Traumatic injury is a common occurrence, with over 2 million people hospitalized in the United States each year following nonfatal injuries (
1). Traumatic injury has been shown to be the leading cause of trauma-related psychiatric disorders and hence represents a major public health issue (
2,
3). Most attention has focused on the incidence of posttraumatic stress disorder (PTSD) and depression after traumatic injury. Studies indicate that 10%–20% of traumatic injury survivors develop PTSD (
4,
5) and 9%–15% develop major depressive disorder (
4,
6). Our understanding of the psychiatric impact of traumatic injury has been limited by several factors, however. The focus on PTSD and depression has resulted in a relative neglect of the broad range of psychiatric disorders that can arise after traumatic injury. Some small studies suggest increased rates of anxiety and substance use disorders after traumatic injury (
4,
7,
8), but most studies indicate that psychiatric disorders after trauma are typically comorbid with PTSD (
9). There remains an outstanding need to evaluate the full range of psychiatric sequelae to traumatic injury.
Another critical issue in the study of traumatic injury has to do with the potential role of mild traumatic brain injury (TBI), which involves transient diminished consciousness following an insult to the brain. Mild TBI represents a major public health issue; the incidence of hospitalized adult patients with mild TBI ranges from 100 to 300/100,000 per year (
10). The role of TBI in posttraumatic psychiatric illness has been controversial. Although there is some evidence of comparable rates of PTSD in mild TBI and non-TBI samples (
11), some commentators have suggested that impaired consciousness after TBI limits awareness of the traumatic nature of the injury and thus is protective against subsequent PTSD (
12). Consistent with this proposal, there is evidence that poorer memory of the traumatic injury after mild TBI is protective against PTSD (
13,
14). Several large-scale studies of psychiatric illness associated with TBI have been reported (
15–
17). For example, based on a large-scale study of 939 health plan members, Fann and colleagues (
15) reported that patients with mild TBI were 2.8 times more likely to develop a psychiatric disorder than patients with no TBI. These studies have been limited, however, by reliance on self-report of brain injury (
17), on medical records rather than on standardized psychiatric assessments (
15), and on retrospective reporting rather than prospective assessments at the time of injury (
16). Systematic reviews have noted a trend for increased rates of psychiatric disorders after mild TBI but have emphasized the pressing need for multicenter studies to assess this relationship prospectively using standardized instruments and indexing relevant risk factors (
18,
19).
These issues require proper attention because of the potential impact of psychiatric illness on functioning following traumatic injury. In this study, which was part of the National Health and Medical Research Council-funded Injury Vulnerability Study, we prospectively studied admissions to four large level I trauma centers following traumatic injury to index 1) the development of new psychiatric disorders after traumatic injury, 2) the influence of mild TBI on the risk of developing psychiatric illness, 3) functional impairment associated with any psychiatric illness, and 4) consequent mental health service utilization.
Method
Participants
Weekday admissions to four level I trauma centers across three states in Australia were recruited into the study between April 2004 and February 2006. The study was approved by the Research and Ethics Committee at each hospital. Patients who met entry criteria were randomly selected using an automated random selection procedure with stratification by length of stay. The researchers estimated each patient's length of stay on admission, classifying it as long, medium, or short. Each day, a patient list was created from which participants were randomly selected. The names of participants classified as short stay appeared three times on the list, those classified as medium stay appeared twice, and those classified as long stay appeared once. Thus, the increased likelihood of long-stay patients being selected because of the length of time they appeared on the daily lists was counterbalanced by the frequency with which short-stay patients appeared on the lists. This approach was adopted to ensure that we did not differentially recruit patients who had longer hospital stays because they may be more accessible.
