In recent years, the global burden of chronic lifestyle-mediated, noncommunicable diseases, such as cardiovascular disease, obesity, and type 2 diabetes, has become substantial, largely owing to changes in the dietary and exercise habits of populations in the developed and developing world (
1). Depression and anxiety are also highly prevalent chronic illnesses (
2,
3), yet while diet and nutrition modulate biological processes underpinning depressive illnesses (
4), such as inflammation (
5), brain plasticity and function (
6,
7), the stress response system (
8), and oxidative processes (
9), psychiatry lacks evidence-based primary prevention and treatment strategies based on dietary modification.
Previous studies regarding the association between diet and depressive illness have focused on individual nutrients or food groups (for instance, see references
10–
12). However, studying individual nutrients or foods may provide an incomplete picture of the relationship between diet and mental health, given the complex interactions among nutrients in our daily diets (
13). Overall dietary intake is better assessed by using a composite measure, such as a dietary quality score derived from recommended national diet guidelines or dietary patterns as derived from factor analyses (
13). The aim of this study was thus to examine the cross-sectional association of habitual diet quality and the high-prevalence mental disorders in an epidemiological study of Australian women. We hypothesized that a better diet quality would be associated with a lower likelihood of depressive and anxiety disorders and with fewer psychological symptoms.
Method
Geelong Osteoporosis Study
The Geelong Osteoporosis Study is a large epidemiological study involving women selected from compulsory Australian Commonwealth electoral rolls for the Barwon Statistical Division. An age-stratified, randomly selected population-based sample of 1,494 women (ages 20–94 years) was recruited between 1994 and 1997, with participation of 77.1%. These women have continued to return for biennial follow-up assessments. Between 2004 and 2008, 881 of the original participants returned for a 10-year follow-up appointment, and the response rate among eligible women was 82.1%. An additional sample of women ages 20–29 years was recruited between 2004 and 2008, with a response rate of 70.9%. This allowed for continuing investigation in the full adult age range. Of the 1,127 women who participated in the 10-year follow-up, participants for whom psychiatric or dietary data were not available at the time of the study (N=81) were excluded from the analyses, resulting in a sample of 1,046 women ages 20–93 years available for analysis. The Barwon Health Human Research Ethics Committee approved the study, and written informed consent was obtained from all participants.
Dietary Assessment
Habitual diet was assessed by using the Cancer Council Victoria dietary questionnaire (
14). This is a comprehensive food frequency questionnaire, validated for assessing habitual dietary intake in the Australian population
15). This questionnaire reports the participant's usual consumption of 74 foods and six alcoholic beverages over the preceding 12 months on a 10-point frequency scale. Additional questions are asked about the type of breads, dairy products, and fat spreads used. By using the estimated portion sizes and frequencies, the intake of each food was converted to daily equivalents for statistical analyses. Nutrient intakes, including energy, were computed from the dietary data by means of the nutrient composition tables in the NUTTAB95 database (Food Standards Australia New Zealand, Canberra, 1995).
Psychiatric Assessments
The Structured Clinical Interview for DSM-IV-TR Research Version, Non-Patient Edition (SCID-I/NP) (
16), was the primary diagnostic instrument for mental disorders. Diagnoses of current major depressive disorder, dysthymia, and anxiety disorders were our outcomes of interest, as they have the highest prevalences. Researchers trained in psychology and administration of the SCID-I/NP (F.N.J., L.J.W.) conducted these interviews. Psychological symptoms were measured with the 12-item version of the General Health Questionnaire (GHQ-12) (
17). This is a well-established screening instrument designed to detect nonpsychotic psychiatric disorders in people in community and medical settings by means of a 12-item self-report questionnaire about the respondent's assessment of his or her present state.
