Anorexia nervosa, once thought to occur only in affluent societies, has now been documented across the globe
(1). Although neurobiological factors have been implicated in the emergence of anorexia nervosa, there is evidence to suggest that social factors play an important role as well
(2–
7). The disorder appears to be related to socioeconomic development, changing roles for women, a sociocultural emphasis on thinness, and a shift in eating patterns
(8). Studies have found evidence of changing attitudes about ideal body size and eating patterns accompanying the introduction of television and other methods of merchandizing to increasingly affluent societies
(9).
Curaçao presented a unique opportunity to examine this question. Curaçao is the main island in a group of five islands collectively known as the Netherlands Antilles and is still part of the kingdom of the Netherlands. Like many Caribbean islands, the society has origins in plantation slavery. Curaçao is now one of only a few of these islands to be classified by the World Bank as a high-income country, albeit the least affluent within that grouping. According to the 2001 Curaçao census
(11), 23% of those 15 years and older had no income, compared to 29% in 1992
(12). Dutch and U.S. television is widely available, and other cultural influences of North America and Europe are increasingly evident. Moreover, the island also provided the opportunity to compare incidence across sociocultural groups. Like many transitional societies, Curaçao includes a well-to-do minority subgroup, which adopts many of the cultural norms of affluent societies, as well as a relatively poor majority.
Curaçao is particularly well suited for epidemiological studies. The vast majority of health professionals are trained in the Netherlands. The comprehensive health care system and population databases (modeled on the Dutch systems) made it possible to identify incident cases as well as to compute the denominator for the incidence rate. To our knowledge, the present study is more comprehensive than any previous incidence study on anorexia nervosa.
Method
This study on the incidence of anorexia nervosa was conducted with the approval of the Netherlands Antilles Foundation for Clinical Higher Education, which, in association with Groningen University Hospital in the Netherlands, was responsible for overseeing medical research conducted on Curaçao. All patients interviewed signed informed consent forms.
At the beginning of the study in 1995, Curaçao had a population of 149,963
(13). Census data indicate that in 2001, 82% of the population was born on Curaçao and another 6% on one of the other islands of the Netherlands Antilles
(11). Papiamentu, the local language, was spoken at home in the vast majority (81%) of the households. The official language was Dutch and was used in schools, but it ranked second as a spoken language. The census did not record ethnicity. According to the Curaçao Health Study (N=2,248) in 1993/1994, 79% of the population of Curaçao was identified as black, 13% as mixed, 7% as white, and 1% as Asian
(14). This study also revealed rates of obesity (body mass index >30 kg/m
2) among the Curaçao population in 1993/1994
(15); 18.7% of the Curaçao men were obese, compared to 20.6% of the men in the United States in 1988–1994 and 27.7% in 1999–2000
(16). The obesity rate of 36.2% for Curaçao women was higher than the obesity rate of 25.9% for U.S. women in 1988–1994 and 34% in 1999–2000. The mean body mass index for women on Curaçao is similar to that of black women and much higher than that of white women in the United States (28.3, 28.2, and 26.0, respectively)
(10,
14–16). Of the obese Curaçao women with low socioeconomic status, only half considered themselves to be too fat
(15).