Inclusion criteria were hospital admission of more than 24 hours following traumatic injury, age between 16 and 70 years, and ability to understand and speak English proficiently. Patients were excluded if they had moderate or severe brain injury (defined as loss of consciousness of greater than 30 minutes or a Glasgow Coma Scale score less than 13), were currently psychotic or suicidal, were non-Australian visitors, or were under police guard. Mild TBI was defined by the ICD-9 requirement of documented injury to the head, loss of consciousness for less than 30 minutes, and no focal neurological deficit or intracranial complications (
20).
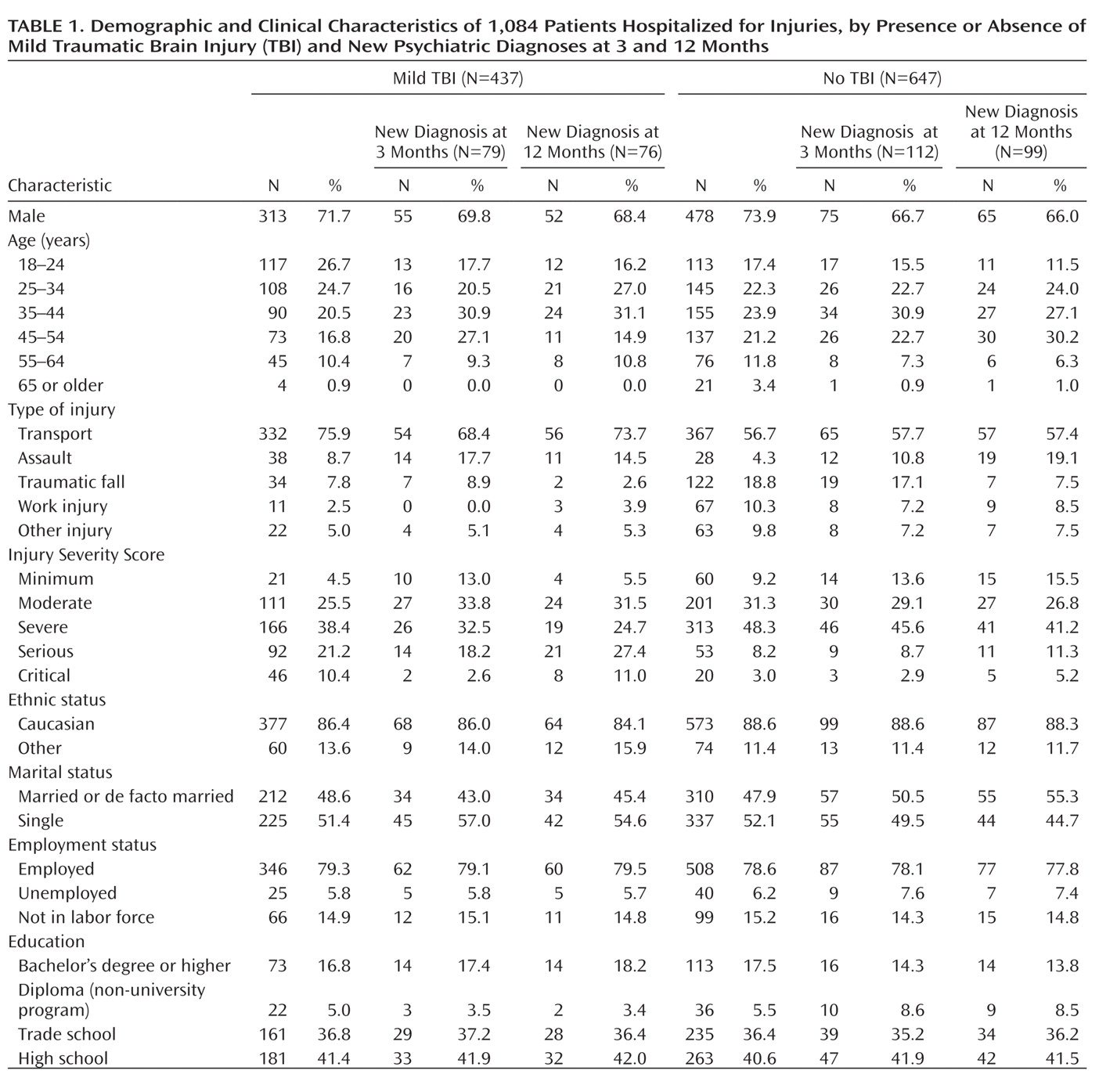
Of 1,477 trauma patients who met inclusion criteria, 1,084 (73%) agreed to participate and completed the initial assessment. Of these, 437 (40%) experienced a mild TBI (
Table 1). More patients with a mild TBI than with no TBI suffered a motor vehicle accident (75.9% compared with 56.7%; χ
2=40.59, df=1, p<0.0001). Patients with a mild TBI had higher Injury Severity Scores (
21) than patients with no TBI (mean=12.94 [SD=8.53] compared with mean=8.71 [SD=6.44]; t=8.9, df=1045, p<0.0001). There was no difference between patients with mild TBI and those with no TBI in number of days spent in hospital (mean=12.78 days [SD=13.56] compared with mean=11.79 days [SD=12.10]). Patients who declined to participate in the study did not differ from participants in gender, length of hospital admission, Injury Severity Score, or age.
At the 3-month follow-up assessment, 152 patients could not be contacted or declined to participate; 932 were interviewed by telephone, representing 86% of the initial sample, and 858 completed the self-report measures described below. Patients who participated in the 3-month follow-up assessment did not differ from those who did not participate in terms of gender, length of hospital stay, or Injury Severity Score. Participants lost to follow-up were younger on average than those who were retained (mean=35.68 years [SD=13.44] compared with mean=38.32 years [SD=13.55]; t=2.31, df=1088, p=0.02).