Covariates
Socioeconomic status was determined by using scores on the Socioeconomic Index for Areas (
18) based on the 2006 Australian Bureau of Statistics census data. It was decided a priori to use one of the included measures, the Index of Relative Socioeconomic Advantage and Disadvantage, which accounts for high and low income and the type of occupation, from unskilled employment to professional positions. A low score on this index identifies the most disadvantaged (quintile 1), and a high score identifies the most advantaged (quintile 5). Information regarding the highest educational level attained was derived from baseline assessments and comprised four categories, from primary schooling only (score=1) to university or other tertiary qualification (score=4). Physical activity was assessed by self-report questionnaire and ranged from confined to chair or bed or having limited activity throughout the home (score=1) to very active (score=4). Alcohol consumption in grams per day was ascertained from the dietary questionnaire and was subsequently categorized according to 2001 recommendations for women (
19) as the following: zero consumption (score=1), 1–14 standard drinks per week (score=2), or 15 or more standard drinks per week (score=3). The presence or absence of current cigarette smoking was self-reported. Height was measured to the nearest 0.1 cm, and body weight was measured to the nearest 0.1 kg. Body mass index was calculated from these measurements as weight divided by height squared (kg/m
2).
Exposure Variables
Dietary pattern
A factor analysis was conducted to identify dietary patterns. In this approach, 100 food and alcohol items were entered into the factor analysis, and a principal components method with varimax rotation was used. Items with loadings of less than 0.2 on all factors were not retained, allowing for a clearer factor set. The scree plot of eigenvalues indicated that there were three dietary factors—two main factors and a smaller third factor—explaining approximately 14% of the variance in dietary intakes. These three factors were retained as variables in the data set and named, respectively, "traditional," "western," and "modern." A traditional dietary pattern comprised mainly vegetables, fruit, beef, lamb, fish, and whole-grain foods, while a western pattern comprised foods such as meat pies, processed meats, pizza, chips, hamburgers, white bread, sugar, flavored milk drinks, and beer. A modern pattern consisted of foods such as fruits and salads plus fish, tofu, beans, nuts, yogurt, and red wine. High factor scores indicate greater consumption of these types of foods, and low scores indicate lower consumption.
Diet quality score
A diet quality score was derived from the dietary questionnaire, based on Australian national guidelines for healthy eating (
20) and on an algorithm recently developed and tested in a large Australian population of middle-aged women (
21). This scoring method assigns points for the consumption of desirable foods at the recommended levels; for example, a point is assigned for the consumption of at least two servings of fruit a day, at least four servings of vegetables per day, red meat consumption one to five times per week, use of low-fat dairy products, and use of high-fiber, whole-grain, rye, or multigrain breads. In addition, a maximum of two points was assigned for alcohol consumption at the recommended levels (
19).
Statistical Analysis
Differences in characteristics between subjects with and without categorical diagnoses of depressive and/or anxiety disorders according to the SCID-I/NP were tested by using the Mann-Whitney U test or the chi-square test. Diet quality and dietary factor scores were normally distributed, but GHQ-12 scores were positively skewed and were normalized by using a natural log transformation. All exposure variables and GHQ-12 scores were subsequently standardized by using z-scores and were expressed as standard deviation units.
Multivariate linear regression analyses were used to assess the relationship of the exposure variables of interest and GHQ-12 scores. Logistic regression models were developed to estimate odds ratios with 95% confidence intervals for the outcomes of current major depressive disorder/dysthymia and anxiety disorders. Diet quality scores and dietary factor scores (entered simultaneously) were the exposure variables of interest. For each analysis, the following covariates were entered sequentially in order to test their contribution to the mental health outcomes: age, socioeconomic factors (Index of Relative Socioeconomic Advantage and Disadvantage score and education), health behaviors (physical activity, alcohol consumption, and smoking), and energy intake (for dietary factor scores only). Body mass index was also tested in the models as an explanatory variable. These models took into account potential nonlinear associations and interactions.
There were no missing data for the dietary variables. There were missing data for GHQ-12 scores (N=23), and listwise exclusions were used when GHQ-12 score was the outcome variable, resulting in a sample of 1,023 women for these analyses. There were 24 participants with missing data for body mass index. There were no missing data for any other variable.
