Amphetamine abuse and dependence represent a major public health problem with growing psychiatric, social, and economic consequences. The total number of amphetamine abusers worldwide is estimated at 34 million, which exceeds the combined number of cocaine and heroin abusers
(1) . In Sweden, amphetamine is the most commonly abused substance after cannabis and alcohol
(2) . Thus far, treatment of amphetamine users in emergency departments and psychiatric clinics has focused on management of the acute and short-term consequences of amphetamine dependence, such as withdrawal symptoms, amphetamine-induced psychosis, and associated depression. However, treatment targeting only acute or short-term problems has proved insufficient for alleviating recurrent craving and preventing relapse to compulsive drug use
(3) . To date, an efficacious pharmacotherapy has remained elusive, despite extensive research on the neurobiological effects of amphetamine
(4) .
The reinforcing effects of amphetamine are principally mediated via stimulation of the cortico-mesolimbic dopamine system
(5) . However, other neurotransmitter systems modulate brain dopamine, such as the μ-opioid receptors, which are located on the mesolimbic dopamine neurons
(6) . Furthermore, certain brain regions known to have a role in appetitive behaviors, such as the ventral tegmental area and the substantia nigra, contain neurons in which dopamine and opioids coexist
(7,
8) . The important functional interaction of the dopamine-opioid system specifically in stimulant abuse is evident from results of preclinical and clinical studies. For example, in rat studies, chronic administration of cocaine has been shown to increase brain m-opioid receptor binding in regions relevant to reward (such as the amygdala and the nucleus accumbens), and this effect seems to be mediated through dopamine receptors, which is evident in the fact that coadministration of dopamine receptor antagonists blocks this effect
(9,
10) . A recent positron emission tomography study demonstrated an increase in m-opioid receptor binding in limbic areas in chronic cocaine abusers, and this increased binding was correlated with self-reported craving
(11) .
Although these changes were observed after chronic cocaine use, a similar effect could be expected in amphetamine use, based on the common pharmacological mechanisms of these drugs. Clinical data from our earlier studies using naltrexone, an opioid antagonist, with healthy volunteers
(12) and with amphetamine-dependent patients
(13) demonstrated that naltrexone blunted the subjective effects of amphetamine in both populations. In the patients, naltrexone also reduced craving for amphetamine. These results suggest that there could be a dopaminergic-opioid interaction in amphetamine use as well. The finding that an acute dose of naltrexone attenuated the subjective effects of amphetamine under experimental laboratory conditions demonstrates a potential pharmacotherapeutic efficacy of naltrexone for the treatment of amphetamine dependence.
Taken together, the preclinical and human laboratory studies provide the rationale for a clinical trial evaluating the efficacy of naltrexone in reducing relapse to amphetamine use in amphetamine-dependent individuals.
