Primary Findings
Virtually all research on patients with borderline personality disorder has studied samples from hospital inpatient units or outpatient clinics. This study compared borderline personality disorder patients with dysthymic disorder patients treated in the community to see whether the phenomena observed in prior samples characterize borderline personality disorder patients as treated in the community or whether samples of borderline personality disorder patients from hospitals and university clinics provide an overly pathological portrait of the disorder. The results point to two primary conclusions.
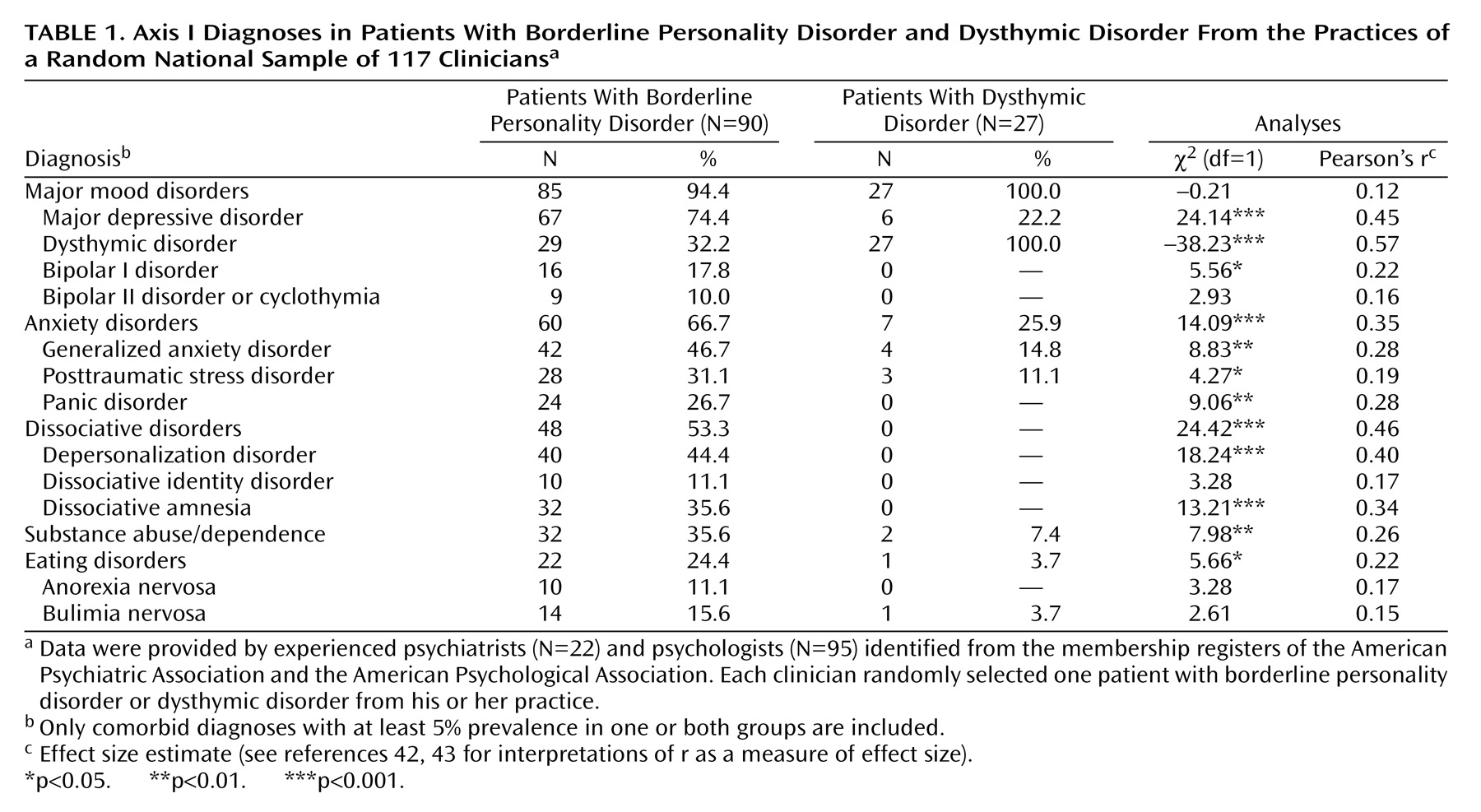
First, the data from prior studies, which could be expected to oversample the more severe end of the borderline spectrum, nevertheless generalized well to the patients seen by randomly selected clinicians across a wide variety of settings. In terms of axis I comorbidity, the borderline personality disorder sample in our study was very similar to other borderline personality disorder samples reviewed by Gunderson