Results
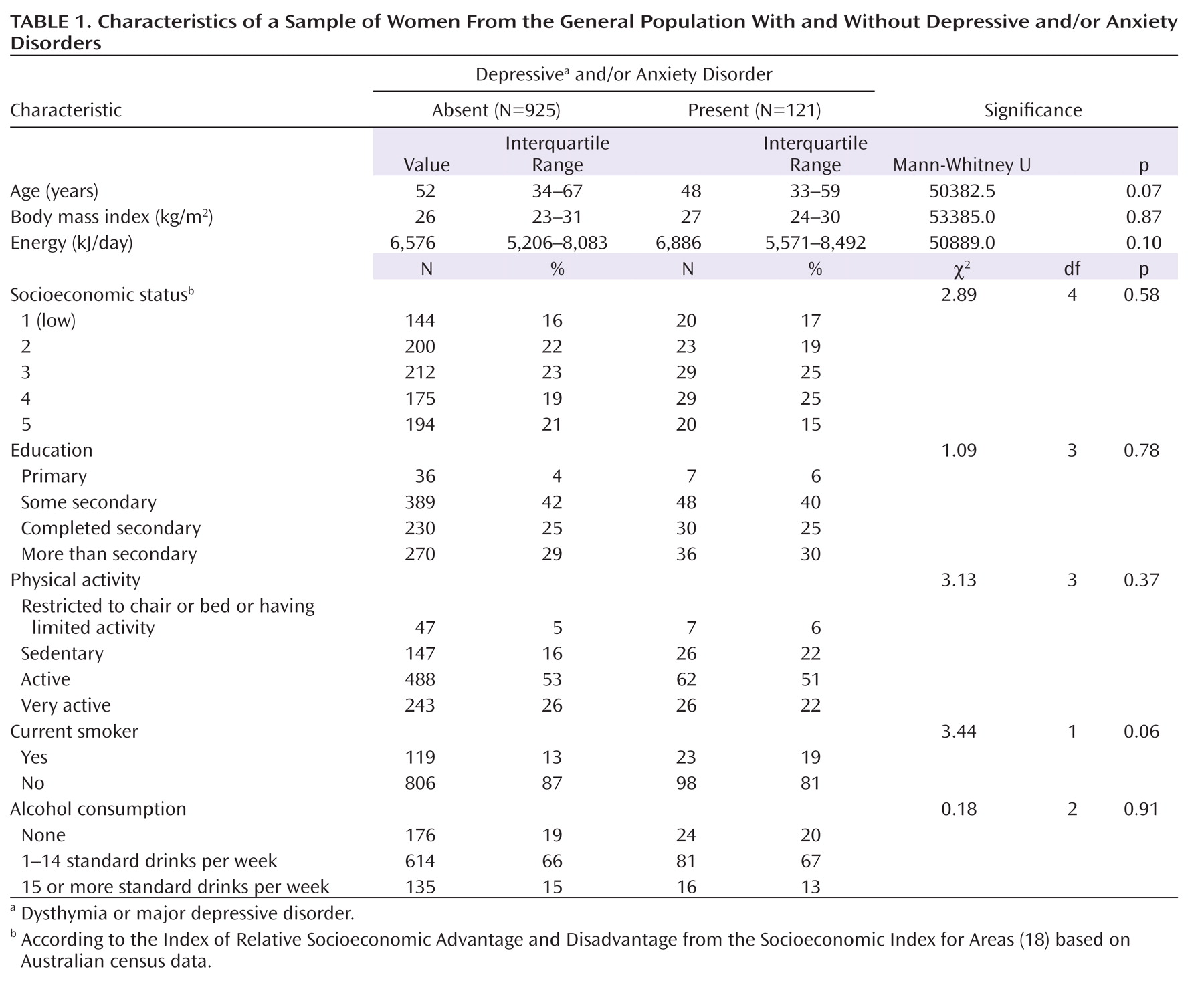
Table 1 presents characteristics of the study participants with and without depressive and anxiety disorders. Comparisons revealed no evident differences between those with and without these disorders on any of the included covariates.