At the 12-month follow-up assessment, 817 participants completed the assessment, representing 75% of the initial sample, and 759 completed the self-report measures. Patients who participated in the 12-month follow-up assessment did not differ from those who did not participate in terms of gender or length of hospital stay. Dropouts had a lower Injury Severity Score (mean=9.32 [SD=6.73] compared with mean=10.92 [SD=7.95]; t=2.87, df=1054, p=0.004) and were younger on average (mean age=35.44 years [SD=13.10] compared with mean age=38.79 years [SD=13.61]; t=3.60, df=1088, p=0.001) than those who did participate.
Measures
The Mini International Neuropsychiatric Interview, version 5.5 (
22), a brief structured diagnostic interview based on DSM-IV and ICD-10 criteria, was used to assess lifetime psychiatric disorders and psychiatric disorders at 3 and 12 months. We used this instrument to identify major depressive episode, panic disorder, agoraphobia, social phobia, obsessive-compulsive disorder, generalized anxiety disorder, alcohol abuse and dependence, and marijuana abuse and dependence. We also used it to assess lifetime PTSD in hospital, but at the 3- and 12-month follow-ups, PTSD was assessed using the Clinician-Administered PTSD Scale–IV (CAPS) (
23), a structured clinical interview with good sensitivity (0.84) and specificity (0.95) relative to the Structured Clinical Interview for DSM-IV diagnosis of PTSD, as well as sound test-retest reliability (0.90).
The World Health Organization Quality of Life–Abbreviated Version scale (
24) assesses quality of life across four domains of functioning: physical (daily living, pain, work capacity), psychological (mood, self-esteem, concentration), social (personal relationships, social support, sexual activity), and environment (financial resources, health care, home environment). It demonstrates good discriminant validity, content validity, internal consistency, and test-retest reliability (
25). Poor functional impairment was defined on the basis of Australian norms for each scale of the instrument (
26).
At the 3- and 12-month assessments, pain levels were indexed by asking patients to indicate on a visual analogue scale their worst level of pain in the past 2 weeks (range, 1=no pain at all to 20=worst pain possible). Mental health service use was assessed by asking participants whether they had consulted a psychiatrist, psychologist, social worker, counselor, or other mental health care professional in the month prior to the 12-month assessment. This time frame was adopted to index treatment-seeking patterns for conditions that patients currently experienced.