Sources
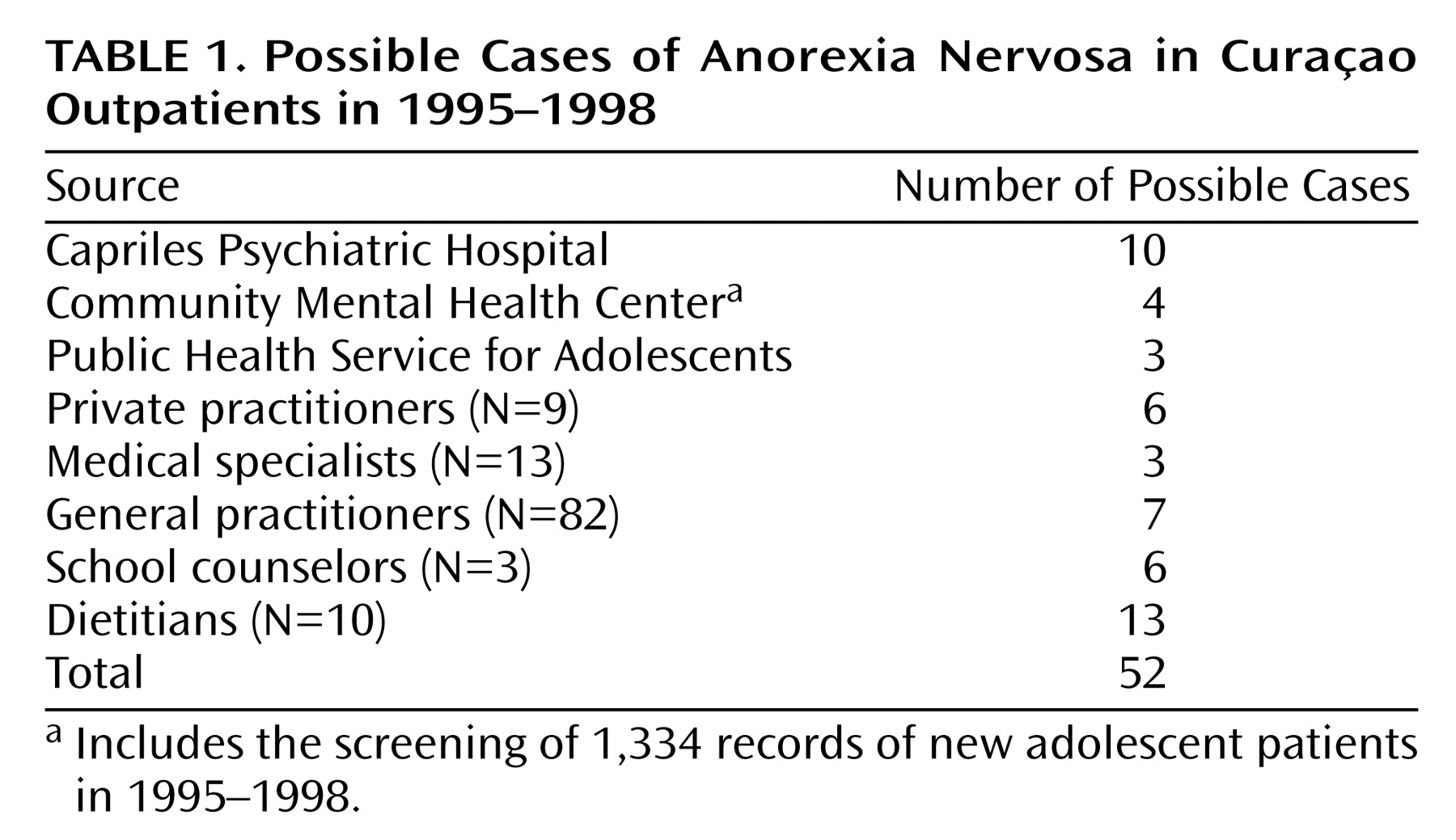
We used both record reviews and personal contacts with service providers to identify “possible” cases of eating disorders. In order to encompass all possible cases, we systematically identified possible cases in both outpatient and inpatient settings. To identify possible cases in outpatient settings, beginning in 1998, we contacted the full range of community health and mental health clinics that might see patients with eating disorders (
Table 1). In addition, we contacted relevant individual health care professionals: all 82 general practitioners, seven of eight psychologists on the island, two psychiatrists with a private practice, seven of eight pediatricians, three gynecologists, and three doctors of internal medicine. All 10 practicing dietitians were willing to provide information. We also informed the three school counselors at the higher grade schools we could find on the island about the study. One of them was a graduate-level psychologist with an official counseling function at the University College of Netherlands Antilles on Curaçao, and the other two were teachers with additional tasks as counselors.
We provided all sources with systematic information about eating disorders and asked them to inform us about any possible cases first seen during 1995–1998. We defined “possible” cases in accordance with a previous general practice study in the Netherlands
(17) and communicated this definition in writing and in person when feasible.