Dietary Factor Scores
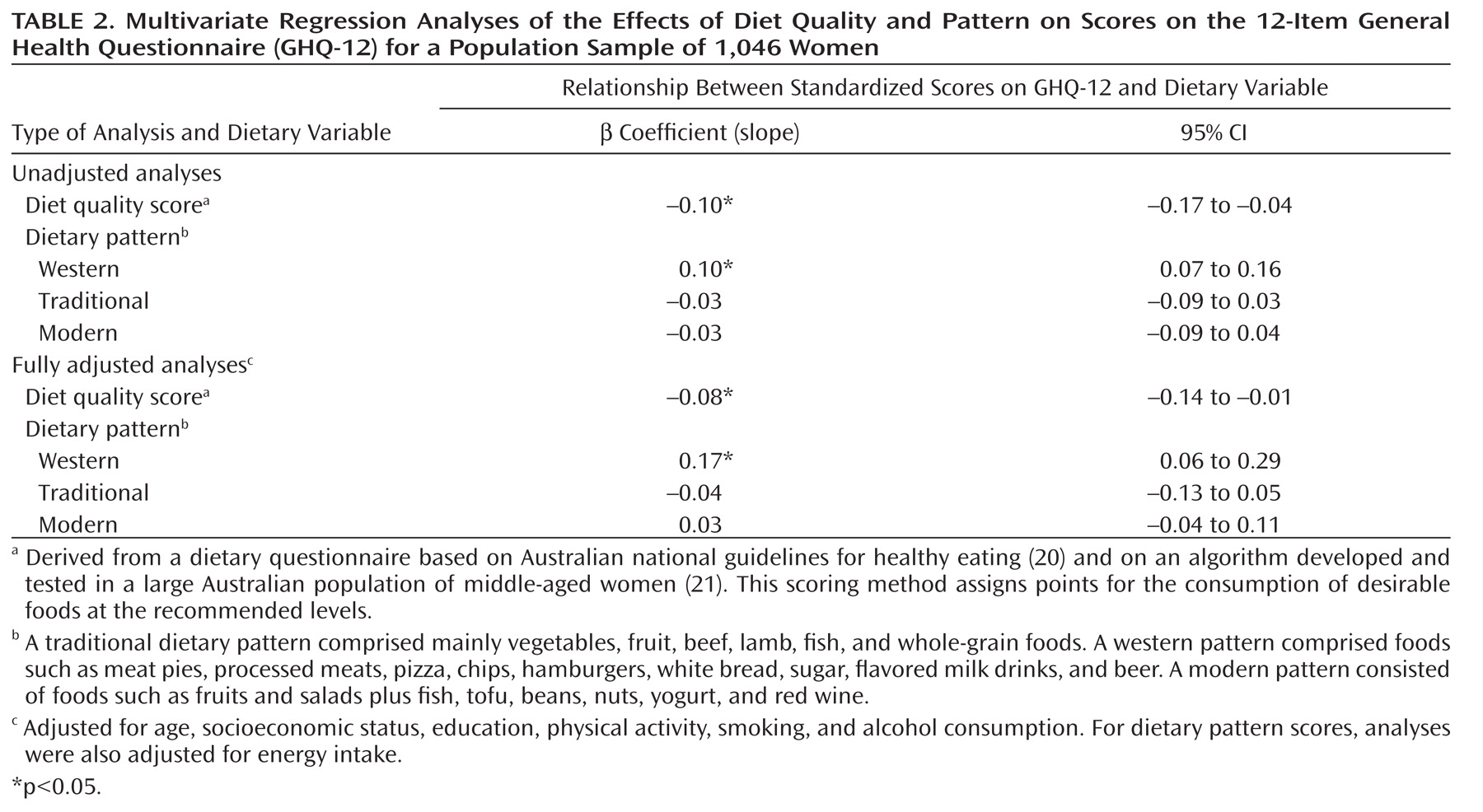
Results from analyses, with all three dietary patterns entered simultaneously as exposure variables, demonstrated that a western dietary pattern was associated with higher GHQ-12 scores, both before and after adjustments for potential confounders. After all adjustments, each standard deviation increase in the factor score for western diet was associated with a 0.17 SD increase in mean GHQ-12 score. There were no associations between the traditional or modern dietary pattern and the GHQ-12 score (
Table 2).
