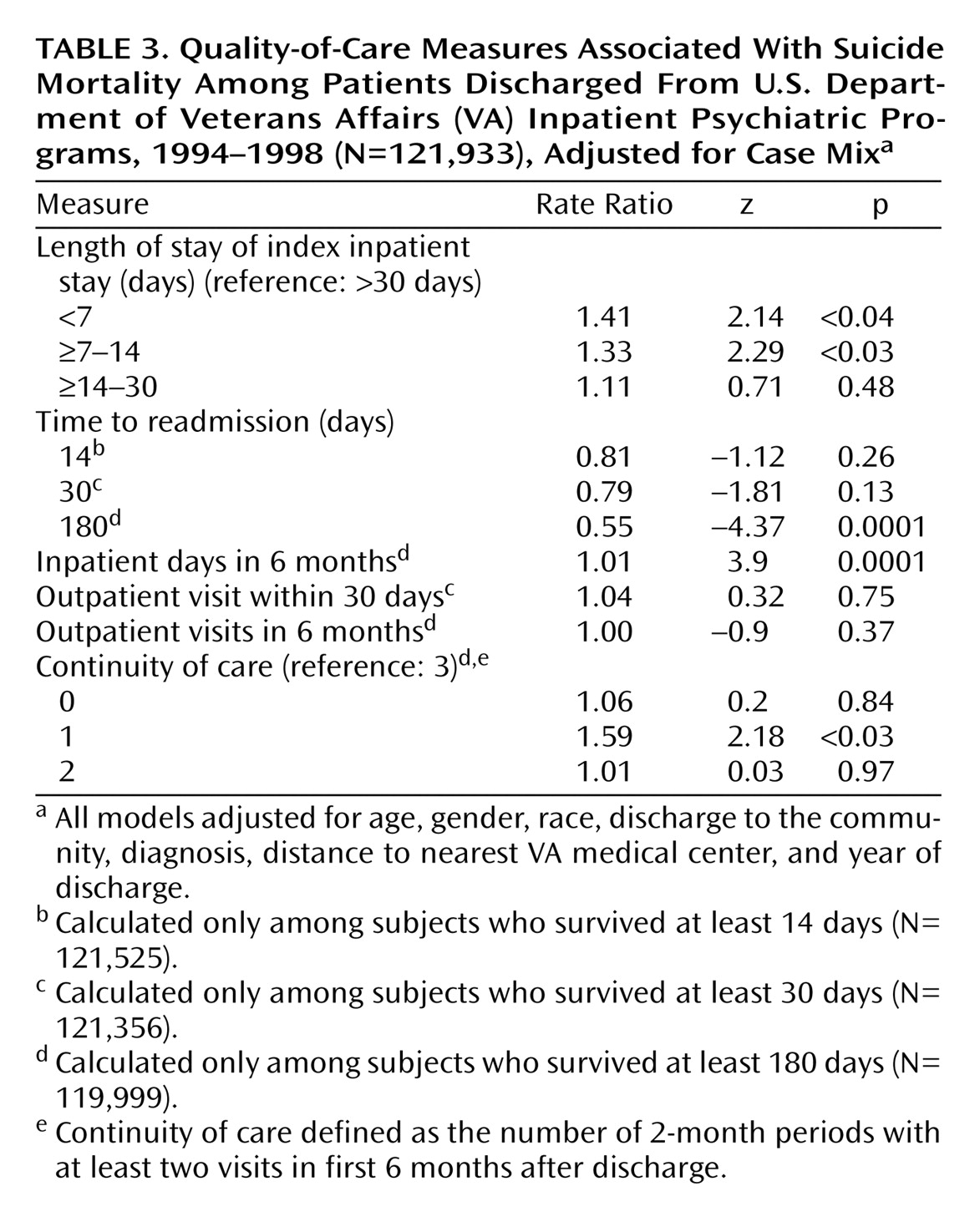
Table 3 presents data for the delivery-of-care variables adjusted for case-mix variables such as age, race, gender, discharge to the community, diagnosis, distance to the nearest VA, and year of discharge. Even after this adjustment, several delivery-of-care variables were significantly associated with suicide: patients with shorter lengths of stay were at higher risk, patients who were readmitted within 6 months of discharge were at lower risk, larger numbers of inpatient days in the 6 months after discharge were associated with lower risk, and patients who had at least two outpatient visits in only one of three 2-month periods in the first 6 months after discharge were at higher risk.
