Disparate health care for racial and ethnic minorities is a major public health problem. A 1999 report by the Surgeon General noted that the U.S. mental health system was not well equipped to meet the needs of racial and ethnic minority populations
(1) . Currently, Latinos are the largest and fastest growing minority group in the United States, comprising just over 13% of the population
(2) . Understanding Latino patients’ use of mental health care takes on added significance given the fact that 77% of Latinos reported that they spoke Spanish, with 24% reporting that they spoke English “not well” or “not at all”
(3) .
Acculturation has been described as “the process by which individuals adopt the attitudes, values, customs, beliefs and behaviors of another culture”
(4) . Language has consistently been the most frequently used proxy for, and strongest measure of, acculturation in Latinos
(5 –
11) . Furthermore, language has been characterized as one of the most important components of cultural identity
(12) and is correlated with other proxy measures of acculturation (e.g., nativity, time in the United States, and generation status)
(13) . Prior studies across a range of health conditions and behaviors have reported that among Latinos, acculturation has a significant effect on health status, health behavior, and use of health services. A recent review found that the relationship between acculturation and health varied; less acculturated Latinos had lower rates of substance abuse and better birth outcomes but were less likely to use health services and had lower perceived health compared to more acculturated Latinos
(14) . In mental health, prior studies have reported that acculturation was associated with a higher prevalence of substance abuse and psychiatric disorders and also with a greater likelihood of receiving mental health treatment
(15,
16) .
Most prior investigations examining mental health services among Latinos have reported that Latinos with a mental illness were less likely to receive mental health services than Caucasians
(16) . However, studies limited to patients within a specific mental health system have reported mixed results
(15) . Some investigations have found lower use of outpatient treatment
(17 –
19) ; others have reported higher rates of outpatient mental health treatment
(20), and some have reported no differences in the rates of inpatient hospitalization
(21) and outpatient treatment
(22) among Latinos compared to Caucasians
(18) . These investigations provided important contributions to our understanding of mental health service use by Latinos but had a number of limitations including not accounting for acculturation
(18,
20,
21), evaluating only English-speaking Latinos
(18,
19), examining only one type of mental health service
(17,
18,
21,
22), and assessing only patients with a single psychiatric diagnosis
(17) .
In this report, we used the administrative database of a large public mental health system to examine the effect of ethnicity and acculturation on the use of mental health services among Latinos by comparing Spanish-speaking Latinos, English-speaking Latinos, and Caucasians initiating services. We examined the type of mental health service first used and the probability of using all types of mental health services (inpatient, outpatient, emergency, and jail) during the first, second, and third year of treatment. In addition, we examined the intensity of using outpatient mental health services because this was the most commonly used type of mental health treatment. We hypothesized that Spanish-speaking Latinos would have a lower probability of using all types of mental health services, would be less likely to stay in services over time, and would receive fewer outpatient mental health visits compared to Caucasians. We also hypothesized that the pattern of mental health service use for English-speaking Latinos would be between that of Spanish-speaking Latinos and Caucasians.
Subjects and Methods
San Diego County, Calif., is located on the United States–Mexico border and has a diverse ethnic makeup. Caucasians constitute 60% of the adult population, and Latinos constitute 23%
(23) . The administrative database used for this study was derived from San Diego County’s Adult Mental Health Services system, which serves persons with Medi-Cal or no health insurance. This database included demographic information and clinical information, including psychiatric diagnosis, presence of substance use disorders, and Global Assessment of Functioning (GAF) scale scores
(24) for each recorded episode of care, and a record of each service used. We used this database in prior publications
(17,
25 –
29) . This study used data from fiscal years 2000–2005 to identify patients initiating mental health services, defined as the first use of service after a 12-month period without service use. To do this, we excluded patients who used any services in the first fiscal year (2000) or did not have a full 36-month exposure period (i.e., those initiating services after June 30, 2002).
A single variable of race/ethnicity was created; all persons identifying themselves as being of Latino ethnicity were classified as Latino, and others were categorized based on their recorded race. Language categories were created based on each patient’s self-identified preferred language. Living situation was recorded for each episode, and we created five categories based on the most frequently recorded living situation for each patient: living independently or with family, board-and-care facility, justice-related (i.e., in jail), homeless, and unknown. We used the mean GAF score as an estimate of functioning. Substance use disorder was categorized as present if any substance use diagnosis was assigned at any of the visits.