Procedure
After patients provided written informed consent, they were assessed prior to discharge, on average 7.2 days (SD=9.6) after injury. They completed the Mini International Neuropsychiatric Interview to assess lifetime and current psychiatric disorders. Information on demographic characteristics, hospital admission, and injury-related factors was obtained from medical records. Three months and 12 months after their injury, participants were contacted by telephone and completed the Mini International Neuropsychiatric Interview and the CAPS to assess current PTSD related to the original traumatic injury and other psychiatric disorders. Self-report questionnaire booklets containing the World Health Organization Quality of Life–Abbreviated Version scale and questions about mental health service use were sent to participants to complete. All assessments were audiorecorded to assess adherence to the protocol. Five percent of all Mini International Neuropsychiatric Interview and CAPS interviews were rescored blind to the original scoring to test interrater reliability. Overall, the diagnostic consistency for PTSD with the CAPS was 1.00 at 3 months and 0.98 at 12 months, and with the Mini International Neuropsychiatric Interview across all diagnoses it was 0.99 at 3 months and 1.00 at 12 months.
Data Analysis
We computed rates of all observed psychiatric disorders and new posttraumatic psychiatric disorders by excluding patients who had the same psychiatric disorder at any time prior to the traumatic injury. To ensure that reported PTSD symptoms were secondary to the traumatic injury rather than any other traumatic event, we restricted new cases of PTSD to those in which symptoms were anchored to the traumatic injury. Associations between categorical variables were subjected to chi-square tests, and Fisher's exact test was used when expected numbers in cells were less than 5. Logistic regression analyses were conducted with type of traumatic injury, Injury Severity Score, age, psychiatric history, and pain ratings at the time of assessment entered prior to entering mild TBI status as a predictor of subsequent psychiatric illness, and adjusted odds ratios were calculated to determine the influence of sustaining a mild TBI on development of new psychiatric disorders.