Method
Participants
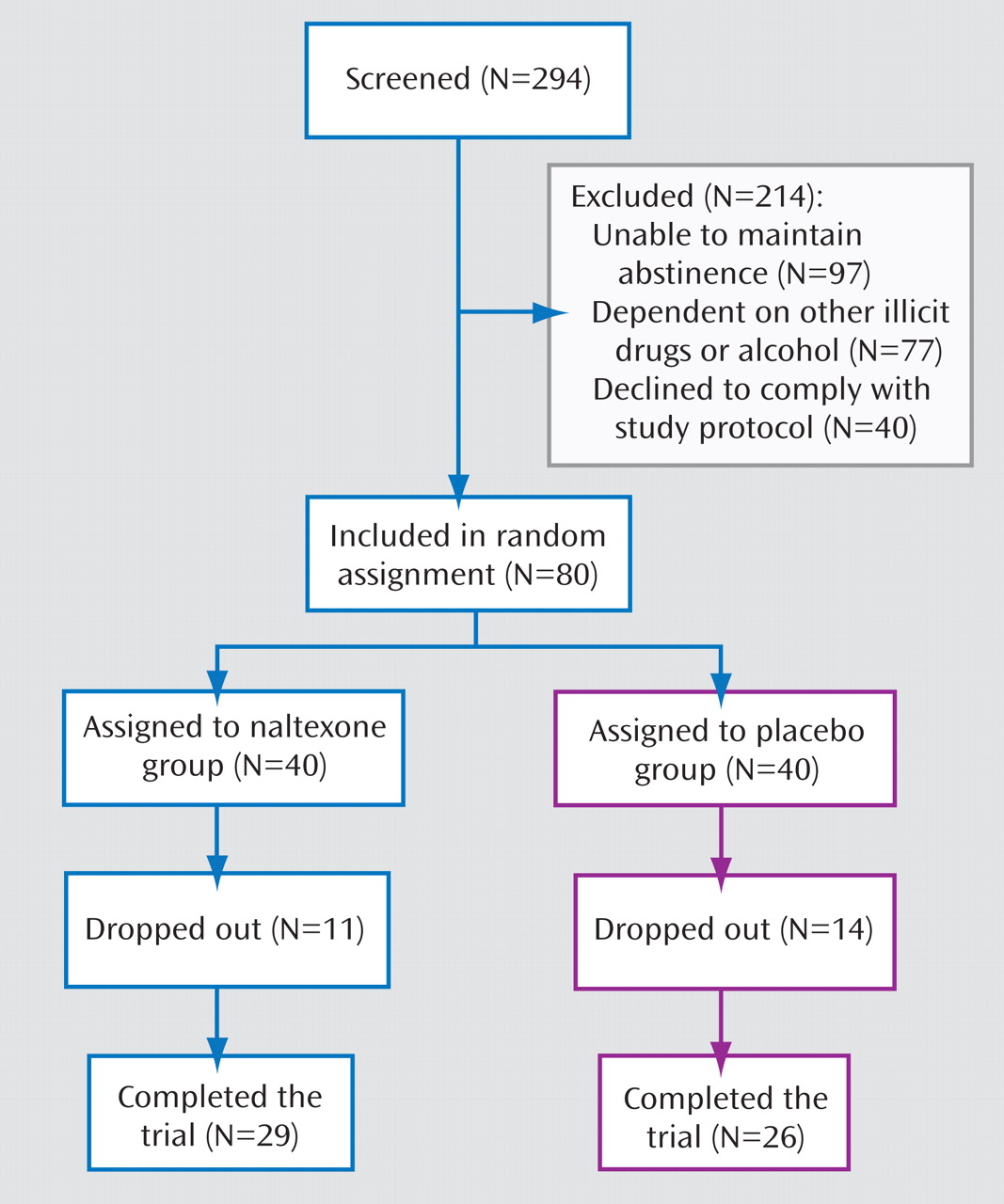
A total of 80 treatment-seeking amphetamine-dependent individuals 20–65 years of age were recruited from the Stockholm metropolitan area via advertisements in local newspapers and written information sent to social workers. The study was approved by the regional ethical review board in Stockholm and the Swedish Medical Products Agency, and the trial was conducted in accordance with the Good Clinical Practice Guideline of the International Conference on Harmonization and with the Declaration of Helsinki. Written informed consent was obtained from all patients.
To be eligible for the study, patients had to meet DSM-IV criteria for amphetamine dependence and to have used amphetamine on at least 12 days in the past 12 weeks. Exclusion criteria included a current DSM-IV diagnosis of any other substance dependence syndrome except nicotine; a history of a major psychiatric disorder (e.g., schizophrenia or psychosis) or a current psychiatric condition requiring medication; use of any opioid medication or illicit opiates in the past month; current use of benzodiazepines; traces of any illicit substance in the urine (amphetamine, benzodiazepines, cannabis, cocaine [benzoylecgonine], dextropropoxyphene, or opiates); a serious somatic disease (e.g., seizure disorder, glaucoma, arteriosclerosis, hyperthyroidism); serum aspartate or alanine aminotransferase activity greater than three times the upper reference range or a serum bilirubin concentration greater than twice the upper reference range; and pregnancy or lactation.