For patients with only one diagnosis recorded, we used the recorded diagnosis. For patients with more than one recorded psychiatric diagnosis, we assigned diagnoses using the following hierarchy: schizophrenia > bipolar disorder > major depression. Uncertainty regarding psychiatric diagnoses is a limitation of administrative databases, and our hierarchy favors more severe diagnoses. We used this method of determining diagnoses for several reasons. Prior investigations have reported that schizophrenia is more reliably diagnosed than depression
(30,
31) . We used this hierarchy in prior reports
(25,
27,
28) . Finally, in a previous study using the Adult Mental Health Services data set, we found there was less diagnostic variability for schizophrenia than for depression
(32) . We were not able to use an alternate method of assigning psychiatric diagnoses based on one inpatient or two outpatient diagnoses of schizophrenia
(33) because outpatient diagnoses were assigned by the treatment episode rather than at each visit and less than 20% of patients had an inpatient hospitalization.
The inclusion criteria for the present study were the following: Spanish- or English-speaking Latino or English-speaking Caucasian, use of at least one of four mental health services (see below) once during the year, a diagnosis of schizophrenia, bipolar disorder, or major depression; and a recorded GAF scale score. Of the 6,321 patients in this group, 539 (8.5%) were Spanish-speaking Latinos, and 1,144 (18.1%) were English-speaking Latinos.
Mental health services were consolidated into four categories:
1. Inpatient psychiatric hospitalization and crisis residential treatment programs
2. Emergency, which included the emergency psychiatric unit (the single county-operated psychiatric emergency room) and the psychiatric emergency response team (a law enforcement officer paired with a licensed clinician who respond to 911 calls involving mentally ill persons)
3. Jail (only clients who received mental health services while in a San Diego County jail)
4. Outpatient services, which included medication management, psychotherapy, and case management
Statistical Analysis
The three groups were initially compared on demographic and clinical characteristics with pairwise comparisons. We performed analyses of variance (ANOVAs) for continuous variables and chi-square tests for categorical variables. Differences were considered statistically significant if p<0.05.
Second, the initial type of service used was analyzed across the three groups with multinomial logistic regression and adjustment for age, gender, Medi-Cal coverage (versus being uninsured), diagnosis, substance abuse, and GAF scale score. Standardized probabilities were calculated by alternately assigning all patients to one group and estimating the mean probability of using each type of service. For example, the probability of hospitalization among Spanish-speaking Latinos was estimated by calculating the mean probability of hospitalization across all persons, assuming they were all Spanish-speaking Latinos. Standard errors were calculated with a nonparametric bootstrap test
(34) . Tests of significance for the pairwise comparisons were calculated from the empirical distribution of the bootstrapped groups.
Third, the probability of service use by type and 12-month time period was compared among the three groups with multivariate logistic regressions and adjustment for the above-mentioned demographic and clinical differences. These data were analyzed as person-periods, with three observations per person, one corresponding to each 12-month time period. Because there were substantial changes in service use across the time periods (especially from the first to second periods), we did not model within client correlation. However, we did adjust the estimated covariance matrices to account for nonindependence of observations at the client level
(35) . Standardized predicted probabilities, standard errors, and p values were calculated as described above.
Fourth, the intensity of outpatient service use among users of outpatient services (defined as the number of outpatient visits during the year) was analyzed with a generalized linear regression specified as having a gamma distribution with a log link function
(36,
37) . We employed a gamma model rather than a count model (e.g., a negative binomial model) because the distribution of outpatient services was nearly continuous. These data were analyzed as person-periods, with adjustment for initial type of service and demographic and clinical characteristics. In addition, we adjusted for region of residence because outpatient mental health services—but not other services—are organized by region in San Diego County and the majority of Spanish-speaking Latinos lived in the region directly adjacent to the United States–Mexico border. Covariance matrices were adjusted, and standardized predicted probabilities, standard errors, and p values were calculated as described above.
In addition, because psychiatric diagnosis has an important effect on mental health service use and the effect of language and ethnicity on service use may be modified by psychiatric diagnosis, each of these analyses described below was repeated separately for patients with schizophrenia, bipolar disorder, and major depression. The results of these analyses, stratified by diagnosis, are presented as data supplement Table 1 to Table 12 and are available at http://ajp.psychiatryonline.org.
