The epidemic of psychiatric disorders in the U.S. prison system represents a national public health crisis. Epidemiologic studies show that 15%–24% of U.S. inmates have a severe mental illness
(1 –
3), and a recent report by the Bureau of Justice Statistics indicates that half of inmates—over 1 million individuals—have at least one mental health condition
(4) . Several factors have synergistically led to the excess of mental illness in the U.S. correctional system. In the late 1960s, with the availability of new antipsychotic medications, a national movement resulted in the mass closing of public mental health hospitals
(5 –
7) . Many leaders in the psychiatric community argued that moving patients out of state hospitals and into community-based outpatient settings represented a humane alternative to overcrowded and understaffed institutions. Unfortunately, in most cases, the closing of state hospitals was not accompanied by the promised number of clinics and halfway houses necessary to care for released hospital patients
(5 –
7) . In subsequent years, health insurers restricted mental health coverage, private hospitals limited enrollment of psychotic patients, and civil commitment laws became more restrictive
(5) . Additionally, beginning in the 1980s, the “war on drugs,” which led to an increase in drug-related arrests and an emphasis on mandatory and fixed sentencing, resulted in dramatic increases in the proportion of inmates with psychiatric disorders and substance abuse problems
(8,
9) . All of these factors have culminated in a revolving-door phenomenon in which many mentally ill people move continuously between homelessness and the criminal justice system
(5,
10) .
Method
Design and Study Sample
This was a retrospective cohort study of all TDCJ inmates (N=79,211) who began serving sentences between September 1, 2006, and August 31, 2007, in any of TDCJ’s 116 facilities throughout the state. The inmates’ history of previous TDCJ incarcerations was determined by examining a comprehensive electronic database containing all TDCJ incarceration records from September 1, 2000, through August 31, 2006. A previous incarceration was defined as an incarceration resulting from a distinct criminal offense; previous incarcerations resulting from parole violations were not included in our analysis. All members of the study cohort underwent standard medical and psychiatric examinations during the intake process. This evaluation lasted approximately 60 minutes and consisted of a detailed medical history, a mental health screening, a physical examination, and a number of laboratory tests. The study was reviewed and approved by the University of Texas Medical Branch Institutional Review Board.
Measures
The study was designed to compare the prevalence of having multiple episodes of incarceration among inmates with any of four types of major psychiatric disorders: major depressive disorder, bipolar disorders, schizophrenia, and nonschizophrenic psychotic disorders. Nonschizophrenic psychotic disorders included schizoaffective disorder, delusional disorder, substance-induced psychosis, and psychotic disorder not otherwise specified. The mental health screening at the time of the intake evaluation was conducted in a standardized fashion across all prison sites by mental health nurses or mental health professionals. The screening consisted of a standardized diagnostic interview and included assessment of the following: display of symptoms of psychiatric disease; history of mental health treatment; current suicidal ideation; prior suicidal gestures; display of unusual behavior; affective distress; and unusual nature of criminal offense. The purpose of the intake screening was to determine whether an inmate should be referred for a formal mental health evaluation. If a referral was made, the evaluation was conducted by master’s-level mental health professionals using a DSM-IV-guided interview structure. A diagnosis of a psychiatric disorder established during this evaluation was based on DSM-IV criteria and recorded in the inmate’s electronic medical record. All incoming inmates who had one of the four types of major psychiatric disorders under study, who reported a history of treatment with psychotropic medication, or who appeared to require such treatment were subsequently referred to a staff psychiatrist or a psychiatric midlevel practitioner for treatment. Diagnoses that were made or confirmed by psychiatric providers were also based on DSM-IV criteria. Approximately 20% of all inmates were referred for psychiatric evaluation during their incarceration. All psychiatric diagnoses used in the analyses in this study were ascertained during the period from September 2006 through August 2007.
