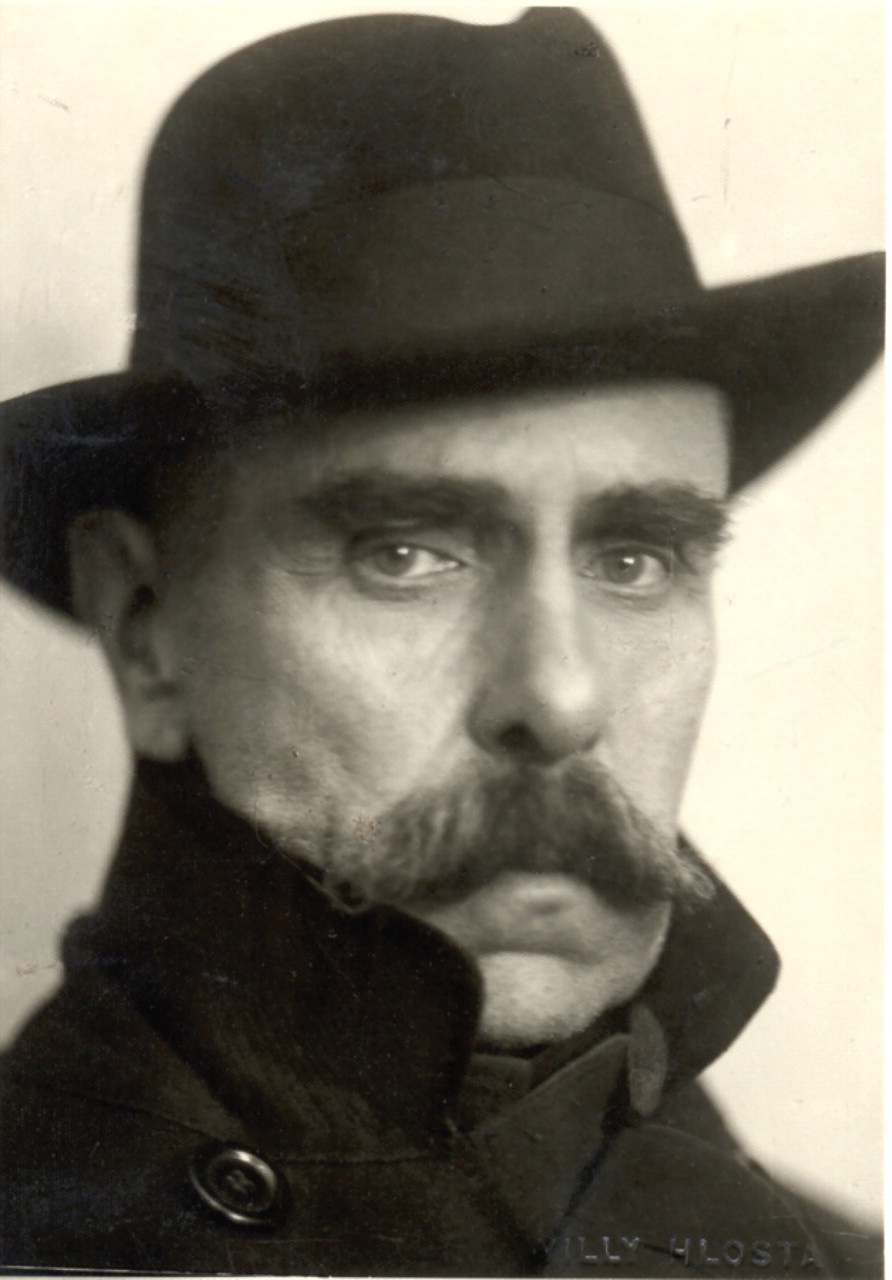
Julius Wagner-Jauregg, the father of fever therapy, retired as director of the Vienna Psychiatric and Neurological Clinic 80 years ago. He was the first psychiatrist to win the Nobel Prize for Medicine and has remained the only psychiatrist to receive the prize for research on mental illness.
Wagner-Jauregg had no previous training in psychiatry when he applied for the assistantship at the first psychiatric clinic in Vienna. In fact, he had initially wanted to specialize in internal medicine, and it was only after being turned down for a job in medicine that he applied for the post in psychiatry
(1,
2) .
Following his appointment at the clinic in Vienna, he noted that people suffering from nervous disorders showed a marked improvement in mental state after contracting febrile illnesses. Others had also reported this, and in 1887 he published a landmark paper that combined a review of the current literature with his own observations (for additional details and historical context, see references 2 and 3).
Further careful study of patients in the 1890s led him to note that those suffering from general paresis of the insane (GPI, also known as paralytic dementia) recovered during attacks of erysipelas and tuberculosis. At this time, GPI accounted for 15% of the patients confined to mental hospitals, and it was thought to be incurable—often starting with psychotic symptoms and generally ending in seizures, dementia, paralysis, and death within 3 to 4 years
(1,
4) .
He attributed their recovery to the fever associated with the infection, and he developed the idea that infection could be a relatively safe way to induce fever and treat GPI. He initially tried to induce fever by using erysipelas and tuberculin but with disappointing results
(2,
3) . He thought this was because the fever was not high enough, and he had the idea of using malaria to cause a higher fever. However, he did not have a ready source of malaria until World War I. At this time a soldier who had caught malaria fighting in the Crimea was admitted to Wagner-Jauregg’s ward for treatment of shell shock. The soldier’s blood provided a source of malaria to test Wagner-Jauregg’s ideas.
On June 14, 1917, he conducted a small-scale study, injecting malarial blood into nine patients with GPI
(3) . Quinine was withheld until there had been at least seven attacks of fever. The results were striking: six patients made a good recovery and were able to return to work (although four of the six went on to experience relapses over the ensuing years)
(1,
3) .
Wagner-Jauregg received the Nobel Prize in 1927 for his work on fever therapy and retired the next year. Fever therapy was not without its risks; death occurred in 2%–13% of cases, depending on severity
(5) . However, it was effective, leading to remission in 15%–40% of cases and improvement in over 50%, depending on the hospital and stage of illness (for full review, see reference 5). As a result, it was widely used until after Wagner-Jauregg’s death, when it was superseded by penicillin
(1,
3,
4) .