Results
Incidence of Psychiatric Disorders
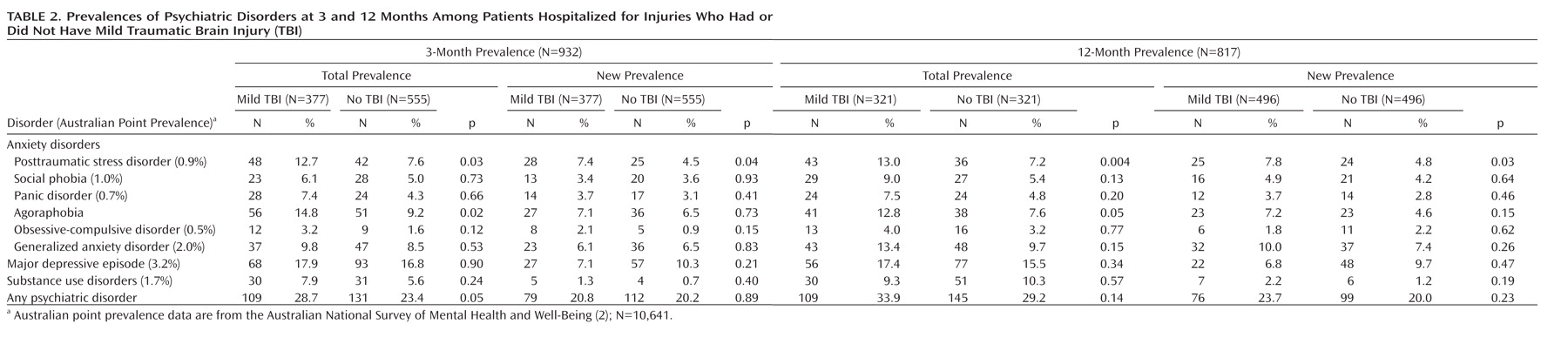
Table 2 presents the rates of all psychiatric disorders for patients with mild TBI and patients without TBI at 3 and 12 months, as well as the rates excluding patients who had a lifetime history of the disorder and the Australian prevalence rates for these disorders. A total of 254 patients (31.0%) had a psychiatric diagnosis at 12 months (patients with mild TBI, 34.3%; patients with no TBI, 29.4%). The most common diagnosis at 12 months was depression (16.3%), followed by generalized anxiety disorder (11.1%), substance abuse (9.9%), PTSD (9.7%), agoraphobia (9.7%), social phobia (6.9%), panic disorder (5.9%), and obsessive-compulsive disorder (3.5%). Overall, 175 patients (22.2%) had a psychiatric diagnosis at 12 months that they had never had before (patients with mild TBI, 24.8%; patients with no TBI, 20.5%). The most common new diagnosis at 12 months was depression (11.6%), followed by generalized anxiety disorder (9.5%), PTSD (7.0%), agoraphobia (6.5%), social phobia (5.0%), panic disorder (3.5%), obsessive-compulsive disorder (2.3%), and substance abuse (2.5%).
There was considerable change in diagnostic status over time; only 59.9% of those with an anxiety disorder at 12 months had an anxiety disorder at 3 months, 54.7% of those with depression at 12 months had depression at 3 months, and 34.6% of those with substance use disorder at 12 months had this condition at 3 months.
In terms of psychiatric comorbidity, it is noteworthy that 68.9% of all patients with psychiatric diagnoses at 12 months did not have a diagnosis of PTSD. Only 8.9% of PTSD cases at 12 months occurred without any comorbid disorders. Major depression (54.8%), anxiety disorders (61.9%), and substance use disorders (84.0%) occurred more often without PTSD than with PTSD. Major depression occurred without comorbid diagnoses in 24.2% of depression cases, non-PTSD anxiety