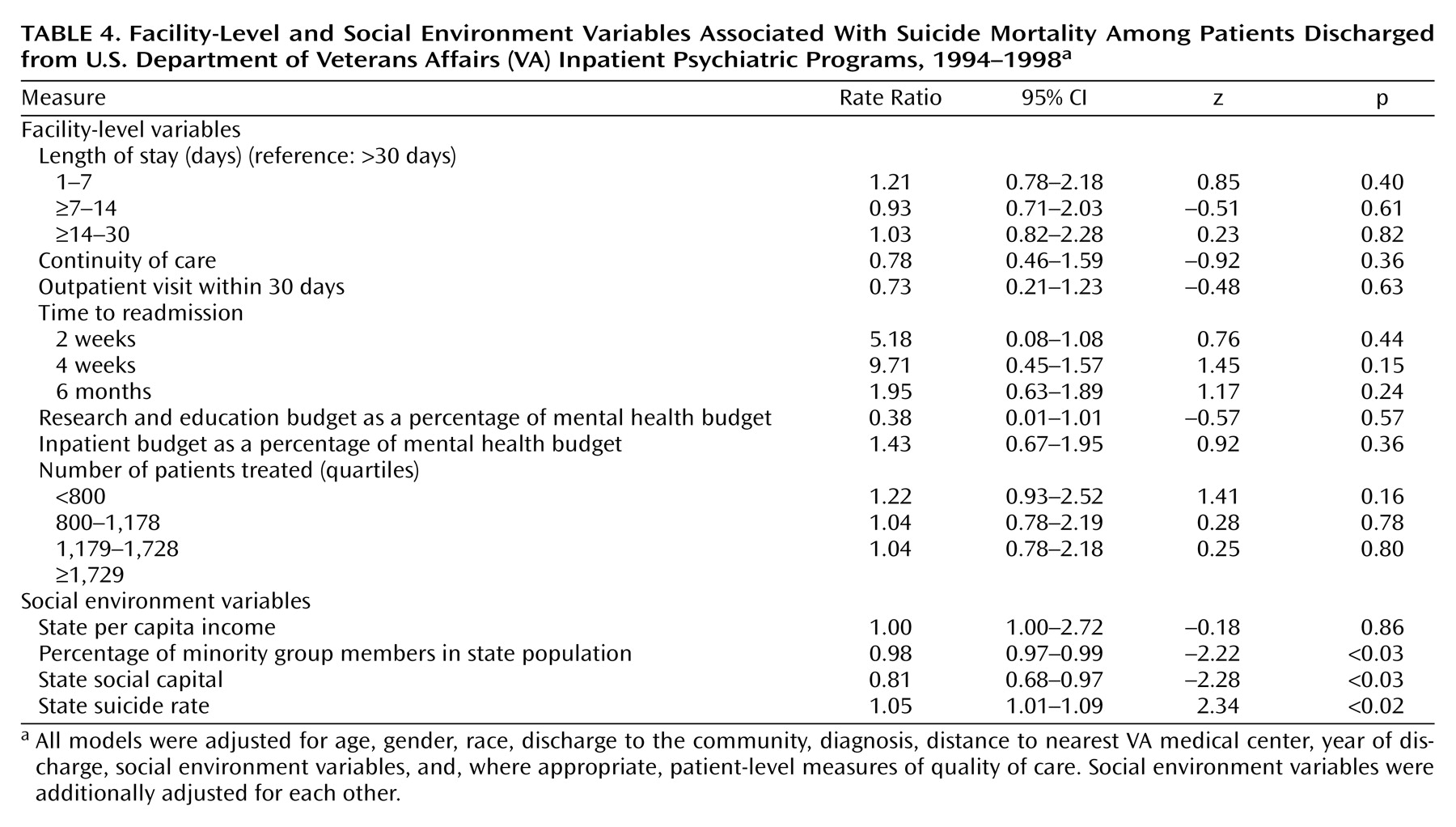
Table 4 presents the results of multivariate models of facility-level characteristics adjusted for case-mix and social environment variables. No facility-level characteristics were significantly associated with suicide risk. However, suicide risk was lower in states that had higher social capital and in states where the percentage of minority group members in the populations was higher. Suicide rates were significantly higher in states with higher general statewide suicide rates.
Discussion
Suicide Rates as a Quality Indicator
We identified a number of disadvantages to using suicide rates as a quality-of-care indicator. First, to use these rates for this purpose, death data are required for patients who may no longer be receiving care in the system. Unlike in-hospital mortality rates, which can be calculated by using administrative data, mortality rates for discharged patients must be determined by means of longer-term follow-up with National Death Index data and cannot be calculated in a timely fashion. Second, the rates of suicide are quite low, even within this highly vulnerable patient population. As such, the rates are unstable and subject to large variation with small changes in numbers. Suicide rates in a single year are thus not likely to be a useful quality indicator except in systems with many very large facilities. The third disadvantage is that risk adjustment is imperfect; even with the large numbers of predictors in the risk-adjusted models, R2 corollary measures in these data never rose above 5%. Comparisons of rates across facilities may be impeded because so much variation in individual risk is left unexplained by administrative risk adjustment.
Despite the disadvantages of using suicide rates as a routine quality-of-care indicator, the 5-year suicide rates across facilities in the VA system showed significant variation, and we proceeded to explore institutional and facility-level characteristics that increased the risk of suicide.
