In outcome studies of anorexia nervosa, crude mortality figures are often quoted
(1) and show a very wide variation, from 0% to 18%
(2,
3). This variation is not surprising considering the very different methodologies used. Initial patient selection can at one extreme be based on national case register information of all diagnosed cases
(4), and at the other be based on carefully diagnosed but highly selected patients in a tertiary referral inpatient setting. For the former there may be doubts about diagnostic accuracy; for the latter there may be doubts about how representative the cohort will be of all patients with anorexia nervosa in a given population. Indeed, in some tertiary referral centers, the base population is not known. Follow-up periods have varied from 5 to 33 years
(3,
5), and crude mortality figures quoted will naturally rise with longer follow-up periods (i.e., as a cohort ages, more cases will die). Many studies have not attempted to calculate standardized mortality ratios, but increasingly standardized mortality ratios and other standardized methods of reporting mortality are being published
(1,
6). Most of these studies have shown a standardized mortality ratio between 4 and 13 for anorexia nervosa, with a few notable outliers reporting very low
(2,
7) or high
(8) standardized mortality ratios. Another limitation in much of the literature is sample size. For example, the study by Norring and Sohlberg
(8) had a sample size of just 25. Most clinically based studies have had fewer than a hundred patients at inception, with four studies having between 100 and 210 patients
(7,
9–11); a fifth study included 332 patients
(12).
The current study attempts to overcome some of these methodological limitations. It is a long-term follow-up study (up to 35 years) of nearly all patients from a catchment area in Northeast Scotland (Grampian Region). In this locality, all patients referred to National Health Service psychiatric, psychological, and other mental health services—whether inpatient, day patient or outpatient—are identifiable, and there is very limited access to and uptake of private services. All the case notes of suspected patients were checked for diagnostic accuracy, and this produced a large intake cohort of 524 cases.
The aims of the study were to establish the standardized mortality ratio for patients with anorexia nervosa seen in specialist services and to analyze the causes of death.
Method
Patients with a diagnosis of any eating disorder category between 1965 and 1999 were identified from the Grampian psychiatric case register, patient administration systems, and the Eating Disorder Service database. All case notes were checked to confirm or refute a diagnosis of anorexia nervosa. Over these years, diagnostic systems changed from ICD-7 to ICD-10, and case notes did not always contain sufficient information to make a diagnosis of anorexia nervosa according to current ICD-10 or DSM criteria. In older ICD versions there were no codes for eating disorders. However, the Aberdeen Psychiatric Case Register had a category for anorexia nervosa beginning in 1965. ICD-9 was introduced in 1980 with a category for anorexia nervosa (307.1), and all those patients were included for case note review. All notes with a coding for any eating disorder (F50) from ICD-10 were scrutinized in case of mistakes in coding. As in a previously published study
(13), a diagnosis of anorexia nervosa was confirmed if the case notes contained the following: 1) a recorded diagnosis of anorexia nervosa, 2) significant weight loss, 3) amenorrhea or evidence of characteristic psychopathology, and 4) no other diagnosis of severe mental illness such as depression or schizophrenia during the index episode. The intention in choosing these criteria was to include all patients with anorexia nervosa and not to exclude those for whom there was insufficient recorded data. In some cases, particularly the earlier ones, the characteristic psychopathology was not described but could be inferred from the degree of weight loss, resistance to normal eating, and the presence of amenorrhea. It seemed important to include those patients even though the full modern diagnostic criteria were not documented. When there was genuine doubt about the diagnosis, patients were excluded. Of the patients with a case note diagnosis of anorexia nervosa, 32% were excluded because they did not meet the study criteria.
For the majority of patients, their index first contact was with general psychiatric services. In those services, no standardized assessments were performed from which severity of illness could be determined.
No patients were involved in any controlled therapeutic trial. Most would have had an eclectic variable mix of outpatient and inpatient treatment with a variety of individual, group, and family therapeutic approaches. It was therefore impossible to assess any associations between therapy and outcome, including mortality.
All cases were traced to the current health authority area using the Community Health Index and the National Health Service central register. This process identified some patients who had died. These and any other cases remaining untraced were then double checked in the register of deaths (General Register Office for Scotland) to determine current status. The register of deaths was also consulted for the recorded causes of death.