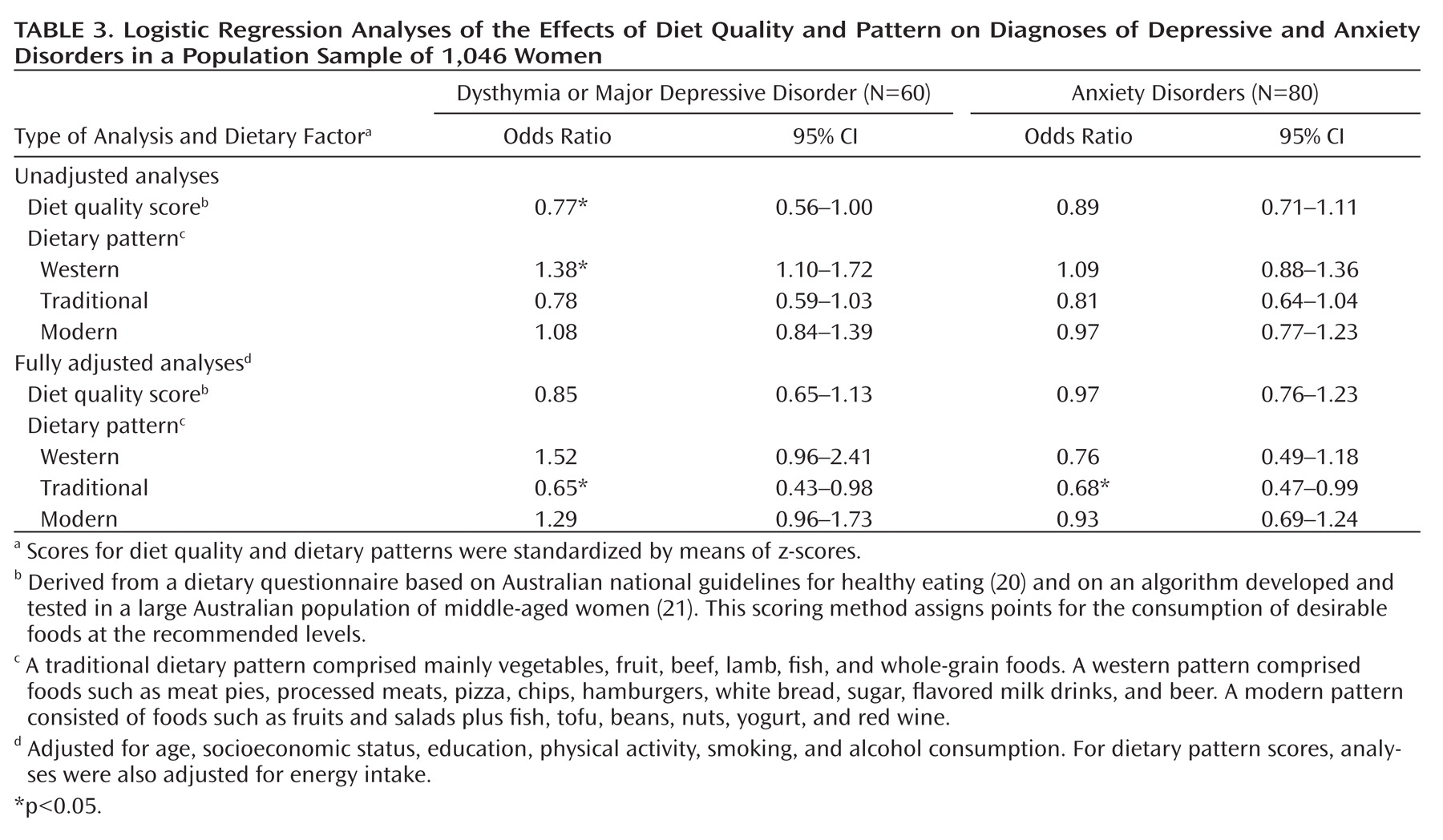
In analyses conducted with categorical depressive and anxiety disorders as outcomes, there were inverse relationships between the score for traditional diet and the odds for both depressive and anxiety disorders, which were strengthened by adjustments for socioeconomic and lifestyle factors. After adjustments for age, socioeconomic status, education, physical activity, alcohol consumption, smoking status, and energy intake, a 1.00-SD increase in the score for traditional dietary pattern was associated with a 35% reduced odds for major depression or dysthymia and a 32% reduced odds for anxiety disorders (
Table 3). The western dietary pattern was associated with increased odds for major depression or dysthymia in the unadjusted analyses. After adjustment for energy intake, the positive association between a western dietary pattern and depressive disorders was reduced but remained evident (Table 3). There was no observed association between a modern dietary pattern and depressive or anxiety disorders before adjustments, but there was a nonsignificant positive association between a modern dietary pattern and major depression or dysthymia after final adjustments for energy intake (Table 3). Further adjustment for body mass index did not affect the reported associations.
