Executive dysfunction is common in late-life depression (
1,
2) and predicts slow, poor, and unstable response to antidepressant agents (
3–6). This observation initiated research that identified structural (
7) and functional (
1,
8) brain abnormalities underlying executive dysfunction and interfering with antidepressant response. Pharmacological approaches to depression with executive dysfunction may be guided by emerging knowledge of the biological abnormalities of these patients.
In a parallel effort, we proposed a nonpharmacological intervention (
9). We envisioned this intervention as treatment that maximizes patients' skills in addressing problems originating from their depressive symptoms and executive dysfunction and reduces the chronic experience of stress. Depression with executive dysfunction has a rather distinct clinical presentation. Compared to cognitively intact depressed older patients, patients with major depression and executive dysfunction are more likely to have psychomotor retardation, apathy, lack of insight into their illness, and behavioral disability disproportionate to the severity of their depression (
2). Their disability is hardly surprising since the behavioral expression of executive dysfunction consists of difficulties in goal-setting, planning, initiating and sequencing behavior, and terminating behavior when goals are accomplished (
1). Disability resulting from the behavioral deficits of executive dysfunction exposes depressed older patients to chronic stress that may contribute to their poor outcomes.
Imparting problem-solving skills to depressed older patients with executive dysfunction is a rational treatment approach because it has the potential to mitigate their behavioral disability. Problem-solving therapy, a depression treatment, is based on the premise that helping patients become better managers of their lives reduces stress and thus ameliorates depression (
10). Problem-solving therapy trains patients to identify problems central to their well-being and provides a method for selecting and implementing problem-solving plans. It is effective in older adults with depressive syndromes (
11), medical problems (
12), and disabilities (
13) as well as in younger patients with mental disorders accompanied by executive dysfunction (
14).
We used problem-solving therapy as our intervention's theoretical basis and modified it to make it usable by depressed older adults with executive dysfunction. We selected the Nezu et al. (
15) social problem-solving structure because of its sequenced approach to teaching problem solving and its emphasis on problem orientation, a critical element of problem-solving therapy (
16). In our modification, we retained the therapy's original five steps in targeting problems and arriving at and implementing action plans. In the modified version, the therapist is more directive than in the original version, and patients may focus on less complex problems to facilitate learning. Similarly, the modified version provides more structure on selecting triggers for initiating action plans, sequencing actions, and terminating action once desirable goals are accomplished. In this study, we tested the hypothesis that modified problem-solving therapy leads to a greater reduction of depressive symptoms, a greater response rate, and a greater remission rate over a period of 12 weeks than supportive therapy in depressed older adults with executive dysfunction.
Method
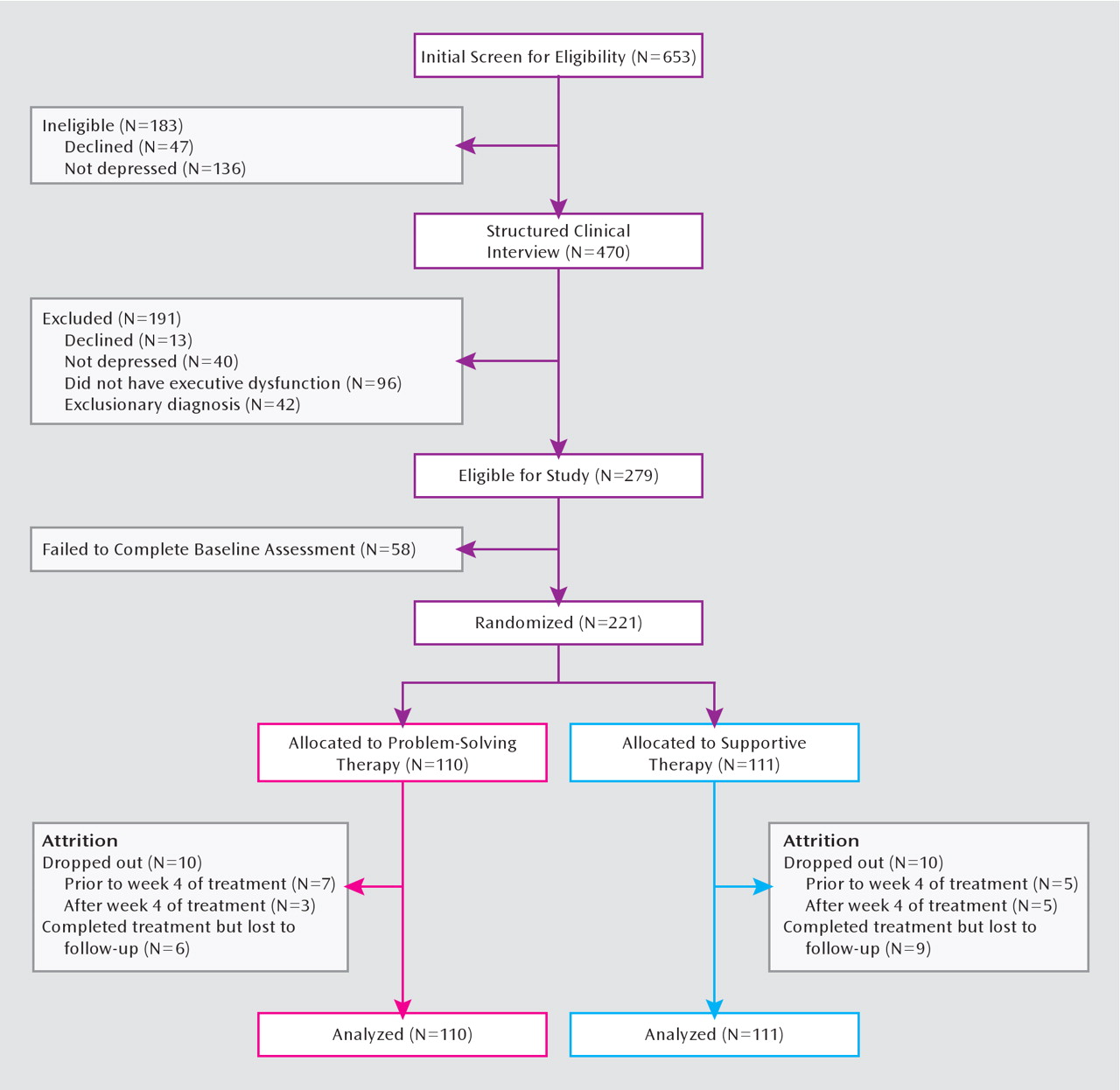
This was a two-site randomized controlled trial comparing a modified version of problem-solving therapy to supportive therapy in older patients with major depression and executive dysfunction. The study protocol was approved by the institutional review boards of both sites. Participants provided written informed consent after receiving a complete description of the study.