The crude mortality rate was calculated simply by dividing the number of deaths by the total number of the cohort who were traced.
To calculate the standardized mortality ratio, the time of interest for each patient was taken as the year the patient was seen at the clinic to either the year of death or mid-2002. For each individual this time was broken into episodes according to 5-year age bands, and into grouped time bands from tables of national statistics (before 1964–1979, 1980–1989, and from 1990 onward). Appropriate death rates for men and women in the Grampian population in 1974, 1985, and 1995 were obtained from the Demography and Dissemination Branch of the General Register Office for Scotland. These were used to calculate standardized mortality ratios and 95% confidence intervals. The methods were those of Clayton and Hill
(14), implemented by using the Stata statistical package
(15).
Results
A diagnosis of anorexia nervosa was confirmed by case note review for 524 cases. Thirty-seven (7.1%) were male. The mean age at the time the patient was seen at the specialist service was 20.1 years (SD=6.8).
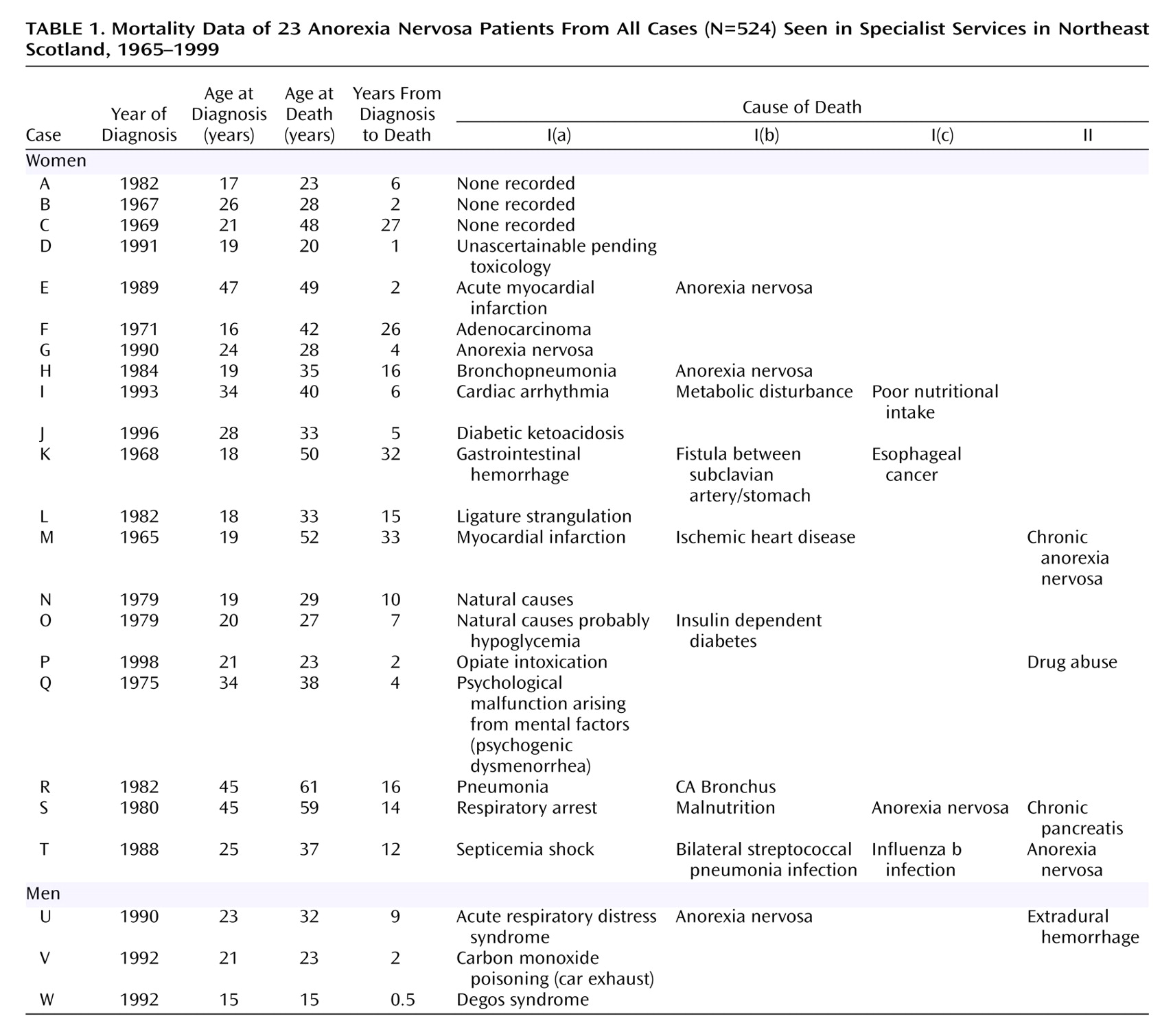
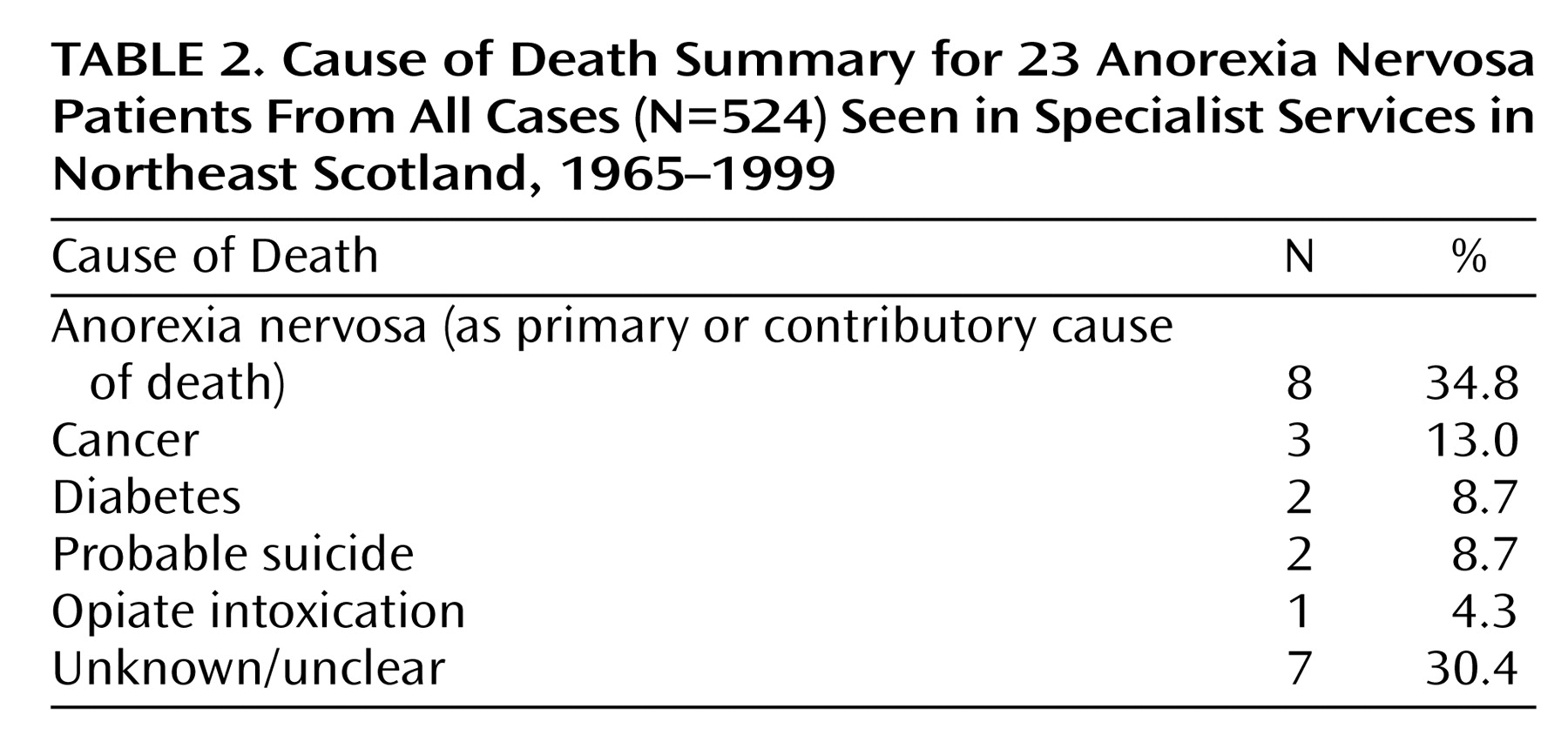
Five hundred seven (96.8%) were traced including 23 who died (one of these during the study). This gives a crude mortality rate of 4.5%. The recorded causes of death for these patients are listed in
Table 1 and summarized in
Table 2. Surprisingly, in seven cases, the cause of death was unknown, uncertain, or in one case difficult to understand as a cause of death: “psychological malfunction arising from mental factors (psychogenic dysmenorrhea).” Eight had anorexia nervosa as a cause of death or a contributory cause (including one in which poor nutritional intake was an additional cause).