Results
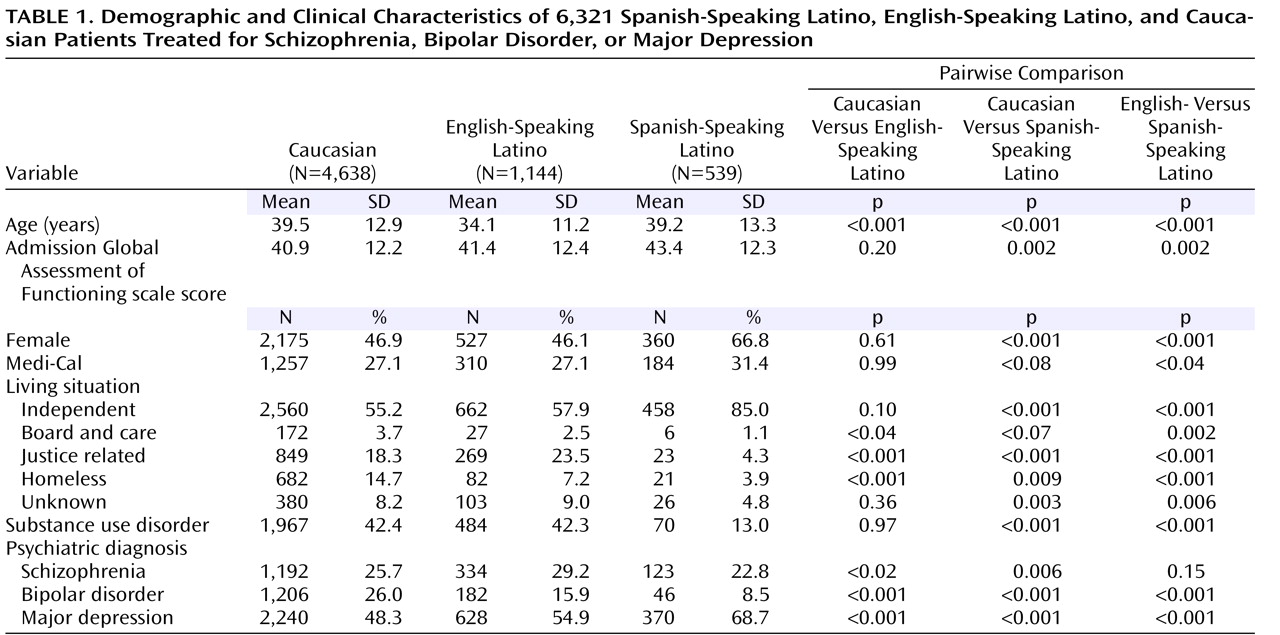
The English-speaking Latinos were younger than the Spanish-speaking Latinos, who were younger than the Caucasians (
Table 1 ). Approximately half of the English-speaking Latinos and Caucasians were women, compared to more than two-thirds of the Spanish-speaking Latinos. The Spanish-speaking Latinos were more likely to have Medi-Cal than the patients in the other two groups. The most common living situation in all three groups was living independently or with family, and the rates of this living situation were higher among the Spanish-speaking Latinos than among the English-speaking Latinos and Caucasians. The rates of living in board-and-care homes or being homeless were lower among the Spanish-speaking Latinos than among the English-speaking Latinos or the Caucasians.
The highest proportion of patients with schizophrenia was among the English-speaking Latinos, followed by the Caucasians. The Caucasian patients had the greatest proportion with bipolar disorder, followed by the English-speaking Latinos. The Spanish-speaking Latinos had the lowest proportion with both schizophrenia and bipolar disorder. Conversely, the Spanish-speaking Latino patients had the highest proportion with major depression, with lower rates observed among English-speaking Latinos and Caucasians. The prevalence of comorbid substance use disorders was lowest among the Spanish-speaking Latino patients (9.0%), whereas approximately one-third of the English-speaking Latino and Caucasian patients had this diagnosis. The Spanish-speaking Latino patients had higher mean admission GAF scale scores than the patients in the other two groups, although the magnitude of these differences was small and of questionable clinical significance. These findings were similar when the three diagnostic groups were examined separately, with a few exceptions: more than 75% of the Spanish-speaking Latino patients with depression were female, compared to just over half of the Caucasian and English-speaking Latino patients with depression, and the rates of Medi-Cal insurance were higher only for the Spanish-speaking patients with major depression (data supplement Tables 1, 5, and 9).