All demographic data (age, race/ethnicity, and gender) were based on inmate self-reports and maintained in a systemwide electronic medical record that is routinely updated to ensure that the information reflects the inmates’ current health status. Information on correctional characteristics (criminal offense classification and length of prison sentence) was maintained in a separate electronic database. Criminal offense classification was based on the National Criminal Information Center criminal offense codes associated with the inmates’ current sentence. Inmates who had at least one violent criminal offense (i.e., homicide, kidnapping, sexual assault, robbery assault, and terrorism) were classified as violent; inmates who had no such criminal offenses were classified as nonviolent. The two electronic data sets were linked using a common numeric identification variable.
Statistical Analyses
All statistical analyses were performed with SAS, version 8 (SAS Institute, Cary, N.C.). Logistic regression analysis was used to examine differences in multiple episodes of incarceration across the subgroups and to calculate adjusted prevalence odds ratios and corresponding 95% confidence intervals (CIs). All logistic regression models were adjusted for age, gender, race/ethnicity, criminal offense classification, and length of current prison sentence. Information on at least one of the aforementioned demographic or correctional variables was unavailable in <1% of the study population; inmates with missing data were excluded from the analysis.
Results
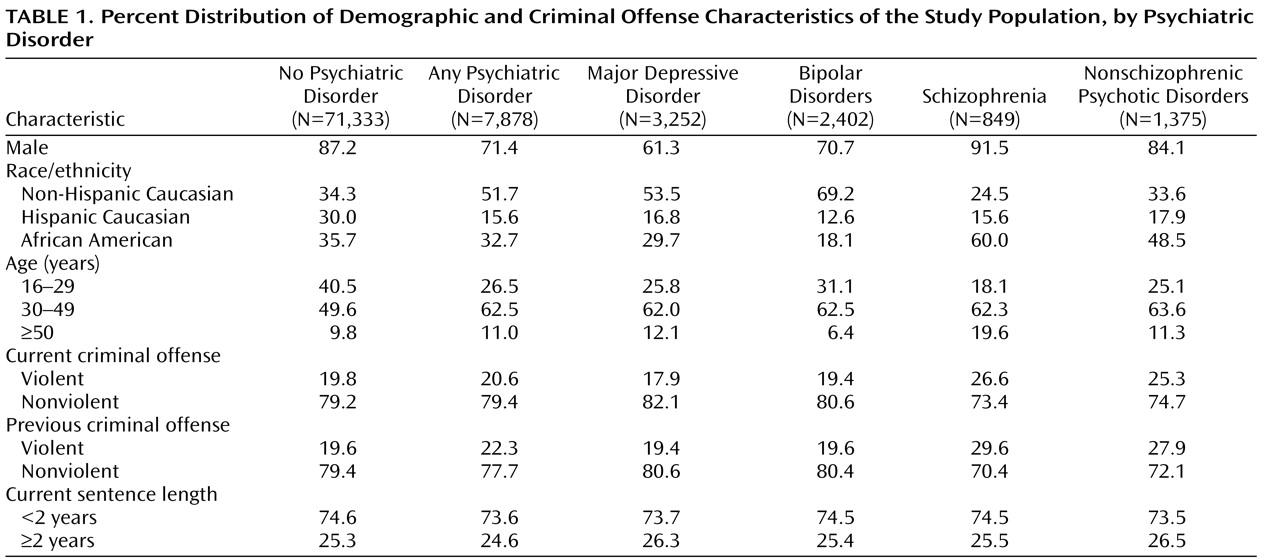
Of the 71,333 inmates in the study cohort who did not have any of the four major types of psychiatric disorders, the vast majority were male (87.2%), were under 50 years old (90.1%), were currently incarcerated for a nonviolent offense (79.2%), had no history of a violent offense during the 2000–2006 period (79.4%), and had a current prison sentence of less than 2 years (60.1%). The three racial/ethnic groups were distributed fairly evenly: 34.3% were non-Hispanic Caucasian, 30.0% were Hispanic Caucasian, and 35.7% were African American. A total of 7,878 inmates were diagnosed with major depressive disorder, a bipolar disorder, schizophrenia, or a nonschizophrenic psychotic disorder. There was substantial variation in several demographic characteristics according to the psychiatric disorders under study (
Table 1 ). Among inmates diagnosed with major depressive disorder and bipolar disorders, females and non-Hispanic Caucasians were overrepresented and Hispanics and African Americans were underrepresented. Among inmates with schizophrenia and nonschizophrenic psychotic disorders, African Americans, inmates age 50 or older, and inmates who had violent offense records (current or previous) were overrepresented.
