Many randomized, controlled trials have examined psychological therapies for adults with eating disorders, most commonly bulimia nervosa. Cognitive behavior therapy has been established as the treatment of choice for bulimia nervosa
(1). Interpersonal psychotherapy may also be an effective treatment in this group
(2), although improvement is less rapid than with cognitive behavior therapy. There is evidence that these specialized psychotherapies are superior to other forms of psychotherapy
(3).
Anorexia nervosa is a serious illness with substantial morbidity
(4) and a mortality rate of approximately 5% per decade
(5). Outpatient therapies are widely used in its treatment. However, few randomized, controlled trials have examined treatments for anorexia nervosa. Favorable results have been achieved by using family-based interventions with adolescents
(6,
7). While some studies with adults have shown that specialized psychotherapies are superior to no treatment
(8) or to a control condition of “routine” treatment
(9), others have found no difference between two or more treatments
(10,
11). The specific therapies studied include cognitive behavior therapy
(11,
12), focal psychoanalytic psychotherapy
(9), cognitive analytic therapy
(9,
10), dietary counseling
(12,
13), individual supportive therapy
(14), and family therapy
(9,
14). Taken together, these studies have not demonstrated clear superiority of any specific therapy for anorexia nervosa. More trials are needed, given the dearth of studies and the known difficulties with recruitment and retention of patients with this disorder
(15).
Cognitive behavior therapy is a theoretically relevant treatment for anorexia nervosa
(16,
17) with some evidence of effectiveness
(17,
18). Although interpersonal psychotherapy has not been the focus of clinical trials in anorexia nervosa, the condition is readily conceptualized within the framework of interpersonal psychotherapy
(19). In order to examine the effectiveness of these two psychotherapies in treating anorexia nervosa, we compared them with a control treatment called “nonspecific supportive clinical management.” This treatment provided education and nutritional advice and used supportive psychotherapy principles in responding to the patient. It was hypothesized that the two specialized psychotherapies would be more effective than nonspecific supportive clinical management.
Method
Participants
The inclusion criteria for this study were female gender, an age of 17–40 years, and the presence of current primary anorexia nervosa; the participants included individuals diagnosed according to the DSM-IV weight criterion (body mass index, <17.5), which was considered to be a strict definition of anorexia nervosa, and those diagnosed according to a lenient weight criterion (body mass index, 17.5–19.0)
(20). Individuals with a body mass index below 14.5 were considered unsuitable for outpatient psychotherapy and were referred for assessment at an inpatient unit. In light of debate as to the necessity of amenorrhea in diagnosing anorexia nervosa
(21), amenorrhea was not an inclusion requirement.
The exclusion criteria were current severe major depression, psychoactive substance dependence, major medical or neurological illness, developmental learning disorder, cognitive impairment, bipolar I disorder, schizophrenia, or a chronic, refractory course of anorexia nervosa. Individuals receiving a stable dose of a psychotropic medication with no change in anorexia nervosa symptoms were included; however, only two individuals were taking an antidepressant medication.
Recruitment was broad-based and included referrals from health professionals, self-referrals, and family referrals. The study received ethical approval from the Southern Regional Ethics Committee, and written informed consent was obtained.
Procedure
The structured assessment consisted of the Structured Clinical Interview for DSM-IV
(22) to determine the presence of axis I disorders, the Hamilton Depression Rating Scale
(23), the Eating Disorder Examination
(24), the Global Assessment of Functioning (GAF) (DSM-IV, p. 32), and additional questions relating to eating and weight history, previous treatment, and demographic variables. For the primary outcome measure we developed a global anorexia nervosa measure using a four-point ordinal scale: 4=meets full criteria for the anorexia nervosa spectrum, 3=not full anorexia nervosa but having a number of features of eating disorders, 2=few features of eating disorders, and 1=no significant features of eating disorders.
The participants completed self-report questionnaires, including the Eating Disorder Inventory—2
(25). Physical measurements were made and included height, weight, and percentage body fat. The participants were seen by the team’s dietician for one or two sessions before commencing therapy.
Therapies
Therapy in each modality consisted of 20 hour-long manual-based sessions conducted over a minimum of 20 weeks. The therapists (including V.V.W.M, J.J., and S.E.L.) were experienced in treating individuals with eating disorders. All therapists delivered all three psychotherapies.