Study Design
This was a single-site randomized, double-blind, placebo-controlled trial of naltrexone for amphetamine dependence. Enrollment began in January 2003 and ended after 29 months. Initial eligibility was ascertained by telephone screening. All eligible patients had a 2-week lead-in period to assist with and confirm their current drug-free state. This process enabled the inclusion of patients who not only expressed a verbal motivation and commitment to seek treatment but also displayed some supporting behavioral evidence.
After the lead-in period, 80 patients were randomly assigned to receive either placebo or naltrexone treatment for 12 weeks. The randomization process was conducted by the Karolinska University Hospital pharmacy with software designed for the purpose. The randomization code was kept by the pharmacy and disclosed at the end of the trial. No interim analysis was performed. Patients were asked to attend the clinic twice weekly. On the first weekly visit, they met with a research nurse, filled out questionnaires, left supervised urine samples, and collected the weekly medication. On the second weekly visit, they received relapse prevention therapy from a licensed psychologist and left supervised urine samples. All urine samples were screened for amphetamine, benzodiazepines, cannabis, cocaine (benzoylecgonine), dextropropoxyphene, and opiates.
Assessments and Outcome Measures
At intake each patient underwent a physical examination and was assessed with the Structured Clinical Interview for DSM-IV. In addition, urine and blood analyses were conducted. Current symptoms of attention deficit hyperactivity disorder (ADHD) were assessed at baseline, first using a checklist of DSM-IV criteria and then a complete neuropsychiatric battery, including interviews with parents or siblings, to ascertain the diagnosis of ADHD. The Addiction Severity Index
(14) was administered before (week 0) and after treatment (week 12). Weekly assessments included self-reports of drug consumption, which were obtained by the timeline followback interview
(15), and of craving for amphetamine, which was assessed on a 7-point visual analogue scale measuring craving at the present moment and over the past week (adapted from the Tiffany et al. cocaine craving scale
[16] ). Monitoring of adverse effects was carried out by both the physician (through interview) and the patient (in self-ratings of intensity and duration) using a standardized form. At weeks 4, 8, and 12, liver enzyme and bilirubin concentrations were measured.
Urine samples were screened for amphetamines by immunoassay with a cutoff level of 500 ng/ml. The confirmation analyses of the positive samples, which included amphetamine, methamphetamine, 3,4-methylenedioxyamphetamine, and 3,4-methylenedioxymethamphetamine (reporting limit=300 ng/ml), were performed using a liquid chromatography-tandem mass spectrometry method
(17) .
Treatments
Naltrexone (50-mg capsules) and matching placebo capsules were obtained through the Karolinska University Hospital pharmacy and prepared for each patient in medication blister packages. Each week, participants received a blister package containing seven capsules, dispensed by the nurse. On the following visit, patients returned the empty blister package with any remaining capsules for pill count. Weekly urine samples were assayed for 6-β-naltrexol, the active metabolite of naltrexone, by mass spectrometry with a quantification limit of 1 μg/ml. Adherence to medication was assessed by detection of 6-β-naltrexol in urine and by pill counts.
All participants received standardized manual-based relapse prevention therapy
(18), delivered in 60-minute sessions once weekly by a licensed psychologist. All sessions were individualized and documented in the case record forms by the therapist.
Power Calculation
With the prediction of a between-group difference of 16% and a standard deviation of 20% (corresponding to a strong effect size according to Cohen’s definition), an effective sample size of 2×30 was calculated to give a corresponding power of 0.85. Given the high probability of dropouts, we increased the sample size to 2×40.