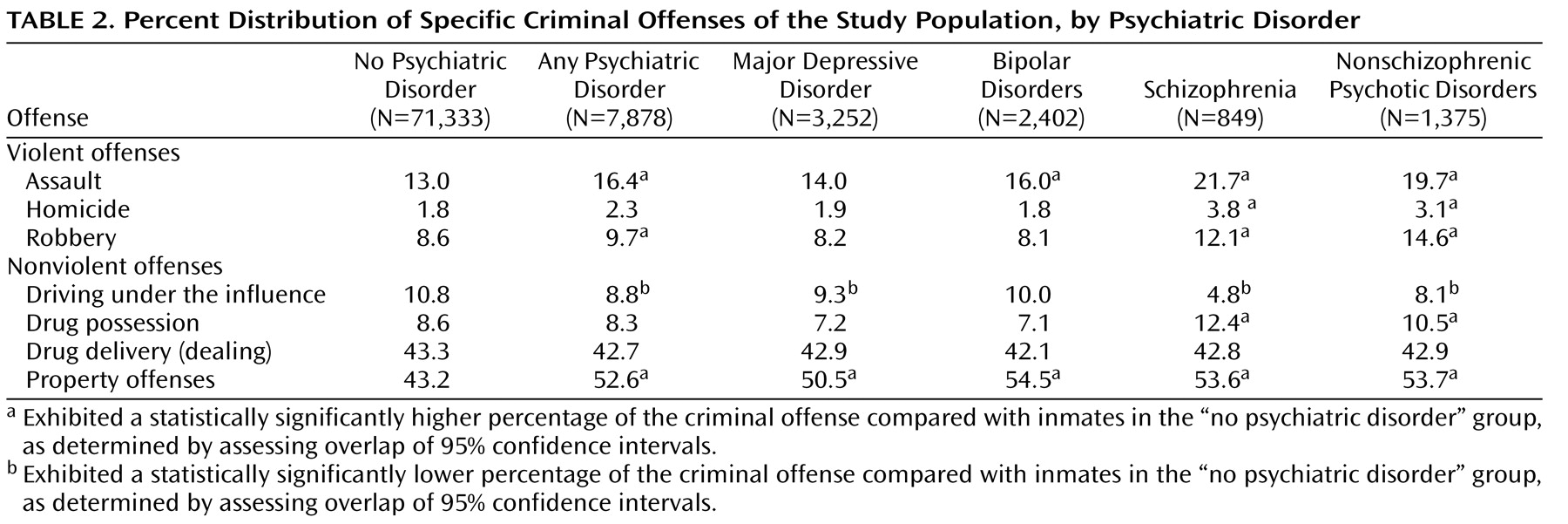
The percentage of specific criminal offenses was calculated according to the four major types of psychiatric disorders (
Table 2 ). Assessment of the major violent offenses showed that, in comparison with inmates who had no psychiatric disorder, those who had any psychiatric disorder, a bipolar disorder, schizophrenia, or a nonschizophrenic psychotic disorder had higher rates of assault; inmates who had schizophrenia or a nonschizophrenic psychotic disorder had higher rates of homicide; and inmates who had any psychiatric disorder, schizophrenia, or a nonschizophrenic psychotic disorder had higher rates of robbery. Assessment of major nonviolent offenses showed that, in comparison with inmates who had no psychiatric disorder, those who had any psychiatric disorder, major depressive disorder, schizophrenia, or a nonschizophrenic psychotic disorder had lower rates of driving under the influence; inmates who had schizophrenia or a nonschizophrenic psychotic disorder had higher rates of drug possession; and inmates in all major psychiatric disorder categories had higher rates of property offenses.