Cognitive behavior therapy
Cognitive behavior therapy for anorexia nervosa is based on the premise that the core features of anorexia nervosa, food restriction and avoidance, become entrenched habit patterns, independent of the circumstances that initiated them
(26). Phase one of therapy introduced cognitive behavior therapy and its rationale and the core techniques of self-monitoring and homework. The patient’s motivation to engage in treatment was evaluated, and her ambivalence about giving up anorexia nervosa was addressed. Normal eating was prescribed, and a weight range goal was negotiated. In phase two the patient learned the cognitive behavior therapy skills of challenging dysfunctional thoughts and thought restructuring. Psychoeducational material was provided as take-home handouts. Phase three prepared the patient for termination, providing information on relapse and recovery and teaching strategies to reduce the risk of relapse.
Interpersonal psychotherapy
Interpersonal psychotherapy for anorexia nervosa was based on interpersonal psychotherapy for both depression
(27) and bulimia nervosa
(28). First, a history was taken of the patient’s life events, interpersonal relationships, and eating problems, and links among these were highlighted. Major problems were identified within the four interpersonal psychotherapy problem areas of grief, interpersonal disputes, role transitions, and interpersonal deficits. The second phase focused on the identified problem(s). In interpersonal psychotherapy for depression, each session includes an assessment of symptoms in order to make links between interpersonal issues and depressive symptoms. Fairburn’s interpersonal psychotherapy for bulimia nervosa
(28) avoided discussion of bulimia nervosa symptoms. In the present study the patient’s presentation of eating disorder symptoms was used to facilitate work on the agreed interpersonal problem, but a systematic symptom review was not conducted. The final termination phase prepared the patient for independent coping.
Nonspecific supportive clinical management
Nonspecific supportive clinical management was developed for the present study, and its aim was to mimic outpatient treatment that could be offered to individuals with anorexia nervosa in usual clinical practice. It combined features of clinical management
(29) and supportive psychotherapy
(30). Clinical management includes education, care, and support
(31) and fostering a therapeutic relationship that promotes adherence to treatment. Supportive psychotherapy aims to assist the patient through use of praise, reassurance, and advice. The abnormal nutritional status and dietary patterns typical of anorexia nervosa were central to nonspecific supportive clinical management, which emphasized the resumption of normal eating and the restoration of weight
(32) and provided information on weight maintenance strategies, energy requirements, and relearning to eat normally. Information was provided verbally and as written handouts. Other therapy content was dictated by the patient, with the therapist constrained to avoid specific strategies or foci of interpersonal psychotherapy or cognitive behavior therapy.
Treatment integrity
The psychotherapy sessions were audiotaped, and three randomly selected audiotapes for each patient were reviewed for adherence to the therapy protocol, which was measured by using an adaptation of the Collaborative Study Psychotherapy Rating Scale
(33). The mean scores for each therapeutic modality were appropriately elevated, relative to the other modalities, on its respective subscale of the Collaborative Study Psychotherapy Rating Scale, indicating satisfactory adherence to therapy
(34).
Assessments
Each participant completed assessments after her 10th therapy session and after her final session. The assessments consisted of physical measurements, body image assessment, self-report questionnaires, and a structured clinical interview with a clinician unaware of the participant’s treatment condition. The interview included the global anorexia nervosa measure, Eating Disorder Examination, Hamilton depression scale, and GAF. The patient also completed the Eating Disorder Inventory—2.
Data Analyses
The outcome measures were determined a priori. The primary outcome variable was the global anorexia nervosa rating. Secondary outcome variables addressed aspects of anorexia nervosa as assessed by the Eating Disorder Examination and Eating Disorder Inventory, weight, body mass index, and other physical measures. Tertiary outcome variables addressed overall functioning and symptoms of disorders other than anorexia nervosa, such as depression.
All analyses were performed by using SPSS
(35). Intent-to-treat analyses were conducted by using the last observation carried forward when data were missing for noncompleters.
Values on the global anorexia nervosa measure were compared among treatment groups by using the nonparametric Kruskal-Wallis test. Pairwise comparisons among groups were made by using the Mann-Whitney U test. For secondary and tertiary outcome measures, repeated-measures analysis of variance was used to compare the treatment groups on the change between baseline and the end of treatment. When there was a significant difference among groups, pairwise least significant difference tests were used to compare pairs of means. The independence of the treatment effect from the effects of baseline differences was examined by using logistic regression. The criterion used for statistical significance was p<0.05 in two-tailed tests.