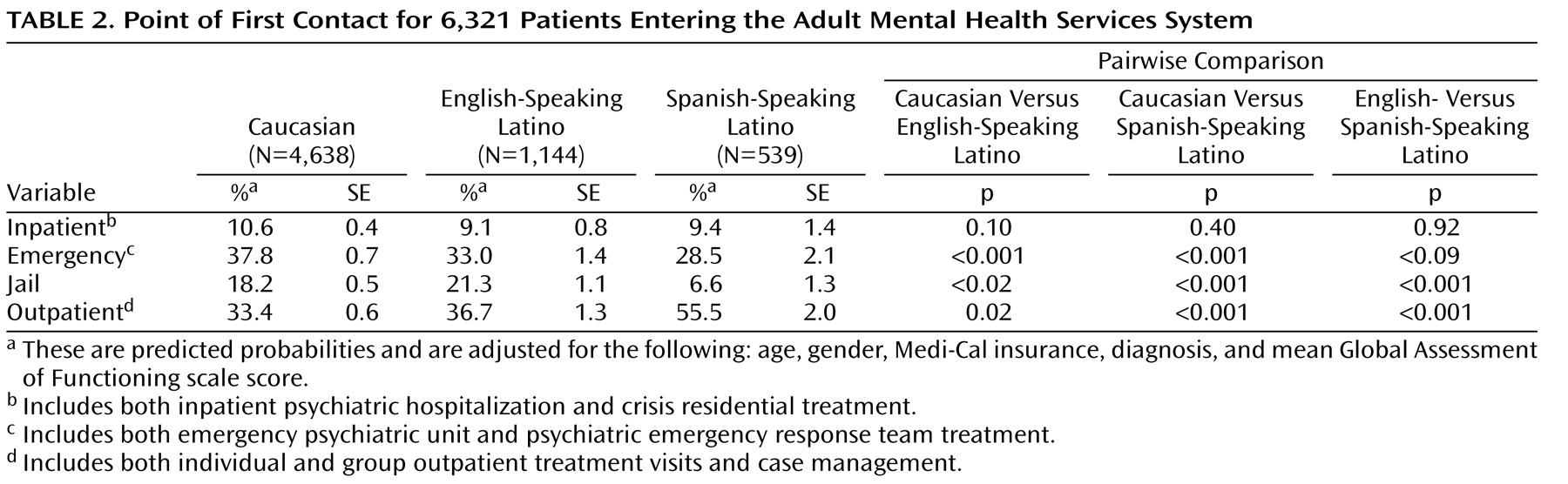
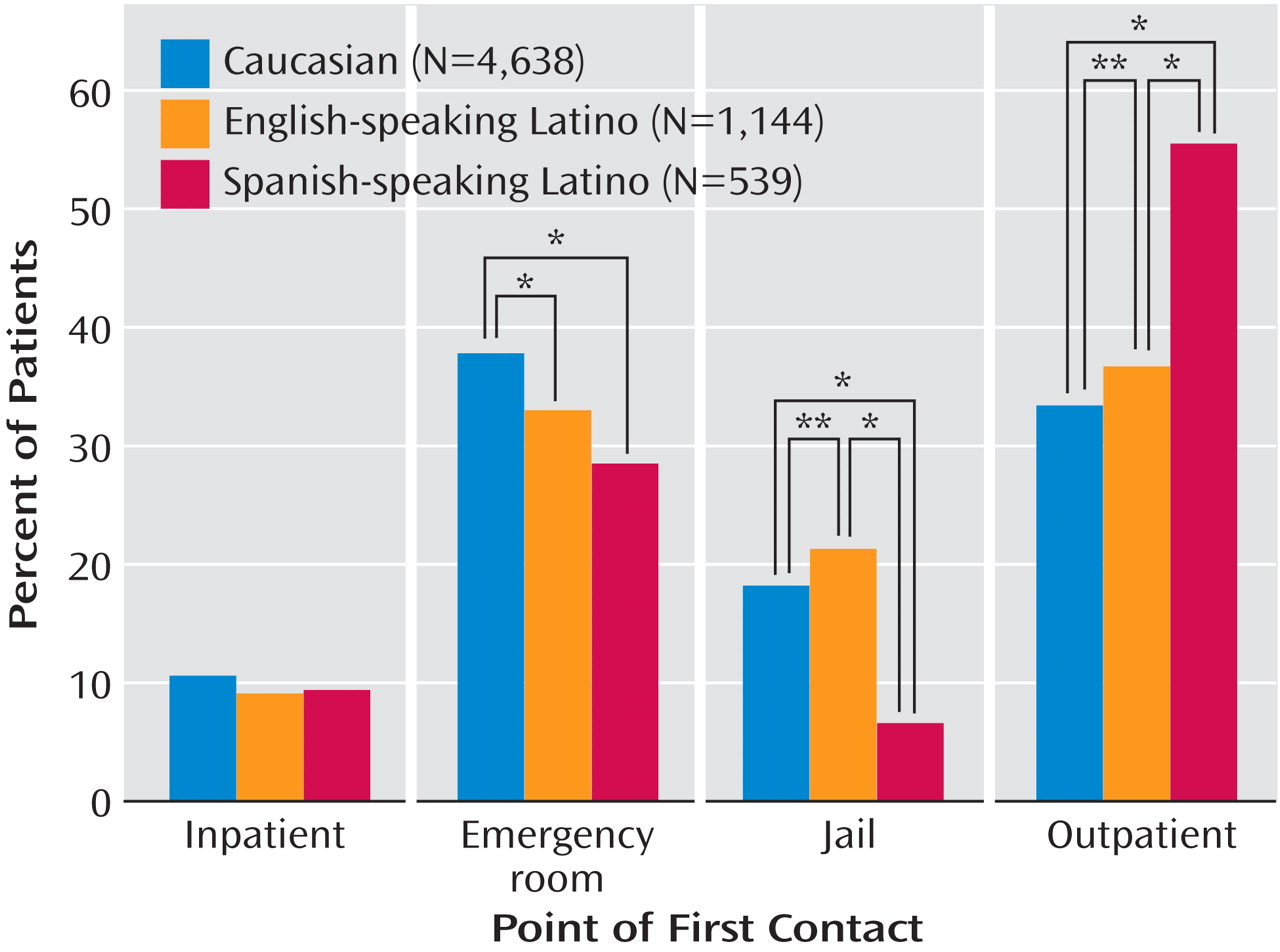
For all three groups, outpatient was the most frequent point of first contact, but Spanish-speaking Latinos were more likely than English-speaking Latinos or Caucasians to first receive care in the outpatient setting (
Table 2,
Figure 1 ). The next most frequent point of entering the Adult Mental Health Services system was through emergency services, either the emergency psychiatric unit or psychiatric emergency response team. Spanish-speaking Latinos and English-speaking Latinos had lower rates of entering treatment through emergency services than Caucasians. Jail was the point of first contact for approximately one-fifth of Caucasians and English-speaking Latinos, whereas the rate of entering treatment through jail was significantly lower for Spanish-speaking Latinos. Finally, the rates of inpatient service as the point of first contact were similar for all three groups, at approximately 10%. When the three diagnostic groups were examined separately, the most common point of entry to mental health care for the patients with schizophrenia or bipolar disorder was through emergency services, and all three ethnicity/language groups had similar rates. In contrast, the patients with major depression