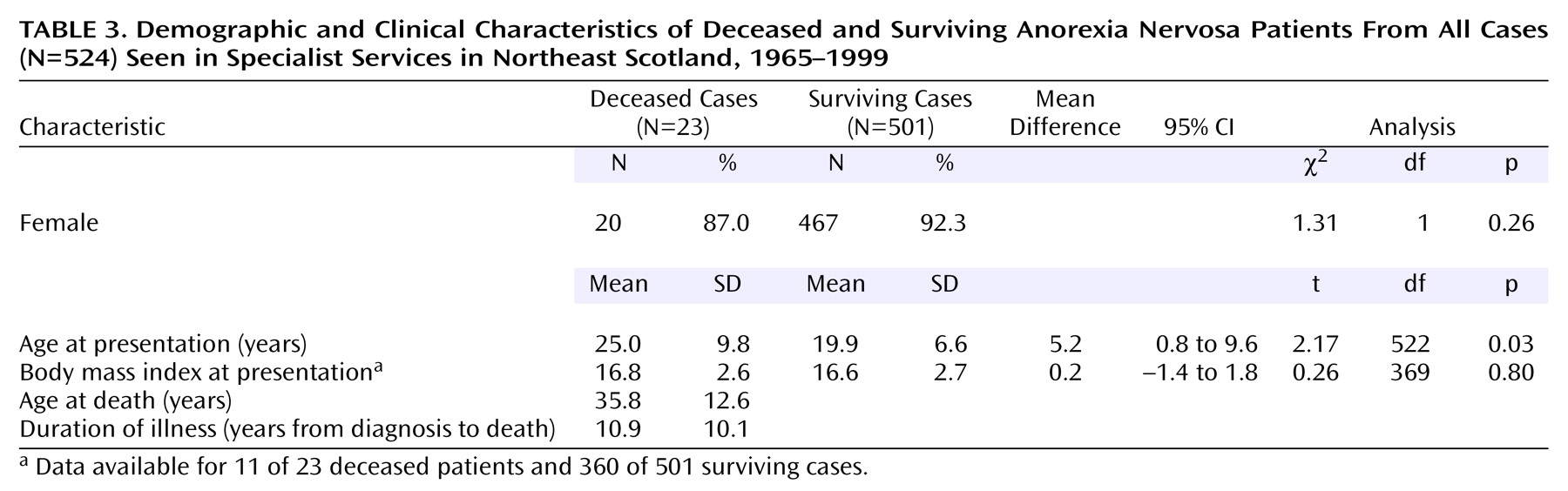
Table 3 shows a comparison of some demographic details comparing the deceased patients with surviving cases. The deceased patients were significantly older at the time they were seen in the specialist service and had sought treatment less recently. The median time from the specialist service visit to death was 11 years (interquartile range=3 to 17), with a mean age of death at 35.8 years (SD=12.6).