Results
Publicity resulted in over 400 inquiries. Of the 135 individuals who were interviewed, 78 were eligible. Fifty-six of these consented to participate in the study. At randomization the three treatment groups were similar on most measures, except that there were significant differences among the groups in the rates of lifetime comorbid diagnoses of bulimia nervosa and panic disorder. In the cognitive behavior therapy group 63% (N=12) had a lifetime history of bulimia nervosa, compared with 31% (N=5) and 19% (N=4) in the nonspecific supportive clinical management and interpersonal psychotherapy groups. For panic disorder, the lifetime rates were 26%, 19%, and 0% for the groups receiving cognitive behavior therapy (N=5), nonspecific supportive clinical management (N=3), and interpersonal psychotherapy (N=0), respectively.
Of the 56 women randomly assigned to treatment, 35 completed therapy, defined as attending at least 15 of the 20 therapy sessions. Among the 21 women who did not complete treatment, dropouts occurred over the course of therapy; the median number of sessions completed was 7, with a range of 1–14. Four of these participants were hospitalized for weight loss or complications of anorexia nervosa (after completing two, seven, nine, and 12 sessions; three were assigned to interpersonal psychotherapy, and one was assigned to nonspecific supportive clinical management). One hospitalized patient later died, probably from medical complications of anorexia nervosa. Comparing the participants who did and did not complete treatment revealed a significant difference in mean baseline weight (46.9 kg and 45.6 kg, respectively). On all other variables at baseline the two groups were not significantly different. However, the four women who were hospitalized had a lower weight (mean=41.7 kg), percentage body fat, and GAF score than all other participants.
Relationship of Global Outcome to Other Measures
The primary outcome measure was the global anorexia nervosa rating. Participants with a global rating of 4 were minimally improved from baseline in terms of weight, body mass index, and Eating Disorder Examination measures, but they reported lower symptom levels on the Eating Disorder Inventory. Those with a global rating of 3 had gained weight, had minimal changes on the Eating Disorder Examination, and reported considerable symptoms on the Eating Disorder Inventory. Those with a global rating of 2 were much improved. Those rated as 1 reported minimal symptoms on the Eating Disorder Inventory and were rated as having minimal symptoms on the Eating Disorder Examination.
Primary Outcome
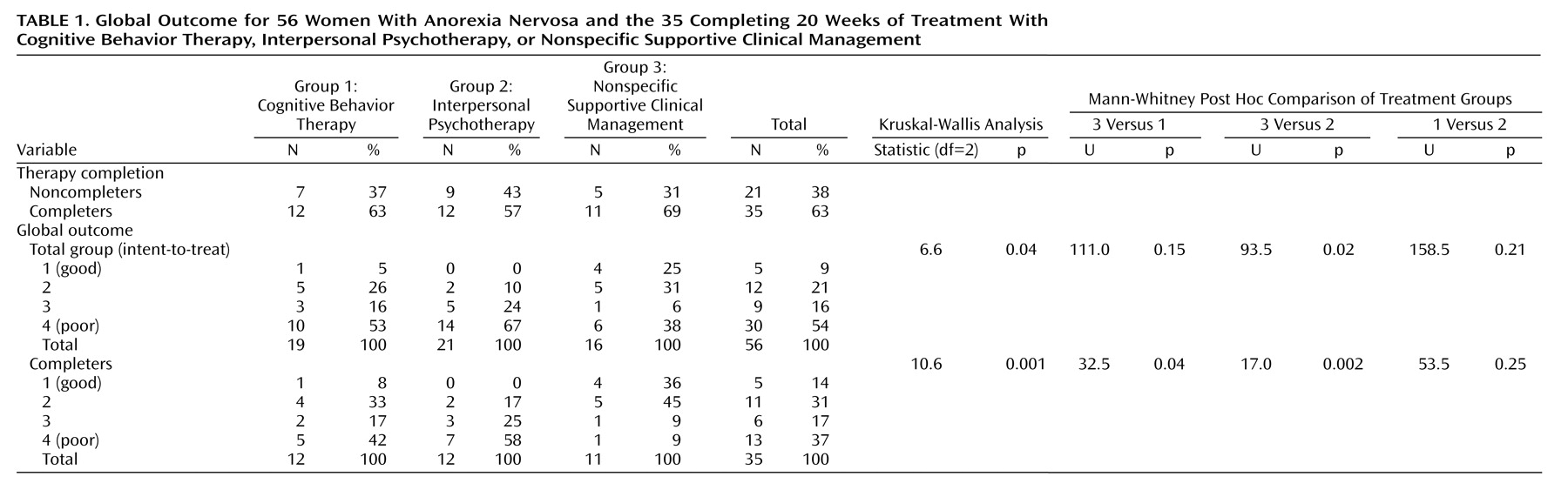
Primary outcome data are shown in
Table 1. The percentages of individuals completing therapy and the time to discontinuation for the three therapeutic modalities were not significantly different. The main reasons for discontinuing treatment also did not differ across the three therapy groups: one subject from each group moved from the area, four improved (cognitive behavior therapy, N=1; interpersonal psychotherapy, N=2; nonspecific supportive clinical management, N=1), seven disliked treatment (cognitive behavior therapy, N=3; interpersonal psychotherapy, N=2; nonspecific supportive clinical management, N=2), and three stopped coming to treatment sessions and assessments (cognitive behavior therapy, N=2; interpersonal psychotherapy, N=1; nonspecific supportive clinical management, N=0).