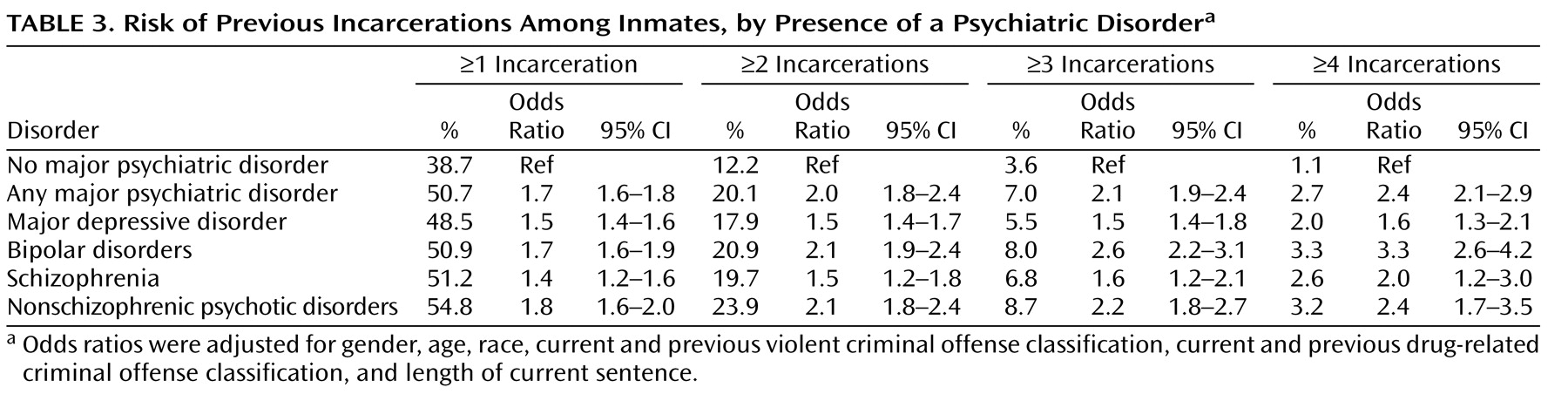
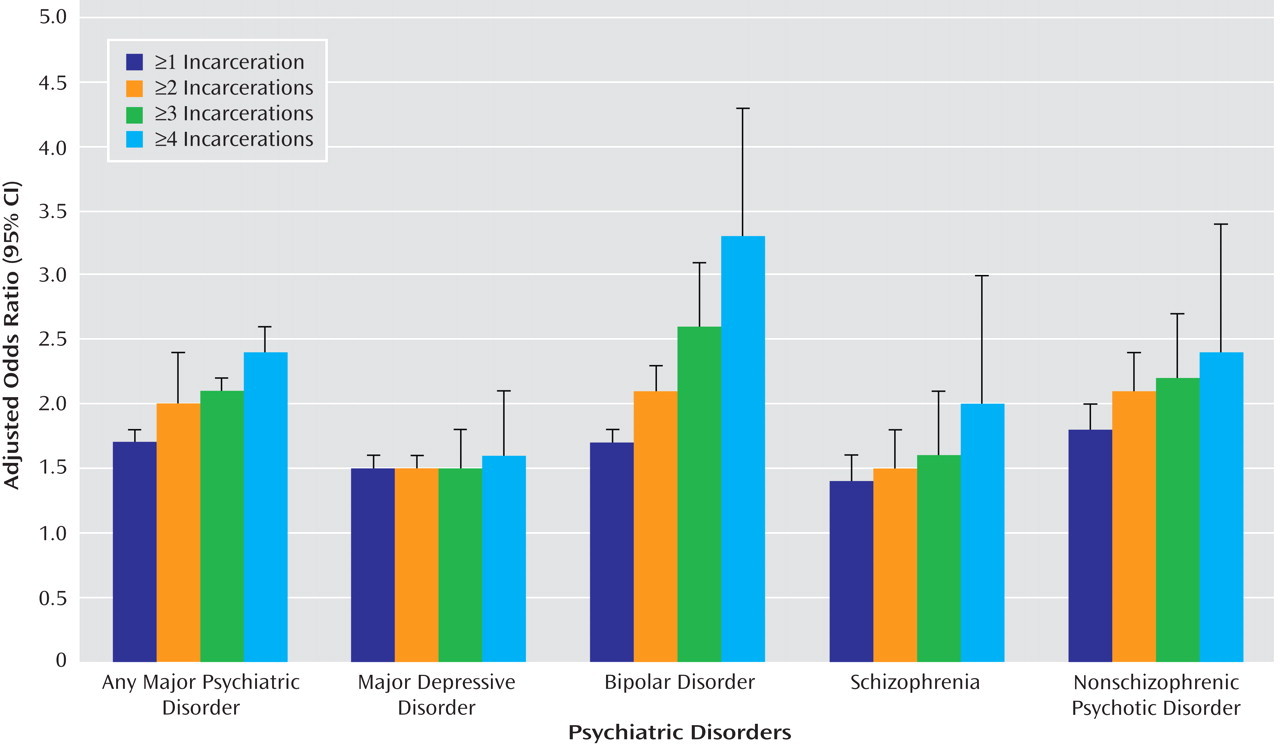
The prevalence of having previous incarcerations was calculated for inmates with each of the four major types of psychiatric disorders, using four different threshold values: ≥1, ≥2, ≥3, and ≥4 incarcerations (
Table 3 ). Odds ratios, adjusted for gender, age, race, current criminal offense classification (violent versus nonviolent), and length of current sentence, were then calculated to assess the risk of each threshold value among each of the four groups of psychiatric disorders. For three of the four categories of psychiatric disorders (bipolar disorders, schizophrenia, nonschizophrenic psychotic disorders), the risk of having multiple incarcerations increased in a stepwise fashion according to the threshold value (
Figure 1 ). For inmates with major depressive disorder, the risk of having previous incarcerations remained relatively stable across all four threshold values.
Discussion
Our study showed that Texas prison inmates with major psychiatric disorders were far more likely to have had previous incarcerations compared with inmates without a serious mental illness. For three of the categories of psychiatric disorders under study (bipolar disorders, schizophrenia, and nonschizophrenic psychotic disorders), this risk increased in a stepwise fashion according to the threshold value for number of incarcerations. The risk of having four or more incarcerations in the 6-year study period was particularly high for inmates with a bipolar disorder. In general, these findings suggest a substantially heightened risk of recidivism among released inmates with mental illness. As a result of the limited availability of community-based mental health services, mass downsizing of state psychiatric institutions, and a legal system with a limited capacity to discern underlying mental health problems, many people with serious mental illness move continuously between crisis hospitalization, homelessness, and the criminal justice system
(10,
15) . To our knowledge, this is the first study to examine the association of psychiatric disorders and multiple episodes of incarceration in an entire state prison population.
Only a handful of studies
(12,
13,
16,
17) involving correctional populations have examined the association between psychiatric disorders and the risk of having a single reincarceration. In contrast to our findings, each of these investigations found that inmates with mental disorders exhibited either comparable
(16,
17) or lower
(12,
13) reincarceration rates for both violent and nonviolent offenses in comparison with inmates without psychiatric disorders. However, a direct comparison of our results with those of earlier studies is of limited value because of differences in sample sizes and methods used to assess psychiatric disorders and recidivism. Feder
(16) examined reincarceration rates among 547 inmates released from the New York State prison system in 1982 and 1983. Lovell et al.
(17) examined reincarceration rates among 337 mentally ill inmates released from Washington State prisons in 1996 and 1997. Teplin et al.