Diet Quality Scores
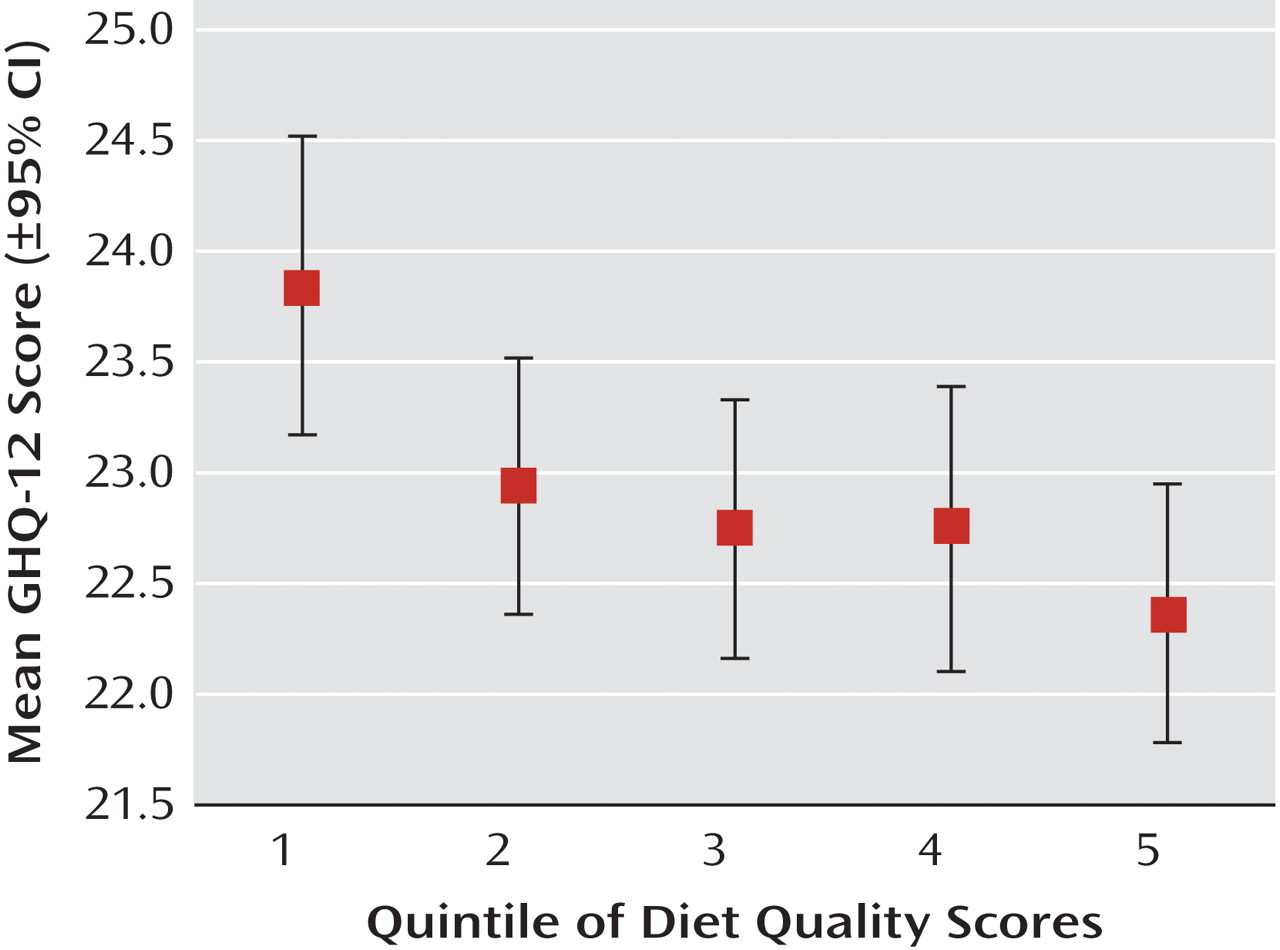
Diet quality scores were normally distributed and ranged from 4.0 to 56.0 (mean=30.8, SD=8.6). Multivariate regression analyses demonstrated that higher diet quality scores were associated with lower mean GHQ-12 scores. After all adjustments, there was a 0.08-SD decrease in log-transformed GHQ-12 score for every 1.00-SD increase in diet quality score (Table 2). The relationship between diet quality scores and GHQ-12 scores followed a dose-response pattern (
Figure 1). A higher diet quality score was also associated with lower odds for depressive disorders in the unadjusted model, but this association was attenuated by adjustments for socioeconomic and lifestyle factors. Once again, further adjustment for body mass index did not affect the reported associations.
Discussion
In this cross-sectional population-based study examining the association between diet and the high-prevalence mental disorders, the hypothesized association between habitual diet quality and these disorders was largely supported by the data. A dietary pattern comprising vegetables, fruit, beef, lamb, fish, and whole-grain foods (traditional) was associated with a lower likelihood of depressive and anxiety disorders, whereas a dietary pattern comprising processed and "unhealthy" foods (western) was associated with a higher likelihood of psychological symptoms and disorders. Better diet quality, as measured by the diet quality score, was associated with a lower level of psychological symptoms. Associations were apparent after adjustments for a wide range of possible confounding variables, including age, socioeconomic status, education, physical activity, and other lifestyle factors.
These results are concordant with previous research demonstrating associations between the quality of habitual diet and a range of other common noncommunicable diseases, risk factors, and medical outcomes. In the Nurses Health Study and the Health Professionals Follow-Up Study, those in the top quintile of diet quality scores had an approximately 25% lower risk for major chronic diseases, such as cardiovascular disease and cancer, over 8–12 years of follow-up compared to the lowest quintile (