(20), with a profile of high emotional distress (in the form of mood and anxiety disorders, including posttraumatic stress disorder) and problematic ways of managing it (e.g., dissociative disorders, substance abuse, eating disorders). The findings were also consistent with Gunderson’s review of research on axis II comorbidity in borderline personality disorder
(20,
21,
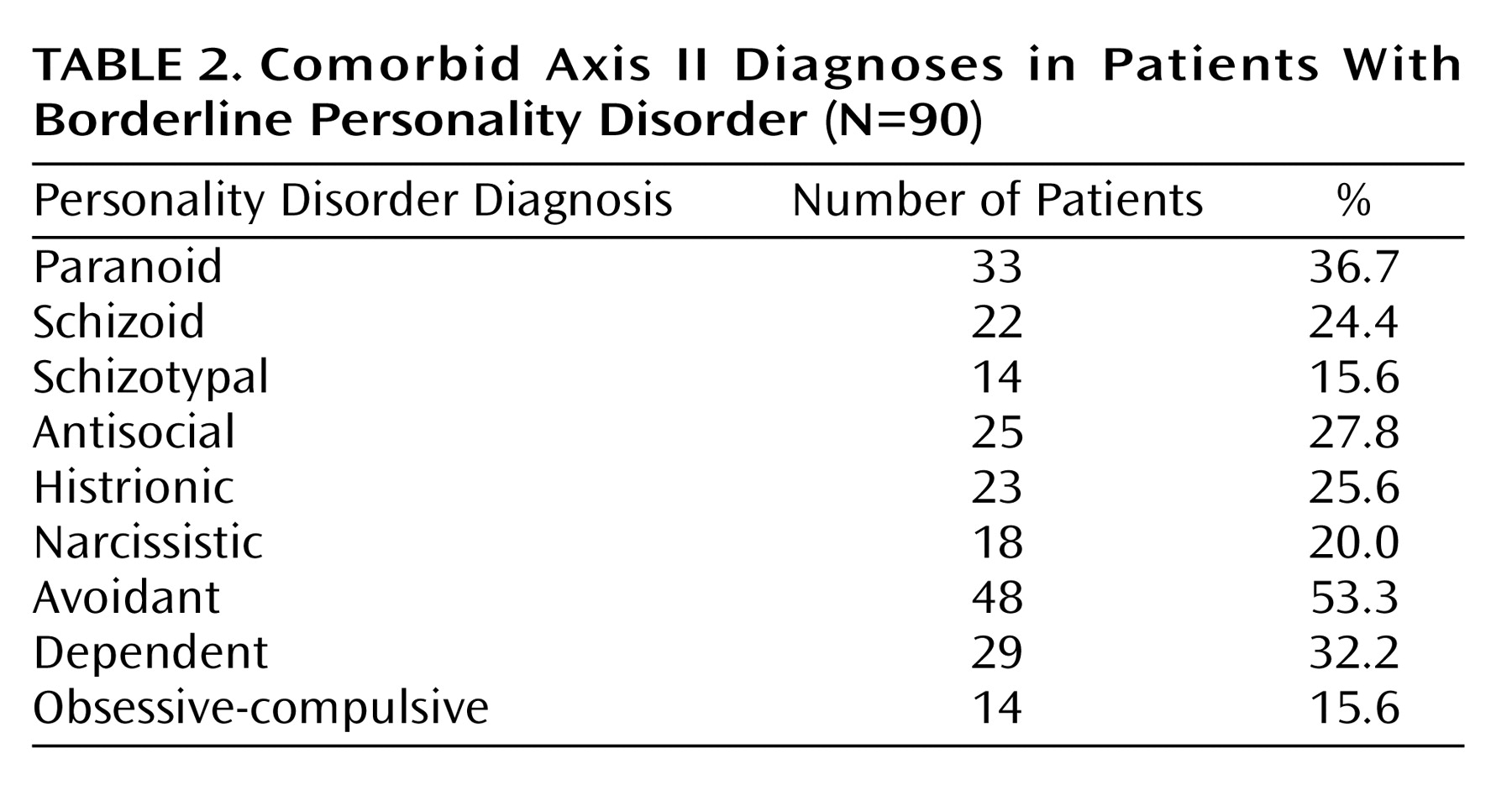
47), in which 90%–97% of borderline personality disorder patients were found to meet the criteria for other DSM personality disorder diagnoses. In our sample, the axis II checklist identified substantial rates of comorbidity for every axis II personality disorder, with particularly high frequencies of avoidant, paranoid, and dependent personality disorders. The slightly higher rates of avoidant