The stress hormone system has been studied as a mediator of the effects of childhood trauma on psychopathology in preclinical and human studies. The role of corticotropin-releasing factor (CRF) in affective regulation and the stress response makes it a promising candidate for study in disorders such as borderline personality disorder. To our knowledge, no study to date has investigated the relationship between childhood trauma and CSF CRF concentration in subjects with personality disorders.
This study tested the hypothesis that childhood trauma leads to persistent stress hormone abnormalities in adult subjects with personality disorders, as measured by altered CSF CRF concentration.
Method
The subjects were 20 adult men who met DSM-IV criteria for personality disorders. The men underwent a lumbar puncture to measure CSF CRF and completed the Childhood Trauma Questionnaire
(1). Subjects were recruited by newspaper advertisement. Written informed consent was obtained from all participating subjects. Physical health was evaluated by medical history, physical examination, laboratory studies, and electrocardiogram. Semistructured interviews (the Schedule for Affective Disorders and Schizophrenia
[2] and the Structured Clinical Interview for DSM-IV) and best-estimate consensus procedures were used to make axis I and II diagnoses according to DSM-IV criteria. History of childhood trauma was assessed by the self-administered Childhood Trauma Questionnaire. Other behavioral data examined included global functioning (Global Assessment of Functioning Scale [GAF] [DSM-IV, p. 32) and general personality measures (the Tridimensional Personality Questionnaire
[3] and the Eysenck Personality Questionnaire
[4]).
Five subjects had cluster A personality disorders (five paranoid and one schizoid), five subjects had cluster B personality disorders (two antisocial, one histrionic, and two narcissistic), five subjects had a cluster C personality disorder (all five obsessive-compulsive), and nine subjects had a diagnosis of personality disorder not otherwise specified. (Subjects could have more than one personality disorder.)
Five subjects had a history of major depressive disorder, currently in remission. One had a history of dysthymia, and one had current substance abuse. No subjects had a history of bipolar disorder, psychosis, or anxiety disorder. Two subjects had a history of attention deficit disorder, and two had a history of intermittent explosive disorder.
This study used the original 70-item self-report Childhood Trauma Questionnaire
(1), which provides a retrospective assessment of traumatic childhood experiences. Principal components analysis of the Childhood Trauma Questionnaire yields four main factors: physical and emotional abuse, emotional neglect, sexual abuse, and physical neglect
(5).
Five of the 20 subjects had a documented history of past, but not current, treatment with psychotropic agents. All subjects were instructed to remain drug free for 2 weeks and to follow a low monoamine diet for at least 3 days before the study.
Subjects reported to the laboratory at 9:00 p.m. the evening before lumbar puncture. At 9:00 a.m. the next day, subjects completed a visual analogue scale rating subjective mood state. At 10:00 a.m., lumbar punctures were performed under sterile technique. A total of 20 cc of CSF was withdrawn in six aliquots. CSF from the third aliquot was assayed for CRF. All CSF samples were frozen immediately at –70°C until assay. Assays of CRF and ACTH were by radioimmunoassay using reagents provided by IgG Corp. (Nashville, Tenn.). CSF CRF inter- and intraassay coefficients of variability were 11.9% and 7.2%, respectively. ACTH inter- and intraassay coefficients of variability were 11.0% and 7.0%, respectively
(6).
The primary methods of data analysis relied on Pearson product-moment correlations and t tests. All CSF variables were normally distributed. Childhood Trauma Questionnaire total scores were normally distributed, as were the scores on Childhood Trauma Questionnaire subscales, with the exception of sexual abuse. Median split analysis was done to estimate the magnitude of the difference in the study group between subjects reporting categorically high versus low amounts of childhood trauma by Childhood Trauma Questionnaire total score.