Intent-to-treat analyses were conducted by using the last observation carried forward for noncompleters. Patients who dropped out before the midtreatment assessment were given a rating of 4, and the rating from the (blind) assessment at midtreatment or end of treatment was used for those who had completed one of these assessments. Significant differences in the primary outcome were found among all participants across therapies. Mann-Whitney U tests showed that nonspecific supportive clinical management was superior to interpersonal psychotherapy. Cognitive behavior therapy and interpersonal psychotherapy did not differ significantly from one another, nor did cognitive behavior therapy and nonspecific supportive clinical management. For the total study group, a global rating of 1 or 2 was achieved in two (10%) of the 21 patients receiving interpersonal psychotherapy, six (32%) of the 19 receiving cognitive behavior therapy, and nine (56%) of the 16 assigned to nonspecific supportive clinical management.
There were significant differences in primary outcome among completers across therapies. Mann-Whitney U tests showed that nonspecific supportive clinical management was superior to cognitive behavior therapy and to interpersonal psychotherapy, while cognitive behavior therapy and interpersonal psychotherapy did not differ significantly from one another. Among those completing therapy, a global rating of 1 or 2 was achieved in two (17%) of the 12 interpersonal psychotherapy patients, five (42%) of the 12 patients completing cognitive behavior therapy, and nine (82%) of the 11 receiving nonspecific supportive clinical management.
Secondary and Tertiary Outcomes
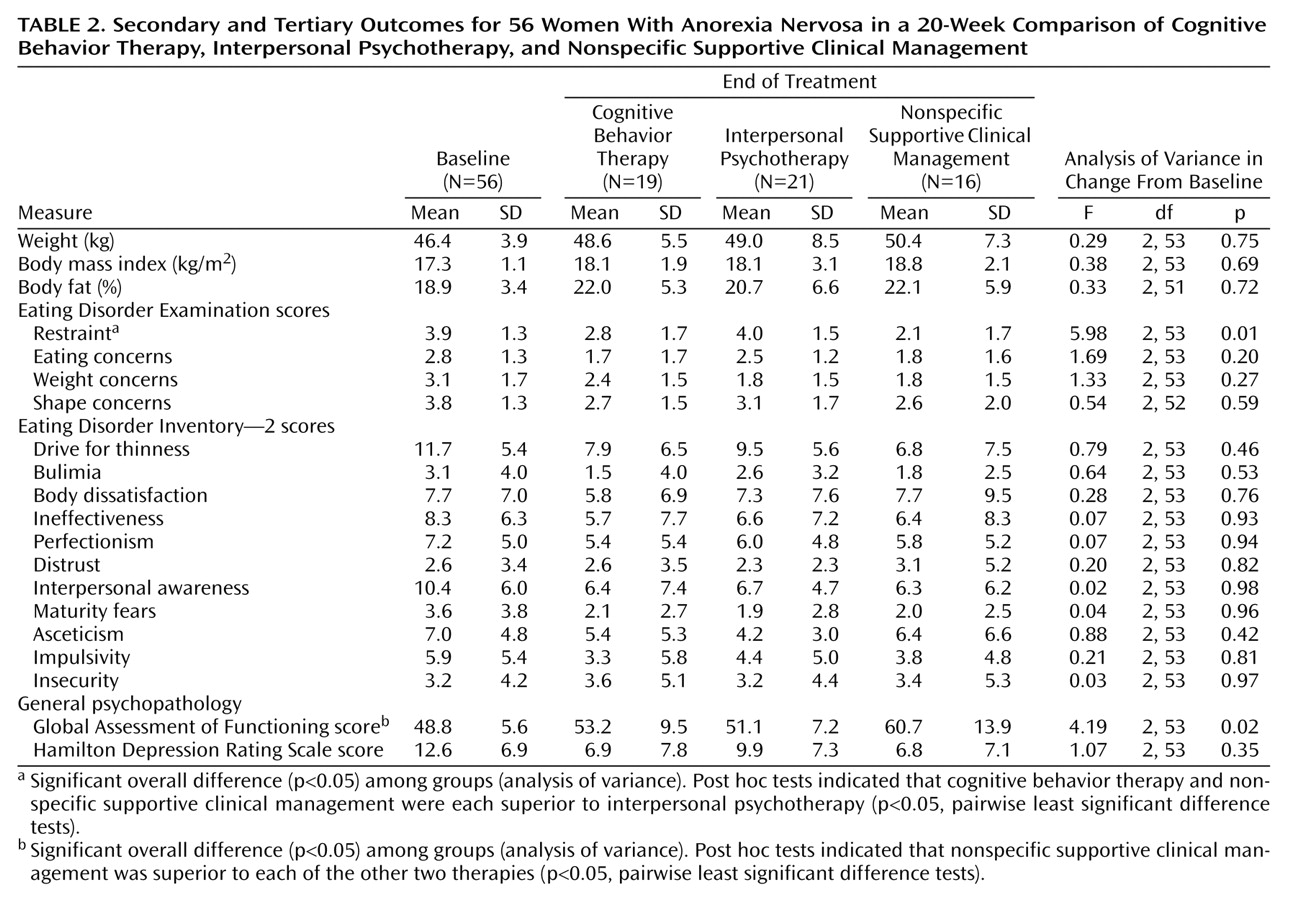
Table 2 shows mean values for the secondary and tertiary outcome measures at the end of treatment for the total study group. There were no significant differences by therapy on any of the physical measures, including weight, body mass index, and percentage body fat. On the Eating Disorder Examination restraint subscale, cognitive behavior therapy and nonspecific supportive clinical management were both superior to interpersonal psychotherapy and did not differ from one another. On the GAF, nonspecific supportive clinical management was superior to both cognitive behavior therapy and interpersonal psychotherapy, which did not differ from one another.