and dependent personality disorder diagnoses in this sample may reflect the possibility that the community treatment-seeking sample is more withdrawn and dysphoric than the more acute hospital or university clinic samples or may reflect changes in borderline personality disorder criteria between DSM-III-R and DSM-IV.
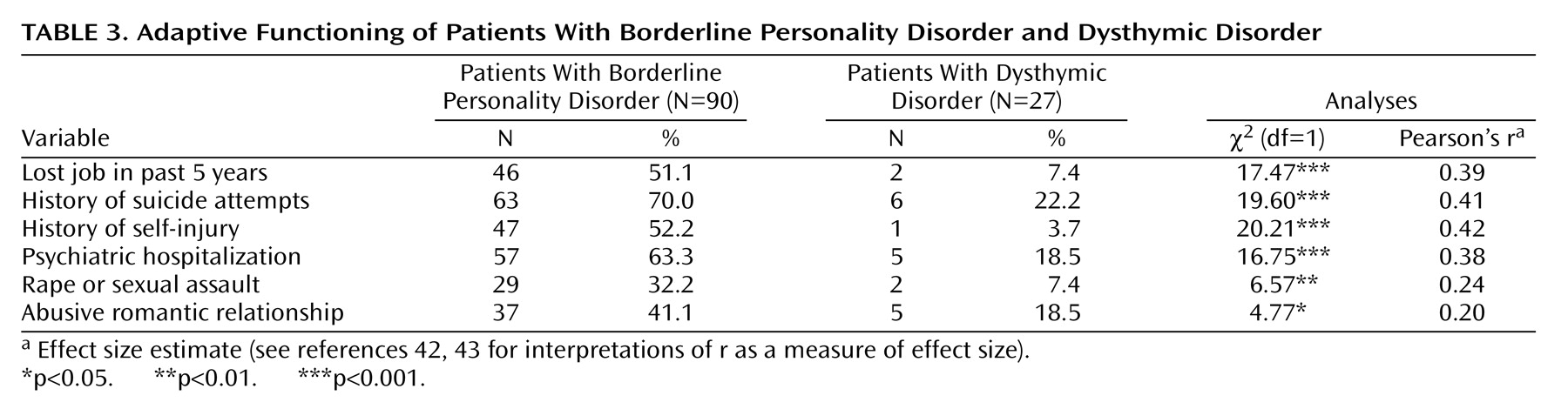
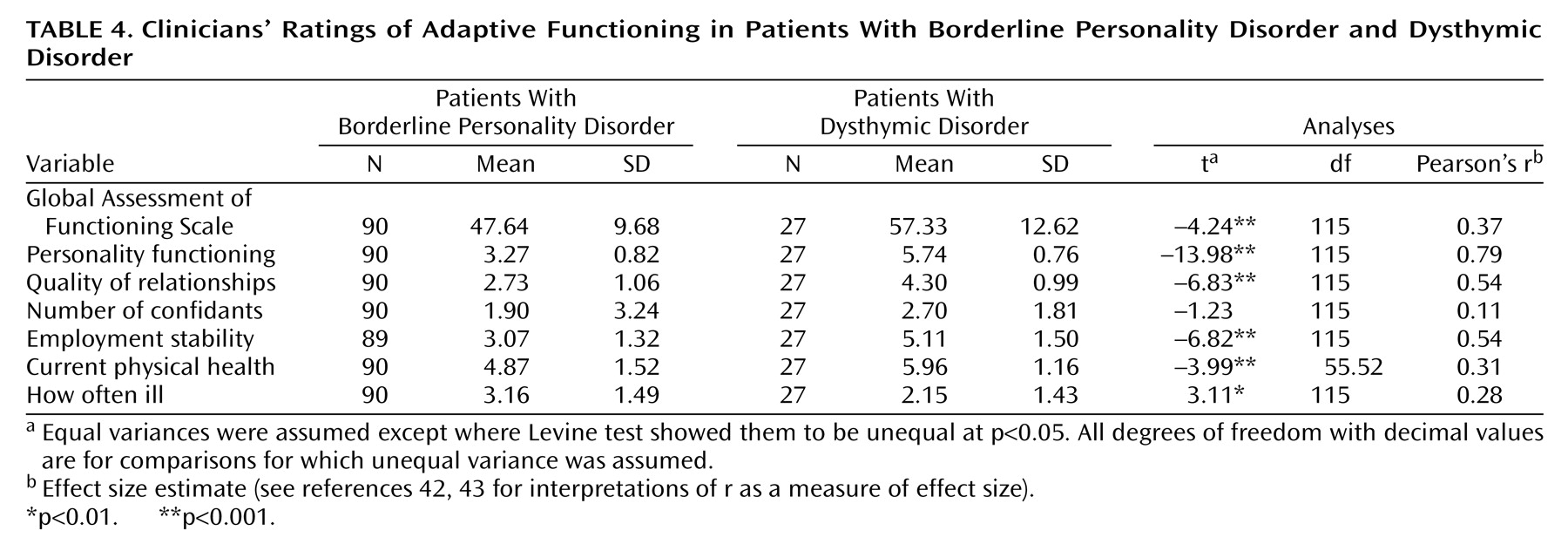
With respect to adaptive functioning, like the borderline personality disorder patients studied in prior investigations, the borderline personality disorder patients treated in everyday practice showed substantial deficits. More than two-thirds had attempted suicide, more than one-half had self-injured (mostly by cutting), and almost two-thirds had been hospitalized at least once. Clinicians reported that borderline personality disorder patients had lower quality of relationships and unstable work histories, with more than one-half having lost a job in the past 5 years because of interpersonal problems.
Of particular interest are findings on physical health and abusive experiences in adulthood, as these areas of functioning have not received as much empirical attention as other aspects of adaptation. Borderline personality disorder patients appeared to have frequent or chronic minor illnesses, leading to missed appointments, days off from work, visits to the doctor, or subjective distress. Forty percent of the borderline personality disorder patients in this sample also had been in abusive relationships in adulthood, with virtually all being victimized (whether or not they also at times perpetrated violence). Nearly one-third of the borderline personality disorder patients had been the victim of rape or other serious sexual assault in adulthood, with such experiences typically occurring multiple times. A recent study by Zanarini et al.
(46) produced similar results.