Results
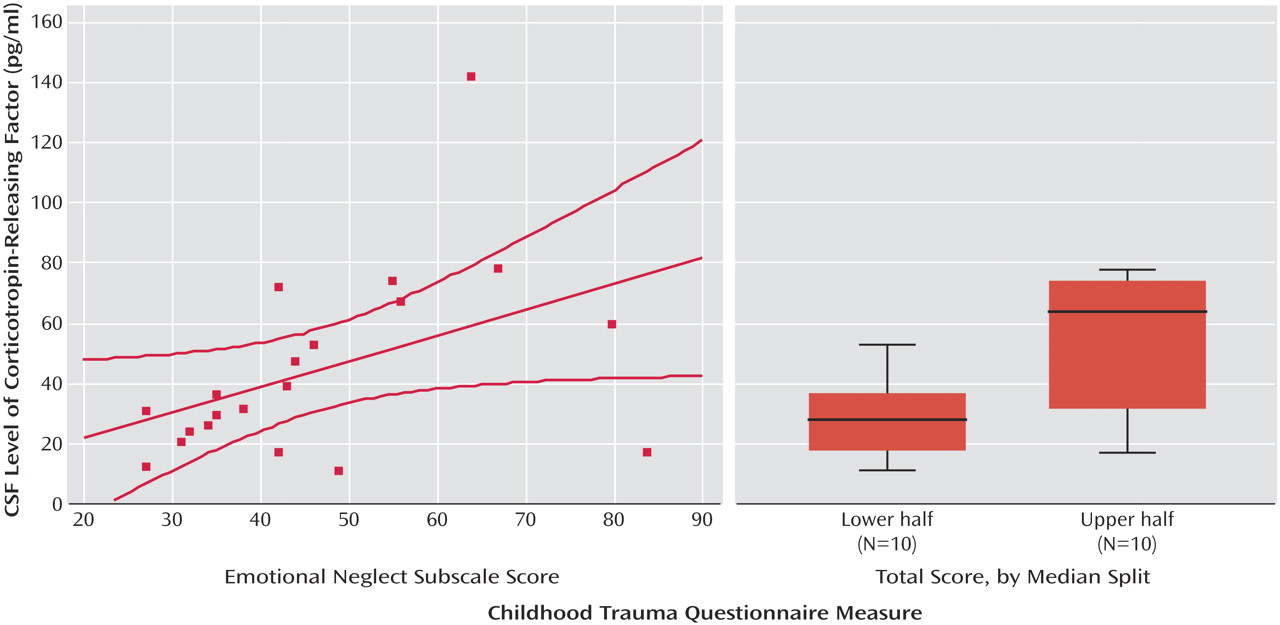
CSF CRF levels were significantly, positively correlated with Childhood Trauma Questionnaire total scores (r=0.48, N=20, p<0.04) (
Figure 1). Median split analysis revealed the same relationship: CSF CRF levels of subjects with scores above the median Childhood Trauma Questionnaire total score were significantly higher than those of subjects with scores below the median total score (mean=60.5, SD=36.3, versus mean=28.5, SD=14.2) (t=2.60, df=18, p<0.03). Subsequent analysis of the four Childhood Trauma Questionnaire subscales revealed a statistically significant positive correlation between CSF CRF levels and emotional neglect (r=0.45, N=20, p<0.05). Correlations between CSF CRF concentration with physical and emotional abuse and physical neglect were smaller in magnitude and not significant (r=0.33, N=20, p=0.15, and r=0.34, N=20, p<0.14, respectively). The relationship between CSF CRF and sexual abuse could not be examined because of the restriction of range in scores for this Childhood Trauma Questionnaire subscale. Age, race, socioeconomic status, and GAF were not correlated with CSF CRF levels or with Childhood Trauma Questionnaire total score.
Despite the fact that the CSF CRF level correlated significantly with CSF ACTH level (r=0.46, N=20, p<0.05), no correlation was noted between CSF ACTH and the total Childhood Trauma Questionnaire score. CSF CRF levels were not correlated with any of the personality variables measured (Tridimensional Personality Questionnaire and Eysenck Personality Questionnaire) and were not correlated with subjective mood states as measured by visual analogue scale.
Discussion
The results of this study reveal a direct correlation between CSF CRF levels and history of childhood trauma in men with personality disorders. The results suggest that of all forms of childhood trauma assessed, childhood emotional neglect has the strongest relationship with CRF levels in personality disorders. Most human studies so far have focused on other forms of trauma, such as sexual and physical abuse. However, the type of child trauma measured by the Childhood Trauma Questionnaire emotional neglect subscale is analogous to the disruptions in maternal care administered in rodent handling and separation paradigms
(7) and primate variable foraging paradigms
(8). These studies have found evidence that early life stress leads to greater hypothalamic-pituitary-adrenal (HPA) axis function by means of less negative feedback at the level of the hippocampus and greater CRF concentration
(7,
9).
CSF CRF levels have recently been found to be positively associated with perceived early life stress in depressed and nondepressed subjects
(10). Human studies have demonstrated abnormal HPA axis function in association with history of childhood abuse in the form of enhanced ACTH hormone response to exogenous CRF
(11).
Given the presence of CRF receptors in areas of the brain associated with emotional and cognitive processing such as the amygdala and neocortex, CRF may play a role in personality psychopathology. Preliminary studies have found relationships between HPA axis abnormalities and dimensional aspects of personality psychopathology such as elevated arginine vasopressin levels in impulsive-aggressive subjects
(12).
The limitations of our study include a small number of subjects, inadequate power to explore the relationship between CRF and dimensional measures of temperament, the inclusion of only male subjects, retrospective assessment of history of childhood trauma, and the stressful nature of the lumbar puncture. Further work in this area should clarify the links between childhood trauma, CNS neurochemistry, and personality psychopathology.