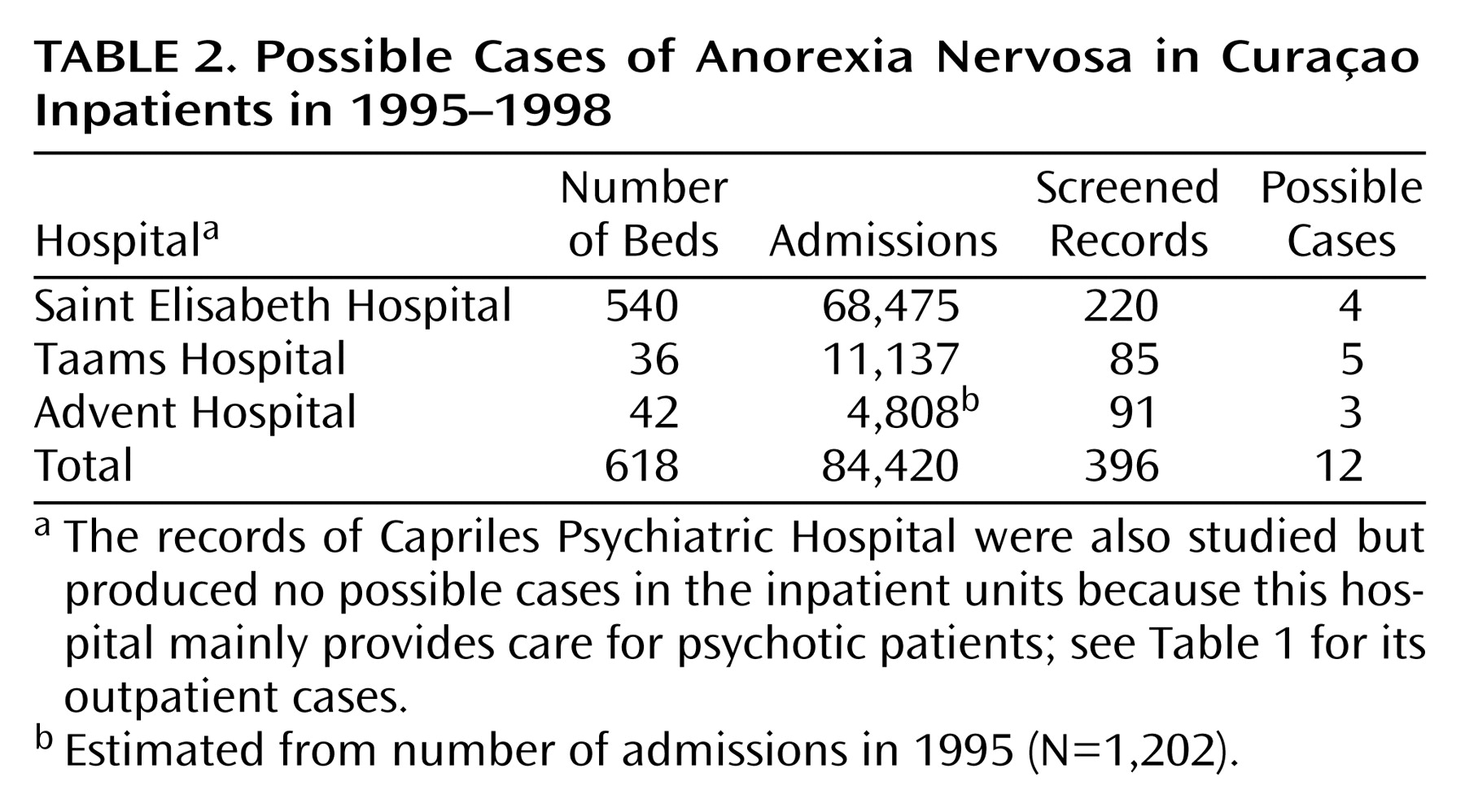
With respect to inpatients in the three existing Curaçao general hospitals, we reviewed the records of all admissions to the Curaçao Saint Elisabeth Hospital and the two smaller private general hospitals for the period 1995–1998 (
Table 2). We screened these records for an ICD-9 diagnosis of an eating disorder, as well as for 26 diagnostic terms that might indicate missed cases. These diagnostic terms were the same as those used in our previous study
(10) and by Lucas and colleagues
(18) in the United States and relate to weight loss, vomiting, or other gastrointestinal problems or menstrual problems. If any of these diagnostic terms had been used on a patient’s chart, an eating disorder expert from the research team (K.M.E.H. or H.W.H.) reviewed the chart, and if the record suggested any symptom or sign of an eating disorder, then it was a “possible” case.