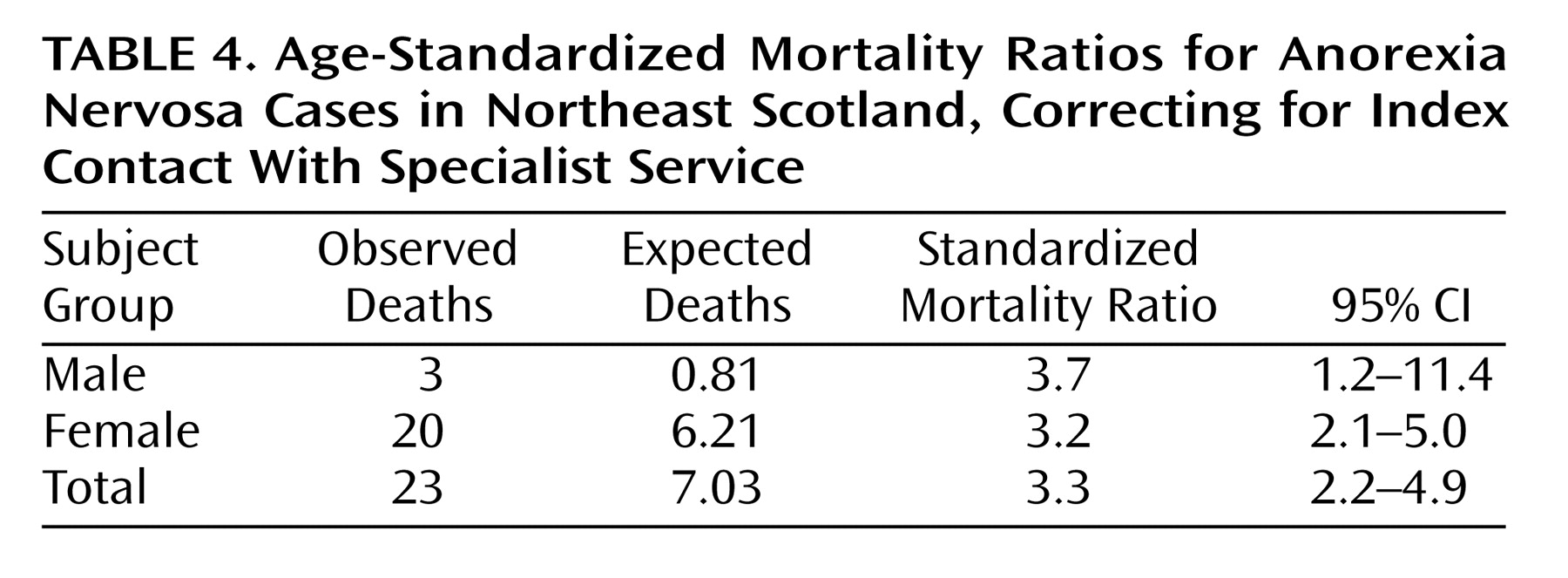
The standardized mortality ratios in
Table 4 have been corrected for age at index contact with specialist service, gender, and year of index contact. The figures obtained without correcting for year of index contact were very similar.
Discussion
This large follow-up study from a known population base, with diagnosis confirmed by case note review for each patient, shows that there is a more than threefold increased risk of premature death in patients diagnosed with anorexia nervosa. This finding is in keeping with most of the literature, although the standardized mortality ratio in published studies has ranged from 0.71 to 17.8
(6,
7,
11,
16,
17). It is very difficult to know what might have happened to the 17 untraced patients. It seems unlikely that they died in a developed country, since there are international systems in place to backtrack deaths to the U.K. Register of Births, Marriages and Deaths. It seems more likely that they moved abroad and were not picked up by the Community Health Index system.
In a smaller, earlier study in Northeast Scotland, a slightly higher standardized mortality ratio of 4.7 was calculated and compared with a lower standardized mortality ratio of 1.4 at St. George’s Hospital in London
(9). It was suggested in this previous study that the presence of a well-developed specialist service for eating disorders at St. George’s Hospital may have been responsible for lower mortality there. Although there is now an outpatient specialist treatment service in the region based in Aberdeen, it is too early to see any effect on mortality rates that this might have produced, bearing in mind the median time from presentation to death is 11 years.
Anorexia nervosa was only featured on about one-third of death certificates but may well have played a part in the death in other cases. In the two patients who died from complications of diabetes, the eating disorder may have been a contributory factor. Neilsen et al.