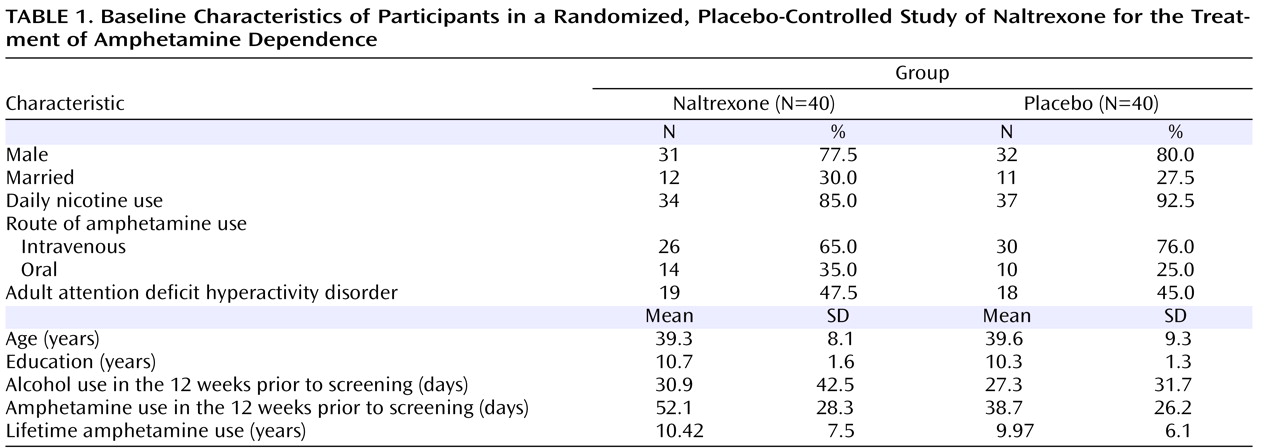
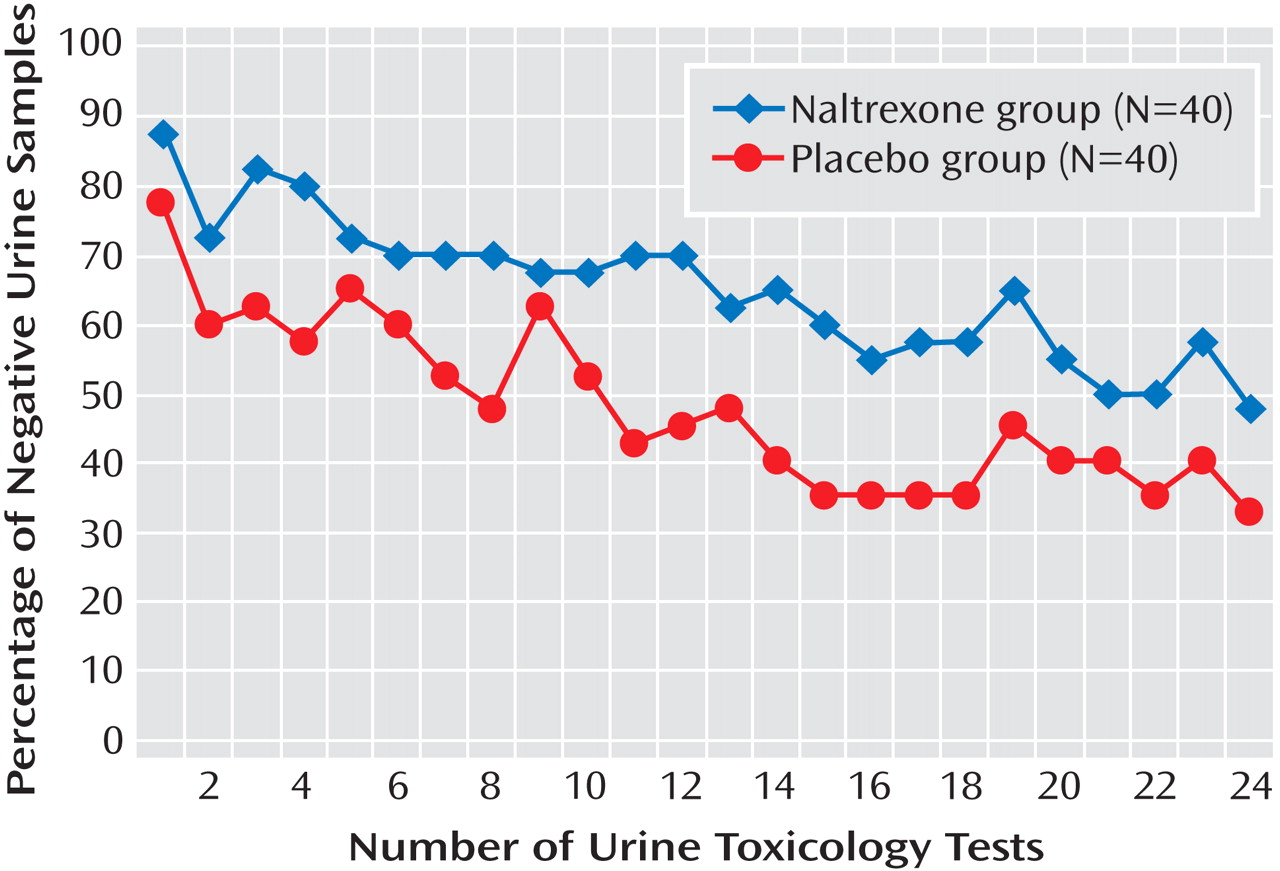
Data Analysis
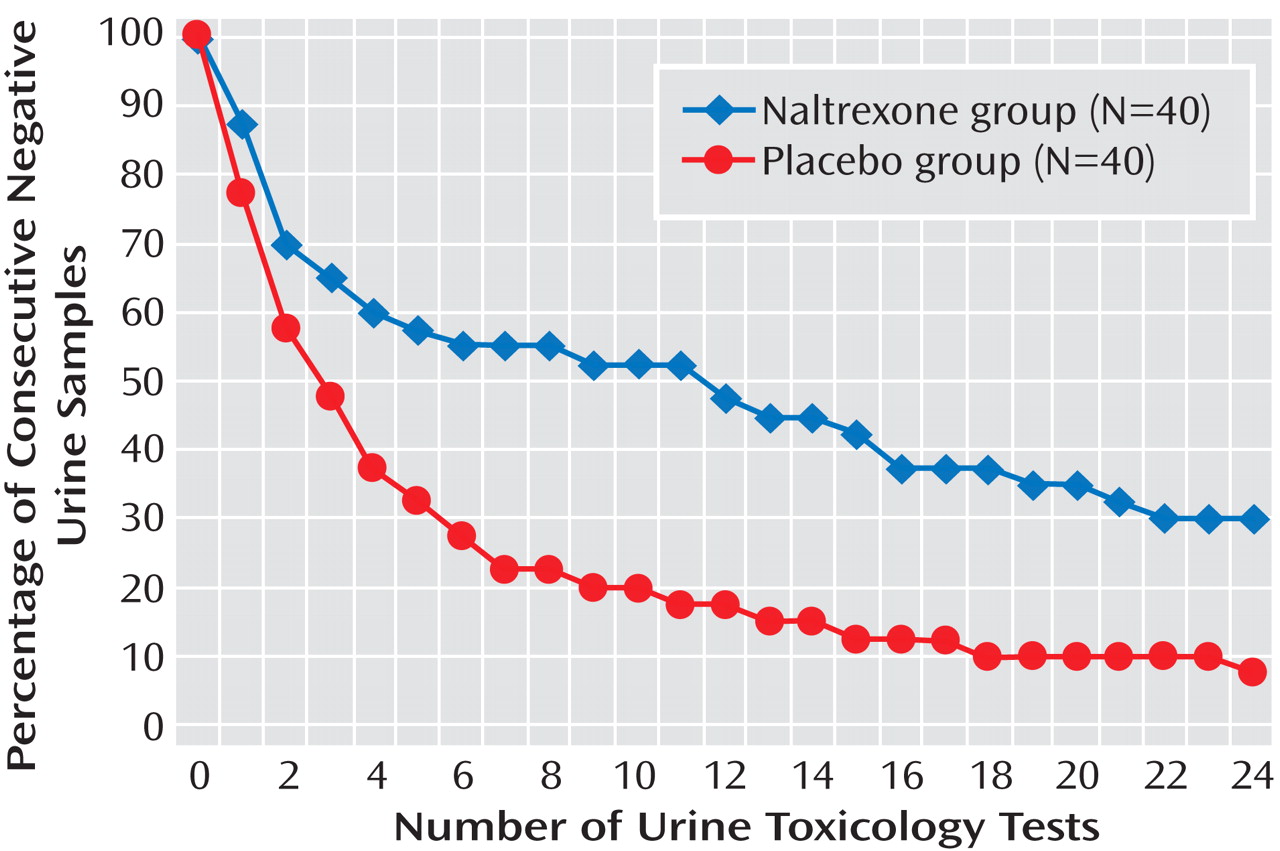
The primary outcome measure of the study was the number of negative amphetamine urine samples during 12 weeks of treatment (of a total of 24 samples). All missing urine samples were defined as positive in the analysis. The primary analysis was carried out according to the intention-to-treat approach. Treatment efficacy was analyzed by repeated-measures analysis of variance (ANOVA) comparing naltrexone and placebo patients over 12 weeks. A secondary completer analysis on the primary outcome measure was conducted using the same statistical method; a completer was defined as per protocol as