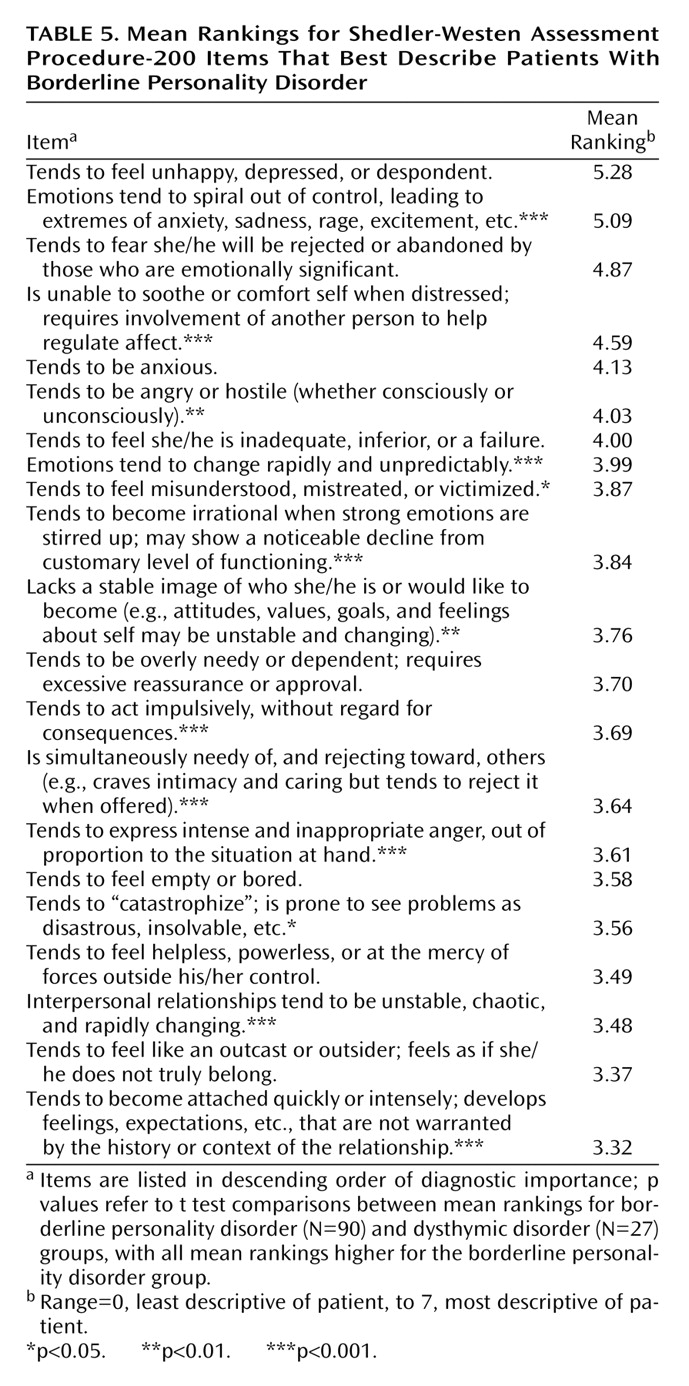
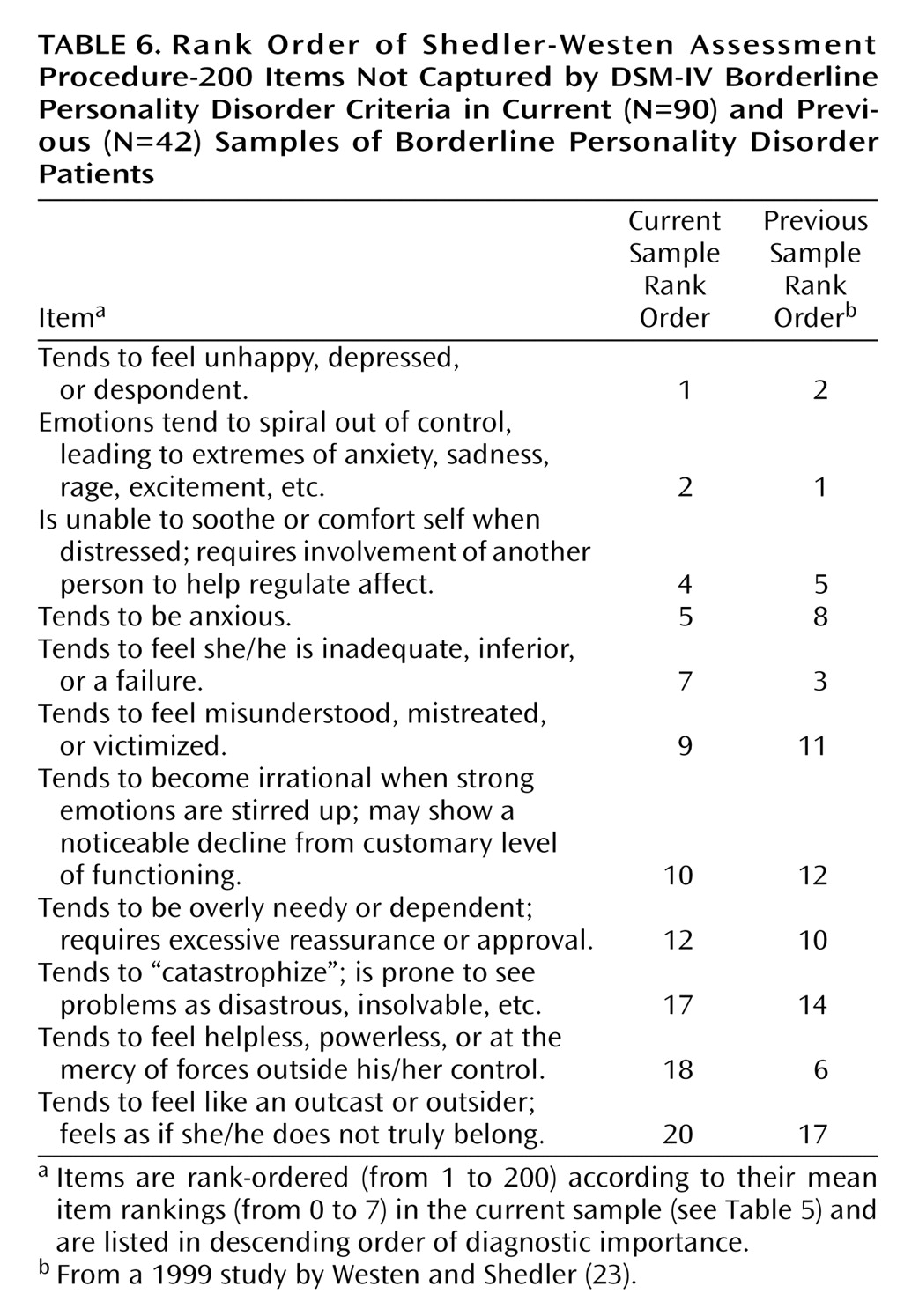
Second, the data provide a portrait of the average patient with DSM-IV-diagnosed borderline personality disorder seen in clinical practice, and this portrait converges with the DSM-IV description in multiple respects but diverges in others. Of the 200 items in the SWAP-200, several designed to reflect DSM-IV diagnostic criteria appeared empirically among the 20 items that were most descriptive of patients who receive a borderline personality disorder diagnosis. These items describe rejection/abandonment fears, unstable relationships, unstable identity, impulsivity, labile emotions, feelings of emptiness or boredom, and intense anger. On the other hand, several DSM-IV criteria were not ranked highly among the SWAP-200 descriptors of actual borderline personality disorder patients, and other items not included in DSM-IV received higher rankings on average than many current criteria.