(12) assessed violent repeat offenses among 728 male jail detainees in Chicago in 1983 and 1984. Porporino and Motiuk
(13) examined all repeat offenses among 36 Canadian inmates with a major psychotic disorder and 36 comparison inmates with no psychiatric disorder. In each of these studies, findings of comparable or lower reincarceration rates among mentally ill inmates may be due to several factors. For example, inmates with psychiatric disorders are reported to stay in prison longer than others charged with similar crimes
(18) . The average time served for U.S. inmates with mental illness is 103 months (8.6 years), compared with 88 months (7.3 years) for other prisoners
(19) . Another possible factor may be geographic differences in the efficacy of community-based mental health programs and prison discharge planning programs in preventing criminal recidivism in former inmates
(20) .
Our investigation’s novel findings may be attributable to a number of factors. One possibility is that the criminal justice policies of Texas result in higher rates of incarceration among persons with mental illness. Another is that community-based mental health systems in Texas may have been less effective in diverting persons with severe mental illness from the criminal justice system. However, Texas does have a state-sponsored continuity of care program that links inmates with serious mental illness who are about to be released to treatment resources in their home communities, including halfway houses and outpatient clinics. The program also provides inmates with a 10-day supply of their prescribed psychotropic medications. Unfortunately, few data on inmates’ participation in this program are currently available.
Several limitations should be considered in interpreting our study. We examined only incarcerations within the Texas prison system. If an inmate in our study population was previously incarcerated in another state, the episode was not included in our analysis. However, given the large geographic size of Texas and the limited mobility of our study population, it is unlikely that a substantial proportion of inmates had been incarcerated in another state’s prison system. Second, because relatively less severe psychiatric disorders such as anxiety disorders and axis II disorders are not rigorously evaluated in the TDCJ, during either the initial mental health screening or subsequent medical encounters, we restricted our analyses to four broad categories of severe psychiatric disorders. Additionally, information about a prisoner’s history of substance abuse is maintained in a separate, confidential TDCJ database that was not available for analysis. Thus, our ability to assess the extent to which either less severe psychiatric conditions or substance use disorders contributed, either independently or comorbidly, to repeat incarcerations was limited. Third, this investigation was subject to the selection biases associated with most retrospective study designs. Specifically, inmates who were incarcerated multiple times may have had a greater probability of being diagnosed with a serious mental illness. This bias was probably minimized by the standardized mental health evaluation used at intake and by our decision to restrict our analysis to four categories of the most severe psychiatric disorders.
A fourth limitation of our study was that because of incomplete access to historical incarceration data, we could not fully examine the extent to which the duration of previous incarcerations may have contributed to differential reincarceration rates between inmates with and without these mental illnesses over the 2000–2006 study period. Although it is possible that inmates with psychiatric disorders receive shorter sentences and therefore have greater opportunities to commit new criminal offenses and ultimately to be reincarcerated, this scenario is not supported by previous studies, which have consistently shown that mentally ill persons receive longer prison sentences and have a reduced likelihood of early parole compared with those who are not mentally ill
(13,
19) . These results are consistent with our own findings that TDCJ inmates with psychiatric disorders had a longer mean current prison sentence and were more likely than other inmates to be currently incarcerated for a violent crime. Assuming that these two variables would serve as reasonable proxies for previous prison sentence length, we adjusted for both current prison sentence length and current criminal offense classification in all statistical models and found that their inclusion in the models had only a minimal effect on the outcome of our analyses. Finally, our findings are highly dependent on the reliability and validity of the screening measures, the diagnoses of mental health professionals, and the accuracy of data entry into the electronic medical record. Although TDCJ has policies of universal and standardized medical screening of all inmates at intake, as well as standardized and validated data entry procedures, it is possible that some inmates were misclassified or misdiagnosed and that some data were entered incorrectly.
Despite these limitations, this is the first study to examine the association between major psychiatric disorders and multiple episodes of incarceration within an entire state prison population. Because this investigation was carried out in the nation’s largest state prison system, these findings have a high degree of statistical power and are likely to be generalizable to other U.S. prison systems. It is important to recognize, however, that inmates with mental illness represent a small and distinct segment of the broader population of mentally ill adults in the United States and that the overall contribution of mental illness to criminal activity in our society is small
(21) .