most frequently entered through outpatient treatment, and Spanish-speaking Latino patients had a lower rate of entering through emergency services than English-speaking Latinos, who had a lower rate than Caucasians. Finally, the rate of entering treatment through inpatient hospitalization was similar for all three language/ethnicity groups except for patients with schizophrenia, where Spanish-speaking Latino patients were less likely to enter treatment through inpatient hospitalization (data supplement Tables 2, 6, and 10).
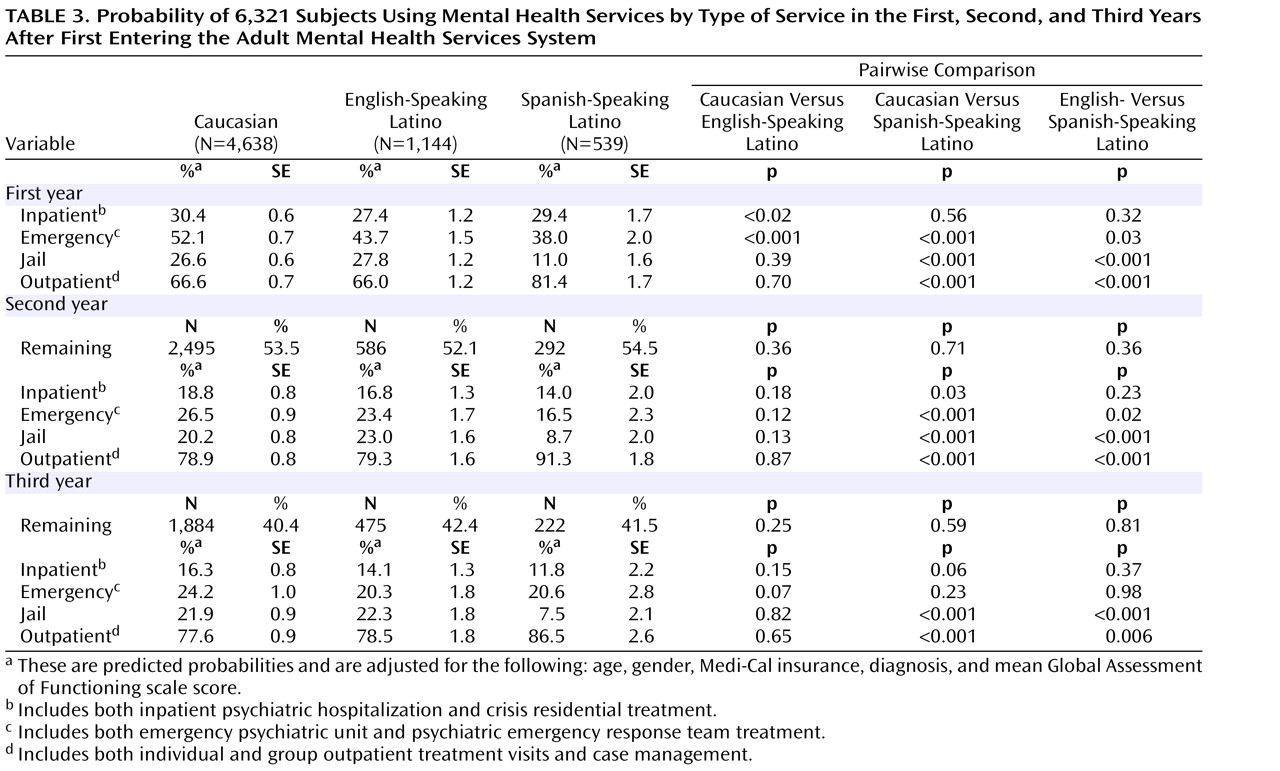
In the first year, the probability of using inpatient hospitalization was similar for Spanish-speaking Latinos and Caucasians and slightly lower for English-speaking Latinos. Use declined in subsequent years, and patients in all three groups had similar rates of inpatient use (
Table 3 ). In the first year, emergency use was highest for the Caucasians, followed by the English-speaking Latinos, and lowest for the Spanish-speaking Latinos. In years two and three, the proportions of patients in all three groups using emergency services were similar and lower than in year one. Jail use was higher in years two and three for the English-speaking Latinos and Caucasians and lower for the Spanish-speaking Latinos. Finally, outpatient use was higher in years two and three for the Spanish-speaking Latinos and lower for the English-speaking Latinos and Caucasians. Over the first 3 years of treatment, the proportion of patients remaining in the system decreased at a similar rate for all three groups; approximately half of the patients who entered services received any services in year two and 40% received services in year three. By the third year, the only significant difference between the groups was that the Spanish-speaking Latinos were less likely to use mental health services in jail and more likely to use outpatient treatment compared to the other two groups. When the three diagnostic groups were examined separately, the results were similar with the following exceptions: for the patients with schizophrenia, there were no differences in inpatient use among the three ethnicity/language groups in any of the years. The Spanish-speaking patients with bipolar disorder were more likely to have an inpatient hospitalization in year one and less likely in year two compared to the Caucasian patients. Finally, for the patients with schizophrenia, the proportion remaining in treatment was higher for the English- and Spanish-speaking Latinos than for the Caucasians (data supplement Tables 3, 7, and 11).