Among the DSM-IV criteria that did not receive high average rankings were items describing the tendency to see people as “all good” or “all bad” (either because empirically these concepts are not as central to the diagnosis or because splitting them into two items may have decreased the ranking of both) and items describing specific forms of impulsivity, such as alcohol abuse and promiscuous sex. The hybrid criterion added to DSM-IV regarding transient psychotic symptoms and dissociative episodes did not rank highly. However, a related item that ranked tenth in the borderline personality disorder sample better appears to capture an aspect of the construct originally intended by Gunderson
(21) and should be considered as a replacement criterion for DSM-V: “tends to become irrational when strong emotions are stirred up; may show a noticeable decline from customary level of functioning.” Although clinicians reported significant self-injury and suicidality (on the Clinical Data Form), SWAP-200 items for these phenomena did not rank as highly as other items. These differences may reflect a sampling difference between prior studies and the present investigation or may reflect the differential salience of particular high-risk behaviors when reported to an interviewer on a single occasion, typically when the patient is most symptomatic and presents at a hospital or clinic for treatment, versus when the behavior is contextualized within a longitudinal portrait of the patient over time.
Several other SWAP-200 items emerged as more descriptive than some of the current borderline personality disorder criteria, despite the fact that we used DSM-IV criteria to define the patient sample. Perhaps most important was a set of items reflecting chronic (rather than transient) aspects of emotional experience, namely the tendency “to feel unhappy, depressed, despondent” (the item with the highest ranking of all the items in the SWAP-200 composite borderline personality disorder profile) and to feel anxious. These data suggest that DSM-IV may understate the pain and dysphoria borderline personality disorder patients feel. They also support the view that negative affect is a central trait in borderline personality disorder as currently defined
(48,
49).
Another set of items that may not receive adequate representation among the criteria for borderline personality disorder in DSM-IV describes the related trait of emotion dysregulation (on the difference between negative affect and emotion dysregulation, see references
28,
34,
40). These items describe a person whose emotions tend to spiral out of control; who can become irrational when strong emotions are stirred; who tends to “catastrophize,” seeing problems as disastrous and insolvable; and who has difficulty self-soothing and hence may become overly dependent on others to help regulate emotion. These descriptions of emotion dysregulation appear clinically richer and more specific than the DSM-IV description of “affective instability due to a marked reactivity of mood.” All of these items distinguished borderline personality disorder patients from dysthymic disorder patients, who share the trait of negative affect, and occurred at a similarly high rate in previous efforts to develop an empirical prototype of borderline personality disorder
(22).
Limitations and Potential Objections
The data from this study, like the data from a number of studies from our laboratory (e.g., references
22,
25,
27,
29), point to the potential utility of practice research network methods in research on personality disorders. The convergence of multiple informants would clearly be ideal (although most studies of psychopathology rely on a single observer—the patient—by means of either self-report or structured interviews); however, data from experienced clinical observers who interact with the patient over time and hence can provide a longitudinal portrait provide a complementary standpoint to that typically seen in psychiatric research.
Another set of limitations concerns the makeup of the current sample. Psychologists were disproportionately represented in the sample, relative to psychiatrists (80% and 20%, respectively), and the overall response rate was relatively low, compared to our previous studies. Although we cannot be sure that some unknown bias was not introduced by clinicians’ decisions to participate or not participate, the data provided by psychologists and by psychiatrists did not show any pattern of differences in this or any of our prior studies using this method, despite substantially different response rates, and our findings converged with those of research from medical centers that used completely different sampling methods. The similarities in these findings suggest that such biases are not likely substantial. Limiting the study to patients in psychotherapy also introduced the possibility that we were oversampling higher-functioning borderline personality disorder patients. However, the data suggested otherwise: The majority of the borderline personality disorder patients in the study reported histories of psychiatric hospitalizations, suicide attempts, and self-injurious behavior, and their average GAF score (mean=47.64, SD=9.68) indicated serious impairment. Finally, male and non-Caucasian borderline personality disorder patients are understudied groups, and broader sampling, including oversampling to maximize representativeness of the population, would strengthen future investigations.