Patients
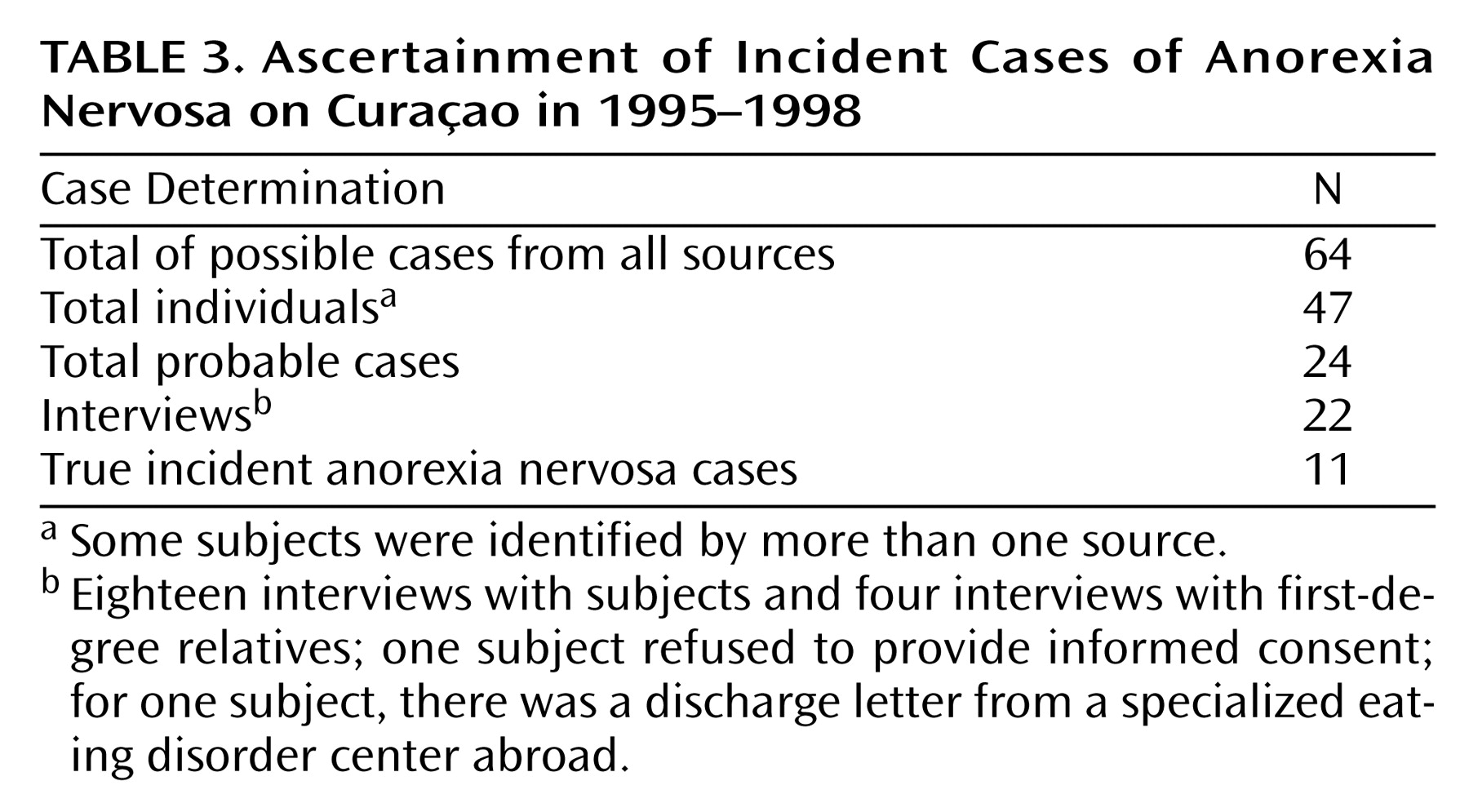
Using this method, we identified 52 outpatients and 12 inpatients (
Table 1 and
Table 2) as “possible” cases, representing 47 individuals (some patients were identified by more than one source). The sources and other physicians involved were contacted and interviewed to determine which of these 47 were “probable” cases. A probable case was one for which there was suggestive evidence that the case might meet the diagnostic criteria of DSM-IV for an eating disorder. Such cases were verified as having been first detected in 1995–1998. Twenty-four cases met these criteria.
With regard to the 24 probable cases, health care professionals located the subjects and obtained their written informed consent for our team to conduct a diagnostic interview. One subject did not give informed consent and was not included in the study. Another woman could not be traced, but the physician was able to provide detailed information. Of the remaining 22 probable cases, 18 subjects could be interviewed in person; the other four subjects were living abroad, but it proved possible to interview a first-degree relative for each of the four on Curaçao.