22), and diet quality measured by dietary pattern analyses predicted cardiovascular disease risk in both studies (
23,
24). Diet quality was also inversely associated with overall and cancer mortality in a study of 42,000 older women over nearly 10 years of follow-up (
25). Recent results from the 52-country INTERHEART study demonstrated a 30% higher risk for acute myocardial infarction in individuals with higher scores on a measure of dietary "risk" (
26).
In this study, the observed attenuation of the positive relationship between the western dietary pattern and depressive disorders by adjustment for overall energy intake may indicate that the absolute amount of unhealthy food consumed in the diet is more relevant to mental health than the quantity as a proportion of overall diet. As it is also a healthy dietary pattern, the tendency for a modern dietary pattern to be associated with a higher, rather than lower, likelihood of depression was unexpected. This may be a consequence of reverse causality, wherein younger, more educated women, who had higher scores on the modern dietary factor, changed their diet in an attempt to improve their symptoms. Another explanation is that components of the traditional dietary pattern, such as vegetables, red meat, whole-grain foods, and high-fat dairy products, are particularly pertinent to the outcomes in question. Alternatively, this association may represent a type I error. We are conducting further studies to examine individual dietary components in relation to mental health outcomes.
Limitations and Methodological Issues
The main limitation of this study is the cross-sectional design, which prevents conclusions being reached regarding the direction of the relationship between diet and mental health. Appetite changes are a common feature of depressive illness, and a poor-quality diet may be a result of mental health symptoms, rather than a causative factor. Thus, without a prospective study design, it is not possible to preclude reverse causality as an explanation for our findings. However, in our study there was little evidence that the energy intakes of individuals with psychopathology were markedly different from those of the other subjects.