The results of our study highlight the need to pursue alternatives to incarceration of persons with severe mental illness. One of the most promising alternatives is the diversion model, designed to prevent or minimize law enforcement detention of the nonviolent mentally ill
(22,
23) . Based on a foundation of extensive interagency collaboration between mental health, law enforcement, and criminal justice systems, the model draws on a wide range of strategies to divert persons with severe mental illness to appropriate community-based mental health services in lieu of incarceration
(15,
24) .
There are two major types of diversion programs. Prebooking programs, which are designed to resolve psychiatric emergencies without resorting to arrest, generally are based on formal liaisons between law enforcement and mental health personnel
(23,
25) . An example is the crisis intervention team, which utilizes specially trained police officers to redirect individuals with mental illness to treatment instead of the judicial system
(22) . Preliminary data suggest that the crisis intervention team program is associated with lower arrest rates and criminal justice costs than other pre- and postdiversion programs
(22) .
Postbooking programs, as the term implies, attempt to divert mentally ill offenders to community-based services after they have been arrested. In contrast to prebooking programs, the criminal justice system plays a major role in postbooking diversion
(26) . One particularly promising postbooking program is the mental health court, which was designed to divert nonviolent mentally ill individuals from jails and prisons into closely supervised treatment programs
(27,
28) . The number of mental health courts in the United States has increased from two in 1997 to approximately 120 today
(27) . Unlike traditional courts, mental health courts have therapeutic goals, such as increasing treatment adherence, and they are presided over by designated judges
(18,
27) . Preliminary evidence indicates that participation in a mental health court is associated with longer periods without criminal recidivism
(18) . Another emerging diversion strategy is the forensic assertive community treatment model, which relies on 24-hour mobile services and comprehensive outreach modalities, such as mental health and addiction treatment, transportation, economic assistance, and vocational training
(24) .
In addition to diversion strategies, the implementation or expansion of discharge planning or continuity of care programs for mentally ill inmates who are about to be released appears warranted. Ideally, such programs should link released inmates with long-term, community-based outpatient services to help them manage their mental health problems and reduce their risk of recidivism. Besides providing outpatient treatment, there is evidence suggesting that community-based mental health programs should make efforts to ensure that ex-inmates have access to acute psychiatric inpatient treatment for an appropriate duration. For example, one study
(29) found that hospitalizations that are too brief may fail to stabilize escalating psychiatric symptoms and increase the risk of criminal recidivism. Other studies have shown that comorbid substance use among persons with mental illness also increases the risk of reincarceration
(29,
30), suggesting that the inclusion of drug and alcohol screening and treatment in community settings may help reduce the rate of recidivism among mentally ill persons
(29) .
Finally, a substantial proportion of inmates with mental illness are incarcerated for violent crimes (20%–25% in our study), especially felony offenses. Because these individuals are generally ineligible for diversion programs, consideration should be given to the development of alternative correctional facilities that would provide an appropriate clinical environment, including expanded opportunities for monitoring and treatment, for inmates suffering from severe mental illness
(31,
32) .
A recent study by the Pew Center on the States estimated that, for the first time in U.S. history, more than 1 in 100 adults are confined in an American jail or prison at any given time
(14) . This striking statistic does not reflect a parallel increase in crime; rather, it is a culmination of criminal justice policies that send more lawbreakers to prison for longer periods. Although the costs of incarceration have increased dramatically, little progress has been made in reducing the rates of recidivism and reincarceration, particularly among inmates with mental illness
(14) . Hence, our finding that inmates with psychiatric disorders have an increased risk of having multiple incarcerations has important policy implications. Addressing this public health crisis adequately will require the continued development of novel and integrated interventions, such as mental health courts, continuity of care programs, and the development of specialized correctional mental health facilities. Given the scale and complexity of this problem, it is likely that a coordinated effort among criminal justice, mental health, and public health systems will be necessary to reduce the widespread criminalization of the mentally ill in America.