a patient who provided at least 16 of the total of 24 urine samples. Time-to-event (relapse) analysis was carried out for both the intention-to-treat and completer samples.
A Kaplan-Meier analysis was used to compute rates of continuous abstinence from amphetamine, in which the time-dependent survival (nonrelapse as measured by negative amphetamine urine samples) probabilities for both treatment groups were computed for both the intention-to-treat and completer samples.
The secondary outcome measures were self-reported use of amphetamine, alcohol, and other drugs; craving for amphetamine; and liver enzyme levels. All secondary measures were analyzed by repeated-measures ANOVA comparing naltrexone and placebo patients over 12 weeks of treatment.
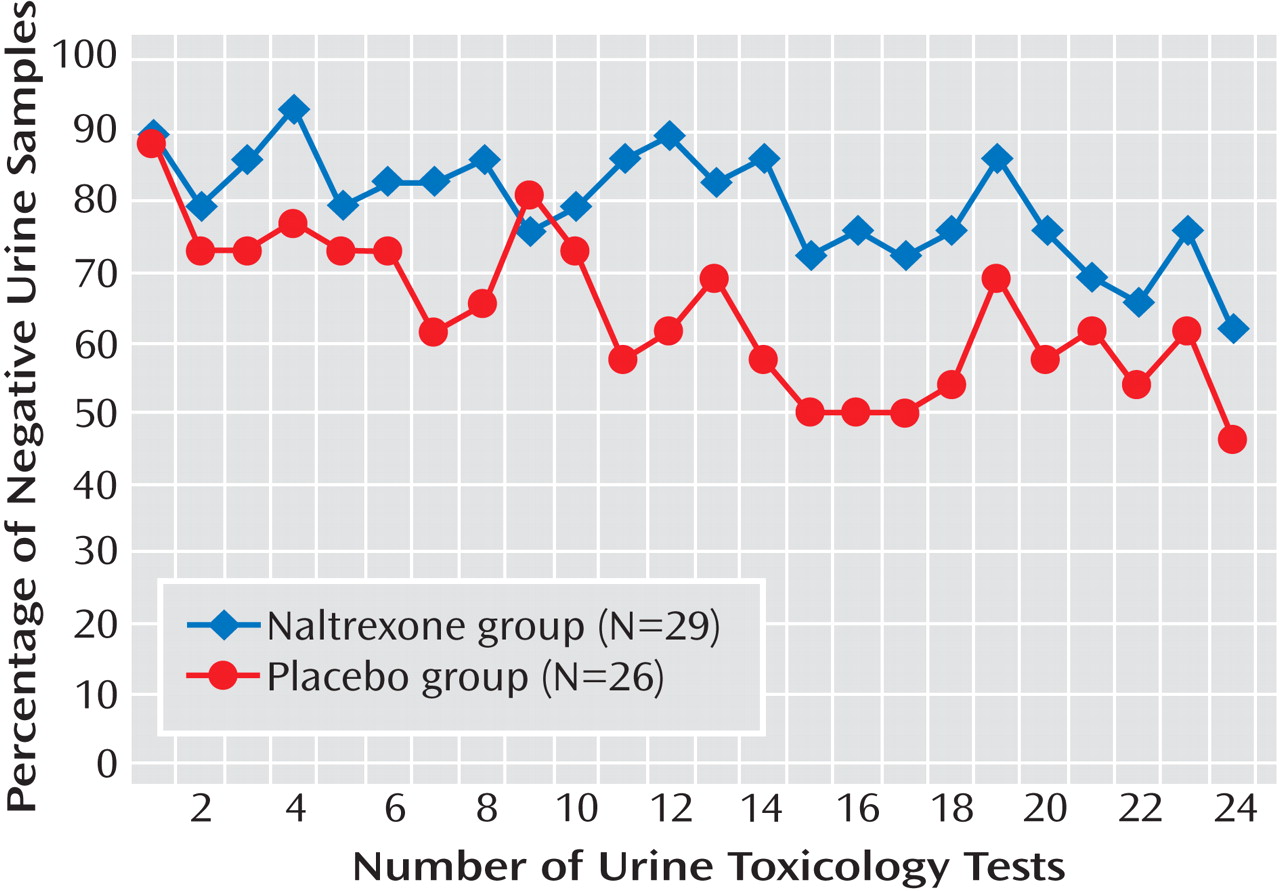
Patients were compared on baseline characteristics using chi-square tests for categorical variables and t tests for continuous variables in order to assess the efficiency of the randomization procedure in ensuring homogeneity between the two treatment groups.
Discussion
To our knowledge, this is the first study to report the efficacy of naltrexone for the indication of amphetamine dependence. The study demonstrated a significant effect of medication on reducing amphetamine use, with an effect size of 0.5 for the intention-to-treat sample, which is comparable to the effect size of naltrexone for alcohol dependence. Treatment with naltrexone reduced the percentage of amphetamine-positive urine samples in patients with chronic amphetamine dependence. The mechanism by which naltrexone mediates this effect is not clear. It has been established
(13,
19,
20) that the therapeutic effect of naltrexone does not result from any nonspecific effect, such as a pharmacokinetic interaction. A more probable mechanism is a reduction of the mood-altering or other subjective effects of the stimulant (e.g., euphoria or liking the drug’s effect), leading to a reduction in drug use. Our findings indicate that a 12-week treatment with naltrexone leads to a sustained effect on the behavioral and subjective correlates of amphetamine dependence, that is, a reduction in drug consumption and craving.