After written informed consent had been obtained, the subjects were extensively interviewed and assessed by trained interviewers, according to the eating disorders section of the Structured Clinical Interview for DSM-IV (SCID)
(19). In addition to the SCID items, we used further assessments developed by the authors as an aid to eliciting the information required for diagnosis. Current weight and height were measured in a standardized way with the official hospital scales. The body mass index at the time of detection has been based on weight and height data from medical records. Eating disorder experts from the research team (H.W.H., K.M.E.H., and M.A.K.) conducted the diagnostic interviews. The research interviewer made the diagnosis, but in all cases in which there were uncertainties, the case was discussed or reinterviewed by another researcher, and the final diagnosis was a consensus diagnosis arrived at by two members of the research team. For the four probable cases that could not be directly assessed, we reviewed all available information and made a consensus diagnosis.
Data Analysis
The denominators for the incidence rates for anorexia nervosa and 95% confidence intervals (CIs) were computed for the total population (605,708 person-years in 1995–1998) as well as for females (320,651 woman-years) and the high-risk group of females ages 15–24 years (40,041 woman-years). These denominators were provided by the Central Bureau of Statistics, which computed their data based on the census in 1992
(12) and 2001
(11) and the migration rates
(13). Since the census data are not reported by race, to obtain the denominator for mixed/white race incidence, we multiplied the denominator for total incidence by the proportion that was mixed/white according to the Curaçao Health Study
(15).
Results
Based on the interviews and the case records, we identified 11 incident cases fulfilling the DSM-IV criteria for anorexia nervosa and first detected in the study period 1995–1998 (
Table 3). Six other possible cases were not included in the study because the diagnosis in three cases had been considered before 1995 and in three others for the first time in 1999.
Four of the 11 incident cases of the study period were the restricter type of anorexia nervosa and seven the purging type. All subjects had serious weight loss; their mean body mass index at the time of detection was 15.2 kg/m2 (range=12.0–18.2). By definition, all subjects had amenorrhea (one of the criteria in DSM-IV).