Case-Mix Variables and Suicide Risk
In observing variation across facilities as well as the associations between service delivery and suicide risk, it was important to adjust for case-mix variables. In these analyses, the sociodemographic characteristics found to significantly predict suicide were similar to those identified in other studies: risk increases with age, compared to risk in those age 40–60 years
(24,
25), and is higher among males
(26) and patients who are white
(27,
28). In general, patterns of risk across diagnostic groups were in the expected directions, with the highest risk groups being those with unipolar and bipolar depression and the lowest risk groups being those with PTSD and substance use disorders.
One interesting variable that was significant in all of the multivariate models was the distance between a veteran’s home and the nearest VA hospital. This finding could possibly reflect variation in access to mental health care: veterans who lived farther from a VA facility may be at higher risk because of poorer access to outpatient care, difficulty getting to the VA in a crisis, or greater social isolation. Distance to the nearest VA hospital could also be a social environment variable that reflects the degree to which the patient lives in a rural environment, a factor that has been associated with suicide risk
(29).
Individual-Level Delivery of Care and Suicide Risk
For suicide rates to be a meaningful quality indicator, they must not only distinguish providers from one another, but should also be related to variation in service delivery. We found that ready access to mental health care is associated with a reduced risk of suicide at the individual patient level. The data suggest that patients with inpatient stays shorter than 14 days were at higher risk for suicide, perhaps because they were prematurely discharged, although a second possible explanation is that some patients may leave programs against medical advice because they intend to commit suicide. Although this hypothesis cannot be tested with these data, it implies that only careful patient assessment and use of involuntary commitment to prevent high-risk patients from leaving prematurely could prevent such ill-timed discharges.
Unexpectedly, we found that readmission within 6 months was protective against suicide risk. Although this finding may seem counterintuitive, because readmission is often considered an adverse outcome, it is likely to reflect successful identification and inpatient treatment of persistent suicidality.
Finally, we found that poor continuity of care was associated with higher suicide risk. It should be noted that those who had no follow-up visits were at equal risk to those who had more than two visits; however, the patients with no follow-up may have left the VA system and sought treatment elsewhere. Those at highest risk were veterans who had two or more visits in only one 2-month period during the first 6 months after discharge. Such a level of care is clearly inadequate for recently discharged inpatients, even for routine monitoring of symptoms and quality of life. We cannot determine from these data if patients were given appointments that they never kept, or whether there was a breakdown in communication between inpatient and outpatient providers. However, it is possible that facilities could reduce risk with more effective communication and active follow-up of patients who miss appointments.
Facility-Level Delivery of Care and Suicide Risk
Factors that reflected facility-level practice patterns showed no association with suicide risk. In addition, neither the size of the facility nor the level of academic affiliation was significantly related to suicide mortality. These nonsignificant findings imply that the most important risk factors are operating at the individual level and that systemic changes in these facility-level measures may not significantly reduce the risk of suicide.
It should be noted that there are two variables missing from these data that are likely to be associated with suicide risk: a past history of suicide attempts and medication use. The inability to adjust for these factors may leave some residual confounding in the facility-level analyses, as both the proportion of patients with past attempts and the medication prescribing patterns could differ over facilities. However, although these variables would likely be significant predictors on their own, it is unlikely that the ability to adjust for these variables would reveal significant associations between facility-level delivery-of-care variables and suicide rates.
Social Environment Variables and Suicide Risk
A number of studies indicated that social environment plays an important role in the risk for suicide
(30,
31). In addition, recent work from our group showed that social capital is associated with continuity of mental health care
(32). Therefore, although these factors are not easily modifiable or particularly clinically relevant, it is important to note that analyses of suicide rates at a macro level (e.g., across facilities or systems) should adjust for these environmental variables as important potential confounders.
Conclusions and Clinical Implications
This is the first study, to our knowledge, to examine the association between delivery-of-care measures and the risk for suicide in a large health care system. The data suggest, first, that although there is significant variation across facilities, suicide data do not lend themselves to being used as a quality measure for mental health care: suicide rates are too unstable, the data are difficult to collect, and there is no association of suicide rates with facility-level quality-of-care variables. Second, some aspects of the delivery of mental health care at the patient level are associated with higher suicide risk. However, variations in patterns of service delivery at the system level are not significantly associated with suicide risk, suggesting that individual-level measures do not reflect variation in overall quality of care but rather variation in individual propensity to commit suicide. Finally, the social environment, particularly the quality of social capital, is a strong predictor of suicide risk, even above individual and facility characteristics, and should be adjusted for in models of population suicide risk.
These data do not suggest that cases of suicide should not be systematically investigated as sentinel events that potentially could have been avoided with more effective identification and intervention. These data confirm that the postdischarge period is the time of greatest risk, that patients require careful predischarge assessment, and that appropriate follow-up care in an outpatient setting, as well as rehospitalization when necessary, may help reduce the risk for individual patients.