(18) found a standardized mortality ratio for diabetes of 4.1 and for anorexia nervosa a standardized mortality ratio of 8.9. However, when these conditions were combined, the standardized mortality ratio was 14.5, suggesting it is a very dangerous combination. Patients are known to lower the dose of insulin as a means of purging calories through glycosuria
(18).
Given the recorded cause of death, it is likely that two patients committed suicide and one other who died of opiate intoxication was a possible suicide, which suggests a crude suicide mortality rate of 0.57%. In a meta-analysis by Harris and Barraclough
(19), the standardized mortality ratio for suicide in anorexia nervosa was 23, and some have suggested that while improved treatment and services may prevent death from anorexia nervosa and the consequences of starvation, there may be an increase in suicide
(12). There were insufficient numbers in our study to explore this theory.
A surprising gap in the data was the lack of any understandable cause of death in six cases. We attempted to find more clinical information from general hospital case notes, but these were either unavailable or did not add to what was on the death certificate. It is possible that some of these deaths may have been related to anorexia nervosa, suicide, or other psychological disturbance, which seemed to be the case in the one which was attributed, rather oddly, to “psychological malfunction arising from mental factors (psychogenic dysmenorrhea).”
Most of the literature has suggested an increased mortality for anorexia nervosa, and this has been well reviewed by others
(1), but there are some studies that have shown no increase in mortality
(2,
7). In the study by Strober et al.
(2), it is of interest that subjects in their cohort were younger at the time they first were seen in a specialist service (between 12 years and 17 years, 11 months) relative to our cohort, which had a mean age at index contact of 19.9 years for the surviving cases and 25.0 years for the cases who died. Naturally, it would be expected that older patients would be at greater risk of death, but it may also reflect delays in seeking treatment of the illness. Also, Strober et al.’s cohort had the benefit of early and intensive treatment, which continued after hospital discharge for most patients. The treatment available to our cohort was, prior to 1994, mostly in general psychiatric and psychological treatment services rather than in an intensive long-term program specializing in the treatment of eating disorders. For many patients in the study of Strober et al., it still took many years to reach full recovery from the illness, but their exposure to treatment may have been a significant factor in lowering mortality. Another study that showed an unexpectedly low mortality was undertaken as part of the Rochester epidemiology project
(7). The possible reasons for the finding of a low standardized mortality ratio are well discussed by Sullivan
(20). In particular, the definition and ascertainment methods used probably identified many milder cases seen in primary care. In contrast most other studies have identified patients seen in specialist services, sometimes highly specialized, tertiary care inpatient settings.
Because the numbers in any mortality study will inevitably be small, it is very difficult indeed to identify predictive factors. The only clear association with mortality in this study was older age at the time the patient was seen in the specialist service. Other possible predictive factors of mortality and poor outcome will be reported in a separate study comparing patients who died or otherwise had poor outcome with those who had a good outcome.
Northeast Scotland provides a unique setting within which it has been possible to study the epidemiology of a large cohort of patients with anorexia nervosa. First, there are case register and other patient administration records dating back to 1965. Second, there is very limited psychiatric practice outside of the National Health Service, and there is a readily accessible National Health Service psychiatric service. In community studies
(21), patients with a definite diagnosis of anorexia nervosa who had not been referred to specialist services are seldom found. While some patients may initially be managed in primary care or referred to general hospital services because they are seen as less stigmatizing than mental health services, the great majority will subsequently be referred to psychiatric services in Northeast Scotland. Third, this study includes all patients seen by specialist services, not just those being admitted for inpatient treatment or only those referred to tertiary referral centers or academic centers, as is the case in many studies
(2,
8,
10–
12,
17). Fourth, the catchment population is well defined. Therefore, this cohort represents a reasonably complete estimate of all patients with anorexia nervosa and consequently a reasonable estimate of the risk of death from anorexia nervosa in a defined catchment population of 580,000.
The findings in this and many earlier studies confirm the medical seriousness of anorexia nervosa. It often runs a chronic course, and our study confirms that death due to anorexia nervosa can occur after many years of illness. Early access to specialist services should minimize delays in diagnosis, and even in those who have been ill for many years, continuing specialist intervention is necessary to try to reduce the risk of death in the long term.