disorders occurred without comorbid diagnoses in 32.3% of anxiety cases, and substance use disorders occurred without comorbid diagnoses in 54.3% of substance use cases. More patients with a new psychiatric disorder (N=94, 38.4%) were involved in litigation at 12 months than those without a new disorder (N=95, 17.6%; χ2=39.79, N=785, p=0.001; odds ratio=1.96, 95% CI=1.61–2.39).
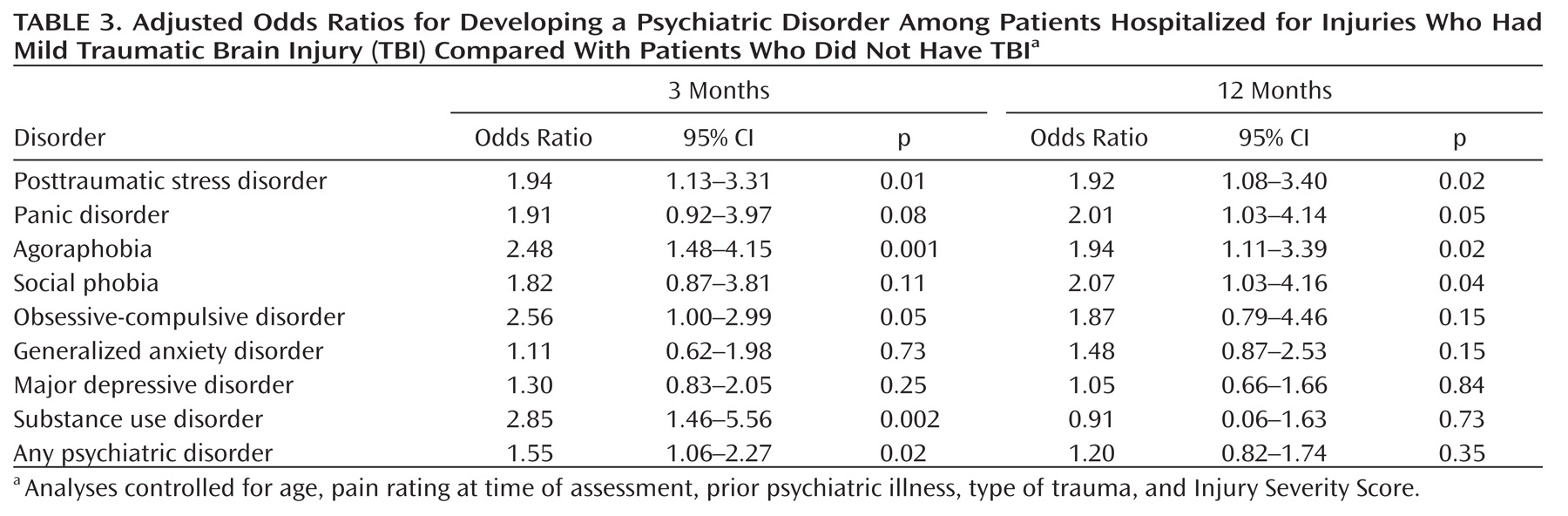
Table 3 presents the adjusted odds ratios indicating the risk of developing a psychiatric disorder if mild TBI was present (with an adjusted alpha of 0.005 to accommodate multiple comparisons). After controlling for the effects of type of traumatic injury, Injury Severity Score, pain rating at time of assessment, and presence of a pretrauma psychiatric history, patients were more likely to develop PTSD, panic disorder, agoraphobia, and social phobia at 12 months if they had sustained a mild TBI than if they had sustained injuries that did not involve a mild TBI. Injury severity was not correlated with PTSD severity at 12 months.
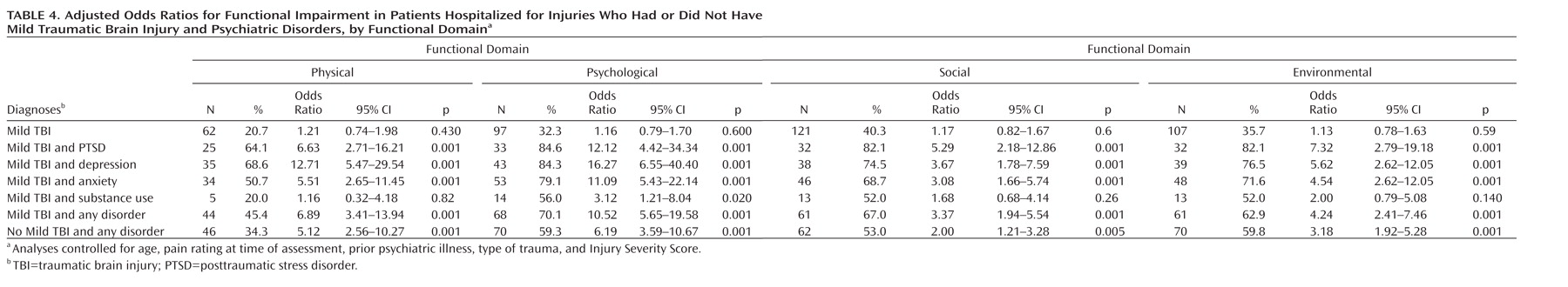
Functional Impairment
Table 4 presents the percentages of patients who reported functional impairment on the World Health Organization Quality of Life–Abbreviated Version scale and the adjusted odds ratios for having impairment with mild TBI and psychiatric disorders relative to patients with no TBI or psychiatric disorders after controlling for type of traumatic injury, Injury Severity Score, age, pain rating at time of assessment, and prior psychiatric illness. Having a mild TBI did not increase the likelihood of suffering functional impairment in any of the four domains. In contrast, the combination of sustaining a mild TBI and having any psychiatric disorder at 12 months resulted in a marked increase in functional impairment. Injured patients who developed any psychiatric disorder 12 months after the injury were two to four times more likely to suffer functional impairment; the likelihood of suffering functional impairment was comparable across patients with a psychiatric disorder who did and did not sustain a mild TBI.