In our sample, in which daily doses of amphetamine use before enrollment ranged from 0.5 g to 2 g, adherence to treatment was generally good. An analysis of the participants who adhered to the study medication (as assessed by the presence of 6-β-naltrexol in urine) was performed to elucidate more clearly the treatment effects of naltrexone. In the naltrexone group, 62.5% of patients exhibited a continuous measure of adherence to medication. Adherence to medication was correlated with reduction in drug use, indicating that adequate exposure to the medication was an important factor in the change in amphetamine use patterns. The duration of effect of amphetamine is 6–10 hours, while the plasma half-life of a 50-mg dose of naltrexone is 10–12 hours, with an ability to block the μ receptor for more than 72 hours
(21) . This, in combination with reductions in amphetamine use and craving, suggests that the duration of inhibition of the opioid receptors by a 50-mg dose of naltrexone was sufficient to counteract the reinforcing effect of amphetamine. Attendance at the relapse prevention sessions was similar for the two groups, and this may have contributed to the observed reduction in drug use in the placebo group as well. While the absence of a biomarker for adherence to placebo medication is a limitation of the study, the results indicate that the ability of naltrexone to promote a clinically significant reduction in drug consumption may be highly dependent on medication adherence.
At the start of treatment, the mean craving scores for the naltrexone and placebo groups were similar. Continued treatment with naltrexone, however, led to a reduction in craving scores as compared with placebo treatment over 12 weeks, and this was evident from week 4 onward. Previous treatment studies of alcohol and cocaine dependence have reported that naltrexone may affect the likelihood of future drug use by decreasing both craving for and liking of the drug
(22,
23) . The clinical significance of this finding is that despite exposure to amphetamine, the reduction in craving for the drug with naltrexone treatment in turn reduces the risk of relapse and helps patients maintain the motivation (enhanced by the relapse prevention therapy) to remain drug free. Thus, it may be that the decrease in drug consumption with naltrexone treatment results from its action on reducing the pleasure and/or high along with the craving. The reduction of these pleasurable effects, along with a greater control over the craving-driven impulses, could also be expected to reduce the likelihood that a patient will increase the daily dose of amphetamine to achieve a larger effect.
There was no evidence (by urine toxicology or timeline followback) of any increase in intake of alcohol or other drugs during treatment to compensate for the reduction in amphetamine consumption. The data provide evidence that the reduction in amphetamine use is mediated by a combination of relapse prevention therapy and medication treatment rather than a consequence of an increase in use of other drugs.
Treatment with naltrexone did not produce any serious adverse effects, and no dropouts were attributed to adverse events. This is consistent with earlier studies of naltrexone for alcohol- and amphetamine-dependent patients
(24,
25), and it suggests that the reasonable adherence and retention rates observed in the naltrexone group are partly related to the lack of significant medication side effects.
There was no differential response to treatment with regard to gender or ADHD diagnosis. The presentation of an ADHD diagnosis among amphetamine-dependent patients was fairly high in our sample, approaching 50%, a proportion similar to that reported in another study
(26), which suggests that there could be a high prevalence of ADHD in the general amphetamine-dependent population.
In Sweden, the vast majority of amphetamine abused is the racemic mixture (
d/l -amphetamine), whereas in other countries, methamphetamine is more common. A quantitative analysis of different amphetamine derivatives in the urine revealed that 16% percent of positive samples displayed a high concentration of methamphetamine. Preclinical data have shown that pretreatment with naltrexone attenuated behavioral sensitization
(27) and cue-induced methamphetamine-seeking behavior in rats
(28) . Our results in this study, together with these preclinical findings, provide some preliminary evidence of naltrexone’s applicability in methamphetamine dependence as well.
Some limitations of this study must be acknowledged. The sample selected for the study did not achieve an equal representation of the genders. Treatment outcome was assessed for 3 months, and long-term effects in this population are unknown. In addition, future studies should also include patients with major depression to understand the impact of treatment with naltrexone on drug use and the symptoms of depression.
The results of this study extend the findings from previous human experimental laboratory studies
(12,
13) by providing evidence of the efficacy of naltrexone in reducing relapse to amphetamine use. Medication adherence and retention to treatment was high in the group treated with naltrexone, which may be regarded as further proof of concept for naltrexone as a treatment for amphetamine dependence.