All 11 were female. Two of the patients were white and were born in the Netherlands. The other nine were of mixed race; there were no cases among blacks. The cases were 15, 18, 20, 22, 23, 24, 24, 26, 27, 27, and 39 years old at the time of detection. At the time of onset, nine of the subjects were ages 13 to 22; for one, the age at onset was unknown, and one was reported to be 36 at the time of onset.
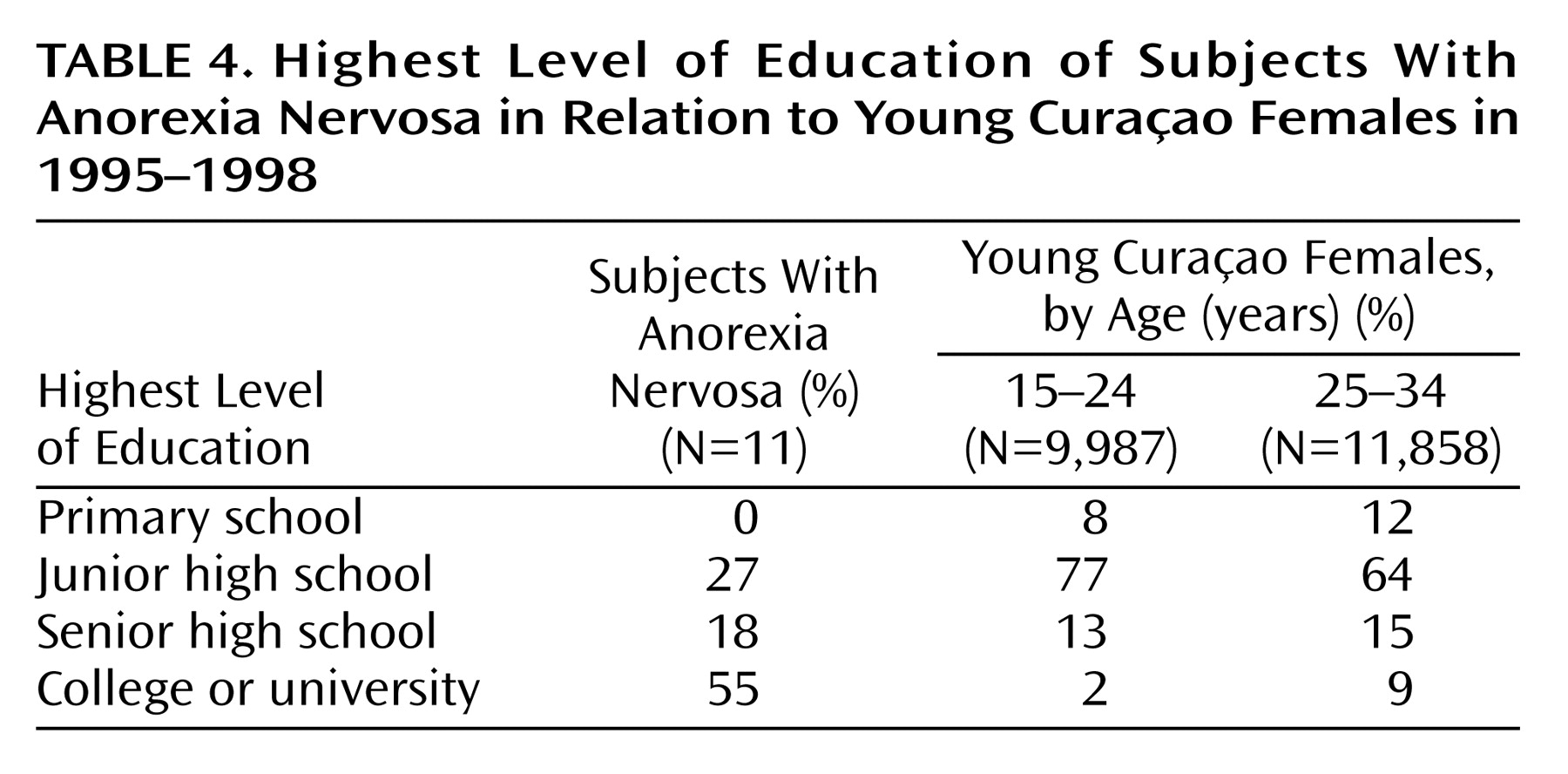
Table 4 shows that 55% of the women with anorexia nervosa had been to college; according to the Central Bureau of Statistics, less than 10% of all Curaçao women in their age group had been to college
(12). At the time of the interview, seven of 11 subjects (64%) earned more than 3,000 Netherlands Antilles florins ($1,695 U.S.) per month. According to the 2001 census, only 0.6% of all 15–24-year-old and 10.9% of all 25–34-year-old females on Curaçao earned more than 3,000 Netherlands Antilles florins. In addition, all subjects had been abroad for a year or more; three had been to the United States and eight to the Netherlands. For seven of the subjects with anorexia nervosa, the stay abroad was before the onset of anorexia nervosa; for one, the stay abroad was after the onset; and for three, this could not be determined.
The associated incidence rates per 100,000 person-years for anorexia nervosa on Curaçao were 1.82 (95% CI=0.74–2.89) for the total population, 3.43 (95% CI=1.40–5.46) for females, and 17.48 (95% CI=4.13–30.43) for the high-risk group of 15–24-year-old females. The associated incidence rates per year per 100,000 person-years for anorexia nervosa for the Curaçao mixed and white populations only were 9.08 (95% CI=3.71–14.45) for the total mixed/white population and 17.15 (95% CI=7.02–27.29) for mixed/white females.
Discussion
This study examined the incidence of anorexia nervosa in a society undergoing a socioeconomic transition. There were two main findings. First, the overall incidence rate for anorexia nervosa of 1.82 per 100,000 person-years on Curaçao is several times lower than in the United States (8.3 per 100,000)
(18) and the Netherlands (8.1 per 100,000)
(17). Also, the overall incidence rate of 17.5 per 100,000 person-years for the high-risk group of 15–24-year-old females is much lower than in the United States (48.4 per 100,000)
(18) and the Netherlands (55.5 per 100,000)
(17).
Second, we did find that sociocultural differences within the island were related to anorexia nervosa. Cases occurred only among the minority white and mixed-race populations. There were no cases among the majority black population, despite our comprehensive case-finding methods. The incidence of anorexia nervosa among the white and mixed-race Curaçao population (9.1 per 100,000 person-years) was similar to the incidence in the United States and the Netherlands.