To index the potential impact of impairment on subsequent psychiatric illness, we calculated the likelihood of developing a psychiatric disorder at 12 months if functional impairment (defined by the World Health Organization Quality of Life–Abbreviated Version scale) was present at 3 months, controlling for type of traumatic injury, Injury Severity Score, age, prior psychiatric illness, pain rating at time of assessment, and psychiatric illness at 3 months. This analysis revealed that participants were more likely to develop a psychiatric disorder at 12 months if they had physical (odds ratio=3.58, 95% CI=2.05–6.25), psychological (odds ratio=5.08, 95% CI=3.23–8.00), social (odds ratio=2.06, 95% CI=1.36–3.11), or environmental (odds ratio=2.89, 95% CI=1.89–4.41) impairment in functioning at 3 months.
Mental Health Service Utilization
Only a minority of injury survivors (33.0%) who met criteria for a psychiatric disorder at 12 months were receiving mental health treatment for their condition (PTSD, 47.7%; depression, 41.2%; anxiety disorder, 37.7%; substance use disorder, 20.9%); 7.7% of patients who did not meet criteria for a psychiatric disorder sought mental health treatment in the month prior to the 12-month assessment. For patients with a psychiatric disorder, more patients with a mild TBI (21.4%) received mental health treatment in the month prior to the 12-month assessment than patients without a TBI (11.5%; χ2=13.15, N=741, p=0.001; odds ratio=2.09, 95% CI=1.39–3.12).
Discussion
Twelve months after traumatic injury, 23% of patients developed a psychiatric disorder that they had never had before. The most common new disorders were depression (9%), generalized anxiety disorder (9%), PTSD (6%), and agoraphobia (6%). Whereas these rates are lower than in populations exposed to violent traumatic events, such as terrorist attacks (
9,
27), they are higher than rates observed in the Australian population. Our overall rates of each disorder at 12 months are consistent with rates of PTSD and depression in small studies of traumatic injury survivors (
4–
6,
28,
29). A novel finding was that PTSD was not the most prevalent psychiatric disorder after traumatic injury, and when PTSD did occur, it typically occurred in the presence of another disorder. This finding challenges notions that PTSD is always the primary psychiatric disorder after trauma. Although PTSD is the predominant disorder after many types of traumatic events that involve marked violence (
9), it appears that a broader range of disorders affect people after traumatic injury. Although this study is limited by the lack of a non-trauma-exposed comparison group, the risk of psychiatric illness following traumatic injury is indicated by the observation that the rates of psychiatric disorders in this cohort were at least five times greater than the point prevalence yielded by general population studies in Australia (
2).
Patients with mild TBI were twice as likely to develop PTSD, panic disorder, agoraphobia, or social phobia than patients without TBI. Several explanations may account for this pattern. First, biological models of anxiety disorder posit that fear is mediated by impaired regulation of the amygdala by the ventral medial prefrontal cortex (
30). Damage to the frontal regions of the brain is common in mild TBI; this damage may render these patients more vulnerable to anxiety and depression because the neural networks required to regulate emotions may be compromised (
31). Closed head injury can also result in damage to the hippocampus and amygdala, which are also implicated in anxiety disorders (
32). The observed pattern suggests that the effects of mild TBI may interact with the stress associated with traumatic injury. It is interesting that this pattern was not evident in relation to the development of depression or generalized anxiety disorder; it is possible that disorders that are more affected by fear circuitry networks involving the medial prefrontal cortex and amygdala are more prone to adverse effects of mild TBI than depressive responses (
33). This interaction may explain why mild TBI following nontraumatic injuries (e.g., sports injuries) does not typically result in anxiety disorders. We also note that mild TBI was associated with greater injury severity and with motor vehicle accidents; although we controlled for these factors, it is possible that extraneous factors associated with mild TBI contributed to higher rates of anxiety disorders, so this finding should be considered tentative until it is replicated in future studies.