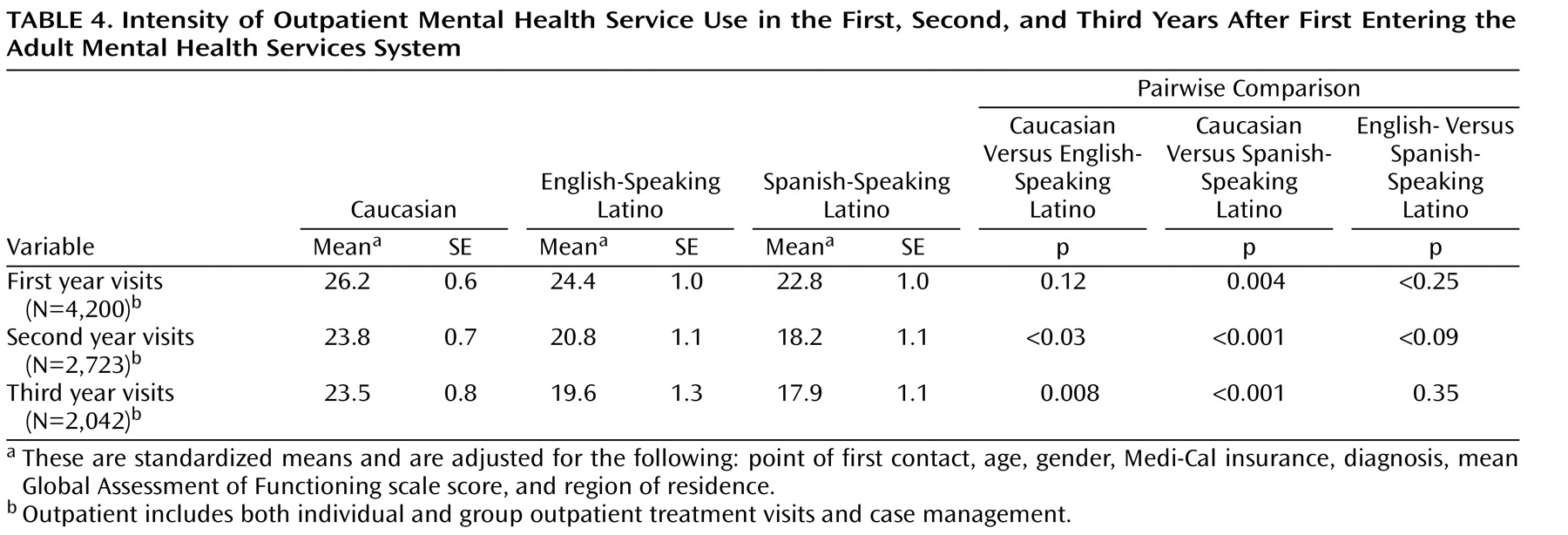
In their first year of care, the Caucasians had more outpatient visits than the Spanish-speaking Latinos (
Table 4 ). In years two and three, all three groups had fewer visits than in the first year, but the Caucasians received significantly more visits over all 3 years than either the English- or the Spanish-speaking Latinos. When the three diagnostic groups were examined separately, the patients with bipolar disorder had similar numbers of outpatient visits in all 3 years. In addition, for the patients with schizophrenia and bipolar disorder, the three race/ethnicity groups had similar numbers of outpatient visits for each of the years. Finally, the greater number of outpatient visits for the Caucasian patients was consistently found only for the patients with major depression (data supplement Tables 4, 8, and 12).
Discussion
The most striking finding of this investigation was that the Spanish-speaking Latinos differed from the English-speaking Latinos on most demographic, clinical, and service use measures, whereas there were a few differences between the English-speaking Latinos and the Caucasians. The Spanish-speaking Latinos differed from the other two groups in terms of service use in the following ways: the Spanish-speaking Latinos 1) were least likely to enter mental health services through emergency care or jail, 2) were most likely to enter mental health services through outpatient treatment, 3) had the highest proportion using outpatient services, and 4) had the lowest intensity of outpatient visits per subject. There were no differences among the three groups in the proportion that stayed in mental health treatment or used inpatient hospitalization. These findings persisted after we controlled for clinical and demographic differences among the three groups and after we repeated the analyses separately for each diagnostic group.
On most clinical and demographic measures, the Spanish-speaking Latinos differed from the other groups, whereas there were a few differences between the English-speaking Latinos and the Caucasians. Three variables that merit particular consideration are living situation, psychiatric diagnosis, and prevalence of comorbid substance use disorders. Spanish-speaking Latinos were more likely to live independently or with family and less likely to live in board-and-care homes, to be incarcerated, or to be homeless than the English-speaking Latinos and Caucasians. It is possible that among Spanish-speaking Latinos, protective social structures and family ties buffer against some of the negative effects of mental illness
(38), although this database lacks the information needed to further explore this relationship. Second, Spanish-speaking Latinos were more likely to be diagnosed with major depression, whereas the other two groups had higher rates of bipolar disorder and schizophrenia. The higher proportion of women among the Spanish-speaking Latinos may partially explain these differences, although these differences persisted in the stratified analyses of patients with schizophrenia and bipolar disorder, groups with smaller differences in gender distribution. In addition, misdiagnosis, previously reported among minority patients
(39), may also contribute to this finding. Finally, consistent with prior reports
(16), the prevalence of substance use disorders was significantly lower among the Spanish-speaking Latinos than among the English-speaking Latinos and Caucasians.