We did not find evidence that socioeconomic transition had caused an emergence of anorexia nervosa. The finding of a low overall incidence rate of anorexia nervosa on Curaçao was contrary to what we had hypothesized. We had theorized that as a result of the socioeconomic transition taking place on the island, the incidence of anorexia nervosa would be approaching that of high-income countries such as the Netherlands. One possible explanation is that the social impact of higher incomes is yet to emerge because profound cultural changes may take two or more generations. A second possible explanation is that the socioeconomic transition has been uneven and incomplete. The World Bank has classified the Netherlands Antilles as a high-income country, but it has a high unemployment rate and other features that make it quite different from the United States or the Netherlands. The third and most likely possibility is that the low overall incidence rate could be explained by sociocultural factors. Such an explanation would be in line with the most intriguing finding: the absence of any cases among the majority black population. In the African-Caribbean population of Curaçao, being overweight is socially more accepted than in the white and mixed populations
(10,
14,
15). The local norms about body size may have enhanced resiliency to sociocultural emphasis on thinness in the media and other influences from the United States and the Netherlands, and this might have served to protect young women in the majority black population from developing anorexia nervosa.
Our findings may be compared with those in a recent prevalence study in the United States
(20) by using a two-stage case-finding method. This U.S. prevalence study found no anorexia nervosa in black women and 15 cases among young white women (lifetime prevalence of 1.5%). In this U.S. prevalence study, on average, the black households had lower family incomes and lower educational levels than the white households. This comparison should, however, be interpreted with much caution, given the differing sociocultural context of Curaçao and the United States.
The high incidence among the white and mixed-race populations—as high as in the Netherlands
(17) and in the United States
(18)—was also remarkable. One factor that may partly explain this result is that the anorexia nervosa cases belong to a high-income subculture that is similar in many ways to that of affluent societies. High-income subcultures within developing countries do sometimes exhibit a health profile that resembles that of developed countries. This phenomenon has been documented for a long time, for example, among whites in South Africa
(21).
Another important contributing factor may be the experience of going abroad. Most of the cases on Curaçao were women who had developed anorexia nervosa after visiting the Netherlands or the United States (usually as students). This parallels reports of eating disturbances in students moving from a developing to a developed country
(8,
22,
23).
The study has some limitations. First, despite extensive screening, we may have missed cases of anorexia nervosa. In addition, case-detection methods by the health system may have differed for the more affluent white and mixed-race population compared with the majority black population. Because ethnicity is not registered in the population and health registers, we cannot examine possible differences in help-seeking behavior or clinician bias toward the different ethnic subgroups. However, it is unlikely that our results can be explained by the failure to detect cases among the majority black population. All socioeconomic classes have access to health care, regardless of ability to pay. Cases of bulimia nervosa and binge eating disorder were detected among black women in the course of the anorexia study. It seems implausible that cases of anorexia nervosa were missed, while other eating disorders—that are usually harder to detect
(24)—were identified. Although clinician bias cannot be ruled out, clinicians received extensive written and oral information on the study. Because four of the authors currently or previously worked on the island, they were familiar with most physicians on the island. Furthermore, health care workers were alerted to the topic after a British Broadcasting Corporation documentary reported on an earlier investigation of anorexia nervosa on Curaçao
(10).
A second limitation, as in all other incidence studies on anorexia nervosa so far, is that we relied mainly on health care providers. The research team trained and educated health care professionals to improve identification and services on the island. The inclusion of health care providers was more comprehensive than in any previous study, and we made an attempt to include cases from three school counselors. We were able to trace some possible cases at higher grade schools. However, we had no sources in primary or secondary schools. To study possibly undetected cases in all Curaçao schools or among the general population would require an additional comprehensive two-stage study with a screening phase and clinical interviews of a large sample.
A third limitation is that in the absence of census information on ethnicity data, we could not examine differences in income and education between the anorexia nervosa cases and the population within the mixed-race group. We compared the income and education of the cases with that of all persons of the same sex and age group in the census data.
We conclude that the socioeconomic transition on Curaçao was not sufficient for the emergence of anorexia nervosa among the majority black population. The incidence among the minority mixed and white population on Curaçao is similar to the incidence in affluent societies as the United States and Western Europe. In contrast to earlier work
(10) done on Curaçao that did not include interviews, the current results underscore the powerful role of the sociocultural context in the development of anorexia nervosa
(25). It is nonetheless compatible with a neurobiological basis for the development of the disorder in individuals
(2,
3,
26,
27). One possibility is that the development of anorexia nervosa in most cases requires a combination of a sociocultural environment, which imposes stress on eating behaviors and an individual vulnerability that patterns the response to stress.