For those completing therapy, there was no difference by therapy group on weight outcome. There were significant differences on all four Eating Disorder Examination subscales and on the drive for thinness subscale of the Eating Disorder Inventory. For restraint and shape concerns (Eating Disorder Examination) and drive for thinness (Eating Disorder Inventory), post hoc tests showed that nonspecific supportive clinical management was superior to interpersonal psychotherapy, while for eating concerns and weight concerns (Eating Disorder Examination), both nonspecific supportive clinical management and cognitive behavior therapy were superior to interpersonal psychotherapy. On the GAF, nonspecific supportive clinical management was superior to both other treatments, which did not differ from one another.
Confounding Factors
Logistic regression was used with a dichotomized form of the global anorexia nervosa rating as the dependent measure to examine whether differences in outcome among therapy groups could be explained by baseline differences (p<0.10) among treatment groups. The analyses were conducted with treatment as a binary comparison (cognitive behavior therapy or interpersonal psychotherapy versus nonspecific supportive clinical management) and as a three-way comparison. Differences in outcome among the treatment groups were not explained by any difference among treatment groups at baseline (p=0.050 for the binary comparison, p=0.033 for the three-way comparison).
Discussion
To our knowledge, this study is the first randomized, controlled trial to compare cognitive behavior therapy and interpersonal psychotherapy with nonspecific supportive clinical management for adults with anorexia nervosa. At the end of treatment, 9% of the subjects had a very good outcome and a further 21% had improved considerably; 70% either did not complete treatment or made small or no gains. Contrary to our hypotheses, the patients who received nonspecific supportive clinical management had an outcome as good as or better than the outcomes of those who received specialized psychotherapies, with 56% of the participants who received nonspecific supportive clinical management given a global rating of 1 or 2, compared with 32% and 10% of those receiving cognitive behavior therapy and interpersonal psychotherapy, respectively. On a number of secondary outcome measures, the outcomes for cognitive behavior therapy were intermediate between the results for nonspecific supportive clinical management and interpersonal psychotherapy.