The findings of prior investigations of mental health use by Latinos have been mixed, with three reporting “favorable” and two reporting “unfavorable” patterns of use. The favorable patterns included less inpatient and more outpatient mental health treatment than Caucasians
(20), similar rates of inpatient hospitalization and lengths of stay when hospitalized
(21), and a greater number of therapy sessions for Spanish-speaking patients
(22) . However, these reports had limitations, including not differentiating between Spanish- and English-speaking Latinos
(20), the inclusion of all psychiatric diagnoses (fewer than 50% of the patients had a severe mental illness)
(20), not reporting data separately for English versus Spanish-speaking Latinos
(22), and not including monolingual Spanish speakers
(21) . In contrast, a Veterans Administration study found that Latinos had lower use of outpatient (but not inpatient) mental health treatment following an inpatient hospitalization
(19) ; however, only a small proportion of the patients were monolingual Spanish speakers. A second investigation, from our group, examined the use of case management in patients with schizophrenia in the Adult Mental Health Services system in 1998. This report found that Latinos were less likely than Caucasians to receive services from specialized case management providers, a finding that persisted after adjustment for language
(17) . However, other mental health services were not examined in that investigation.
There are several possible explanations for the observed differences in mental health service use among the three groups in our study. First, Latinos with a mental disorder, and particularly Spanish-speaking Latinos, enter into mental health care at lower rates than Caucasians. Prior epidemiologic studies of the general population (as opposed to investigations of patients receiving mental health treatment) have consistently found that Latinos with a psychiatric disorder were less likely to receive mental health services than Caucasians
(15,
40,
41) . Mechanic and Bilder characterized the U.S. mental health care system as being “highly dependent on perceived need and demand, and those with resources and insurance get care more easily”
(42) . For Latinos, low rates of health insurance
(43), cultural beliefs about mental health problems that differ from those of Caucasians
(15), and the protective effects of family and social networks
(15) may result in Latinos being less likely to enter into mental health care but have less effect on what type of mental health services a person receives. Second, the healthy immigrant hypothesis proposes that Latinos who have migrated from Mexico to the United States are a select group and are healthier than the general population of either the United States or Mexico
(44,
45) . Therefore, these “healthy immigrants” may need fewer mental health services than English-speaking Latinos or Caucasians. Third, acculturation, a process of cultural change and adaptation
(46), may result in changes in patients’ culturally based treatment preferences
(47) and may be responsible for the elevated prevalence of mental illness diagnoses in U.S.-born Latinos compared to those born in Mexico or other Latin American countries
(16,
48) . Fourth, given San Diego’s proximity to the U.S.–Mexico border, some Spanish-speaking Latinos may have returned to Mexico to obtain mental health services
(49) . These explanations are not mutually exclusive, and the data that we have do not allow us to test these hypotheses. Nonetheless, these are important questions for future research.
There are several limitations to our study. We used administrative data, and some clients may use informal care outside mental health services. The accuracy of the clinical diagnoses and GAF scale scores may be lower than in research studies; however, these are the diagnoses used by Adult Mental Health Services clinicians. The large group size may lead to statistically significant findings that are of limited clinical use. Spanish language use was used as a proxy for acculturation; we did not have other measures of acculturation such as nativity, time in the U.S., or generation status. However, prior investigations have also used Spanish language as a proxy for acculturation
(50 –
52) . Our study was limited to persons who received mental health care at least once, and therefore, we cannot determine the prevalence of these disorders in the general population or investigate access to mental health care. It is possible that a number of Spanish-speaking Latinos were unable to access any public mental health services, an important concern pointed out by prior reports. Finally, it is possible that the San Diego County public mental health system is particularly effective in providing care to Spanish-speaking Latinos; therefore, these findings need to be confirmed in other public mental health systems.
Notwithstanding these limitations, our findings suggest that Spanish- and English-speaking Latinos have different patterns of mental health use. Rather than finding underuse of all mental health services by Spanish-speaking Latinos, as hypothesized, the results were mixed. The Spanish-speaking Latinos had a more favorable pattern of service use than the other two groups on some measures, including using the emergency psychiatric unit and jail (lower probability of entering care through these services or using these services) and outpatient services (higher probability of entering care through this service and higher probability of using this service). However, the Spanish-speaking Latinos had fewer outpatient visits in all 3 years, a less favorable pattern of service use. Finally, the proportion of patients who continued to use services over time was the same for all three groups. These findings need to be replicated in other public mental health systems. Our findings suggest that language, which is a proxy measure of acculturation, may be more important than ethnicity for understanding Latinos’ use of mental health services and that future studies comparing the mental health service use of Latinos to that of Caucasians need to differentiate between Spanish- and English-speaking Latinos.