Although previous studies have reported decreased quality of life following mild TBI (
34), this study provides evidence that sustaining a mild TBI does not directly lead to greater functional impairment after traumatic injury. The likelihood of functional impairment increased significantly in patients with psychiatric disorders, regardless of the presence of mild TBI. This finding accords with recent evidence that mild TBI does not predict subsequent health problems in military personnel after controlling for the effects of PTSD and depression (
35,
36). Comparisons between the present study and recent military studies must be qualified, however, given differing approaches to assessing mild TBI. In contrast to the criteria we used, the current military screening protocol identifies a mild TBI if an individual endorses any questions concerning losing consciousness, being dazed, or not recalling the injury (
35).
Rates of psychiatric disorders did not decrease between 3 months and 12 months after the traumatic injury. Although this finding contrasts with many studies that suggest that PTSD gradually remits over time (
37), the pattern is consistent with evidence that rates of psychiatric disorders may be maintained or even increase over time after combat in military settings (
38) and after massive disasters in civilian settings (
39). These observations have been attributed to the persistent stressors that occur in the aftermath of these traumatic events, which may erode the resources available to manage the adverse consequences (
40). In addition to ongoing stressors that are known to compound posttraumatic adjustment (
41), ongoing problems directly attributable to the injury may add to the maintenance of psychiatric disorders throughout the first year. This interpretation is supported by our observation that impairment at 3 months predicted psychiatric illness at 12 months, even after controlling for psychiatric illness at 3 months. Whereas rates of anxiety and depressive disorders remained constant over time, approximately half of participants with either an anxiety or a depressive disorder at 12 months did not have the disorder at 3 months. This pattern may reflect the possibility that some people who meet criteria at one time become subsyndromal (or vice versa) over time. Alternatively, it may suggest significant change in the psychological responses of people throughout the initial year after traumatic injury.
Only a minority of patients (33%) with a psychiatric disorder sought mental health treatment in the month prior to the 12-month assessment. This finding is consistent with the general observation that most people with mental disorders do not seek mental health assistance after trauma (
42). The finding that patients with mild TBI sought mental health services more often than patients without TBI may reflect a tendency for people who sustain a mild TBI to receive more health service attention. We asked patients if they had received mental health assistance in the previous month, and it is possible that they consulted mental health professionals prior to the last month. Overall, this finding raises concerns about the limited professional assistance given to traumatically injured people with psychiatric disorders.
Our follow-up clinical assessments were conducted via telephone rather than in a face-to-face format; however, comparisons indicate that telephone and personal interviews have high levels of agreement (
43). Our design did not allow us to determine the extent to which psychiatric disorders contribute to impaired quality of life or vice versa. The fact that patients who did not participate in the follow-up were on average younger and less severely injured than those who did may have skewed the findings since it is possible that these characteristics presaged a better prognosis. Although it is understandable that patients with psychiatric disorders may be likely to seek compensation, there is a possibility that litigation-seeking may contribute to patients reporting the presence of psychiatric illness. We also note that the sample focused on patients who were admitted to hospitals and were severely injured; it is possible that rates of psychiatric disorders are not as high for patients with less severe injuries who are treated in emergency departments and discharged. Finally, our approach of reporting new cases of each disorder may be overly conservative because there is evidence that prior PTSD is a significant risk factor for subsequent onset of PTSD (
44).
This study highlights the significant mental health needs experienced by about one-third of survivors of traumatic injury. It is apparent that public health initiatives are needed to address the huge mental health burden caused by the psychiatric effects of such injuries. New approaches that facilitate early identification of emergent psychiatric disorders and prompt early interventions to prevent psychiatric illness might facilitate optimal recovery from traumatic injuries.