Inclusion of patients in the lenient weight range resulted in a study group that differed from the subjects in many other studies. However, the subgroups based on strict and lenient weight criteria were indistinguishable on almost all measures of severity at baseline
(20), and inclusion of strict/lenient as a covariate in the logistic regression did not explain the differences in outcome across therapies.
Other methodological issues include the relatively short duration of therapy and the relatively small number of subjects. Although the study group was smaller than the groups in clinical trials for bulimia nervosa or major depression, in the eight existing randomized, controlled trials for adults with anorexia nervosa of which we are aware
(8–
12,
14,
18,
36), the numbers of subjects were modest (range=24–90, mean=50.7, median=34.0), reflecting difficulties with recruitment and retention, both of which are features of anorexia nervosa trials
(15). These methodological limitations, however, would not account for the differential treatment outcome. Further, the differences among the treatment groups in rates of comorbidity were not found to contribute to the differential treatment outcome.
Interpersonal psychotherapy was the least effective of the three therapies. Possible explanations include the relative lack of symptom focus, the relatively long time taken to decide on the problem area, thus reducing the length of the middle phase of interpersonal psychotherapy, and the lack of reactivity of the symptoms of anorexia nervosa to interpersonal triggers, which may hinder exploration of links between interpersonal issues and eating disorder symptoms. Interpersonal events may be less rewarding for or more avoided by anorexia nervosa patients, and thus a personal rationale for interpersonal psychotherapy may be missing for this patient group at this stage of illness. However, we found no difference across the three therapies in patients’ ratings of treatment credibility or satisfaction, indicating that differences in how patients perceived the three therapies did not account for the differences among therapy groups. Therapy had a relatively early focus on affect and interpersonal functioning, which may be difficult for anorexia nervosa patients.
Possible reasons for poor outcomes with cognitive behavior therapy include the large amount of psychoeducational material and extensive skills acquisition, inability to generate alternatives to fixed cognitions stemming from the cognitive rigidity of anorexia nervosa patients, and the ego-syntonic nature of anorexia nervosa, causing difficulty in actively working toward change in a direct therapy, such as cognitive behavior therapy. Cognitive behavior therapy may be less effective for patients with anorexia nervosa, who have high rates of obsessional personality traits
(37), as has been found in depressed patients
(38). It may be more effective after an initial weight gain.
It may be, however, that nonspecific supportive clinical management is a particularly suitable treatment for acute anorexia nervosa. Both clinical management and supportive psychotherapy have been found to be highly effective treatments with other disorders
(39,
40). In this study it was delivered by clinicians experienced with eating disorders, was practiced according to a detailed treatment manual, and included the potentially powerful components of psychoeducation and a focus on normalizing eating (shared with cognitive behavior therapy). Thus, the therapy included detailed discussion of ways to increase food choices and quantities in order to gain weight. As the remaining session content was based on issues the patient chose to present, nonspecific supportive clinical management may allow an increased sense of patient autonomy and control. A key feature of nonspecific supportive clinical management may be the important nonspecific factors of psychotherapy: the therapeutic alliance, empathy, positive regard, and support for a patient group greatly in need of these.
To our knowledge, this is the first comparison of cognitive behavior therapy and interpersonal psychotherapy with a control therapy for adults with anorexia nervosa. Some previous randomized, controlled trials for anorexia nervosa have included aspects of nonspecific supportive clinical management
(9,
11,
13) but with important differences: the therapists were not eating disorders specialists
(9,
11), therapy was disrupted when therapists left the service
(9), and the sessions were shorter and fewer than in the other therapies
(9,
11). In the present study, the proportion of patients with a very good or good outcome (30%) was similar to that in other studies
(9,
10). Hall and Crisp’s comparison of dietary advice and psychotherapy
(13) showed improvement in both groups, with the group receiving dietary advice having greater weight gain.
A stepped approach has been advocated in the treatment of eating disorders
(26), and nonspecific supportive clinical management may be a good first phase of treatment. Further research is needed to identify which patients will respond to a particular first-line treatment. It is not known whether some therapy models are better for some individuals or whether individuals who fail to respond to one therapy will also fail to respond to another therapy model.
In conclusion, the results of the present study caution against assuming that more specialized psychotherapies are necessarily more effective in the clinical management of anorexia nervosa. As this appears to be the first time that nonspecific supportive clinical management has been the subject of a treatment trial for anorexia nervosa, replication of the study is necessary. However, the outcome in the present study indicates that nonspecific supportive clinical management may be a valuable treatment for adults with anorexia nervosa.