Diet is an indicator of overall lifestyle patterns, and health-related behaviors are influenced by mental illness, as well as influencing the risk for depressive illness (
27). Smoking, alcohol consumption, and physical activity levels are all indicators of self-care (
28) and were adjusted for in our analyses. Nevertheless, the possibility exists that we did not account for these adequately or that other unmeasured confounders were a factor in the results. Moreover, in studies examining diet as a risk factor for medical outcomes, confounding by socioeconomic status must be considered (
29). In this study, socioeconomic status and education had little impact on the reported associations, but it is not possible to rule out residual confounding or reporting bias by socioeconomic status as a factor in these results.
The strengths of this study include the use of gold-standard assessment tools for the diagnosis of depressive and anxiety disorders, the inclusion of a wide range of likely confounding variables, the testing of body habitus as a possible confounding or mediating factor, and comprehensive dietary assessments with a tool appropriate for the population under study. Diet quality was also operationalized by using both a priori measures (diet quality score) and naturalistic observations (factor analysis). Moreover, the study cohort was randomly selected, population based, and representative of the wider female Australian population (
30).
Mechanisms
Depressive illness is influenced by genetic, hormonal, immunological, biochemical, and neurodegenerative factors. Diet modulates each of these factors and, as a result, has a plausible impact on the development and course of this illness (
4).
Inflammatory processes are thought to play an etiological role in the onset and maintenance of depressive disorders (
31), as well as being of central importance in the high-prevalence noncommunicable diseases, such as cardiovascular disease, diabetes (
32,
33), and cancer (
34). Inflammation may, in part, explain the association between these medical illnesses, depression, and mortality, as well as the associations with diet. Adherence to a Mediterranean diet, high in vegetables, fruits, legumes, whole grains, fish, olive oil, and low-fat dairy products, correlates with lower levels of inflammatory markers (
35), whereas western-type diets and diets high in refined carbohydrates are associated with higher levels of C-reactive protein, a marker of low-grade inflammation (
5).
Nutritional factors also exert a direct and potent influence on neural physiology (
7). In experimental studies a western-style diet lowered brain-derived neurotrophic factor (BDNF) levels within a short time, an effect that was independent of obesity or nutritional deficits (
6). BDNF protects neurons from oxidative stress and promotes neurogenesis (
36) and is believed to play a central role in depressive illness (
37). Thus, by modulating the expression of BDNF, diet may influence psychiatric status.
Finally, diet influences oxidative processes, which may also be implicated in the pathophysiology of depressive illnesses (
38). For example, antioxidant-rich diets appear to be effective in slowing or preventing age-associated pathophysiological and cognitive changes (
39) and reducing the risk of age-associated diseases (
9). In this way, dietary factors may modulate the risk for neurostructural and cognitive changes in the brain that affect psychological symptoms across the life course (
38,
40).
The potential impact of diet on pathogenesis of depression may compound the impact of depressive illness on appetite and self-care. Thus, mental illness, dietary inadequacy, and nutrient depletion exacerbating mental illness may be linked in a vicious circle. This model remains to be tested but mirrors and overlaps with what is already known about the course of depressive illness (
41).
Conclusions
To our knowledge, this study is the first to present data suggesting that the significant impact of diet quality on common chronic noncommunicable diseases extends to the high-prevalence mental illnesses. We have reported associations between diet quality and mental health cross-sectionally; however, this relationship requires further examination in well-designed prospective studies in order to determine the direction of the relationships and to rule out residual or unrecognized confounding. Confirmation of a causal relationship between diet and mental health would afford the possibility for an evidence-based preventive health care strategy incorporating dietary improvement. Such an approach would overlap with existing strategies for other medical conditions and could be implemented at a population level. Given that diet, unlike many other risk factors, is theoretically a modifiable environmental exposure, the development of an evidence base seems worthy of pursuit.