Systematic Assessment and Selection Criteria
Potential participants age 60 and older were interviewed with the Structured Clinical Interview for DSM-IV (SCID). Baseline interviews were conducted by interviewers credentialed by the Cornell Advanced Center for Services Research. Diagnoses were assigned by investigators after review of the clinical history, the SCID data, and all other available data during research case conferences. Severity of depression was quantified with the 24-item Hamilton Depression Rating Scale (HAM-D) (
17). Based on 56 interviews over the course of the study, interrater reliability for the HAM-D was found to be satisfactory, with an intraclass correlation coefficient of 0.80. Overall cognitive impairment was assessed with the Mini-Mental State Examination (MMSE) (
18). Executive functioning was assessed with the Wisconsin Card Sorting Test (
19), the Trail Making Test, Part B (
20), and the Frontal Systems Behavior Scale (
21). Measures related to psychopathology included age at onset of first episode of major depression, neuroticism (from the neuroticism subscale of the NEO Personality Inventory [22]), and history of antidepressant use (from the Composite Antidepressant Treatment Intensity Scale modified to include newer antidepressants [23]). Medical burden was assessed with the Charlson comorbidity index (
24), and disability with the 14-item World Health Organization Disability Assessment Schedule (
25). Baseline variables related to demographic characteristics, cognitive functions, psychopathology, medical burden, and disability were used in analyses of treatment moderators. All measures were selected for their documented validity and reliability in older adults.
To be eligible for the study, individuals had to meet DSM-IV criteria for major depression and have a score >20 on the HAMD, a score >24 on the MMSE, a score <33 on the initiation/perseveration subscale of the Mattis Dementia Rating Scale (
26), and a score <25 on the Stroop Color-Word Test (
27). These measures of executive function were selected for their utility in detecting executive dysfunction in late-life depression and the association of poor scores on these instruments with poor response to anti-depressant medication (
4).
Exclusion criteria included current treatment with psychotherapy or antidepressants; psychotic depression as indicated on the SCID; a high suicide risk (i.e., intent or plan to attempt suicide in the near future); any axis I disorder other than unipolar major depression and generalized anxiety disorder; antisocial personality disorder; a history of head trauma; dementia (an MMSE score <24 or a DSM-IV diagnosis of dementia); acute or severe medical illness (e.g., delirium, metastatic cancer, decompensated cardiac, liver, or kidney failure, major surgery, stroke, or myocardial infarction during the previous 3 months); use of drugs known to cause depression (e.g., reserpine, alpha-methyl-dopa, steroids); and inability to perform one or more activities of daily living even with assistance (e.g., walking with a cane was not an exclusion criterion). Less than 2% were taking benzodiazepines or sleep aids, and none were taking cognitive enhancers.
After baseline assessment, the HAM-D and the World Health Organization Disability Assessment Schedule were administered again at weeks 3, 6, 9, and 12. Transportation to assessment and treatment sessions was provided. Participants were compensated for time spent in assessments, but not treatment sessions.
Randomization
Participants were assigned to problem-solving therapy or supportive therapy within each site using random numbers in blocks of five participants. Raters were unaware of participants' randomization status and the study hypotheses. Therapists were aware of participants' randomization status but not the study hypotheses.
Problem-Solving Therapy
Treatment consists of 12 weekly sessions to teach participants a five-step problem-solving model (P.A. Arean et al, unpublished manuscript, 2003). This model is taught over the first 5 weeks of treatment, and subsequent sessions are dedicated to refining problem-solving skills. Participants set treatment goals; discuss and evaluate different ways to reach goals; create action plans; and evaluate their effectiveness in reaching goals. Participants are expected to implement plans and apply the problem-solving model to additional problems between sessions. In the last two sessions, participants create a relapse prevention plan using the problem-solving therapy model.
Supportive Therapy
Supportive therapy is a manualized therapy (M.S. Sachs, Cornell University, unpublished manuscript, 2000) similar to person-centered psychotherapy and consists of 12 weekly individual sessions. Therapists create a comfortable, nonjudgmental environment by demonstrating genuineness, empathy, and acceptance of patients without imposing any judgments on their decisions. This approach aids patients in addressing problems without direct input from therapists. Participants are encouraged to talk about their depression and any contributing life events. Therapists do not engage in any therapeutic strategy other than active listening and offering support focusing on participants' problems and concerns.
Therapist Intervention Adherence and Quality
Four doctoral-level clinical psychologists and four licensed social workers with at least 5 years of postlicensure experience served as therapists. None had prior experience with problem-solving therapy or supportive therapy, and each therapist was trained in both therapies. To control for potential bias resulting from therapists offering both treatments, all therapists participated in extensive training and were closely monitored to ensure that both treatments were provided with high quality. Training consisted of a 2-day workshop and supervision of six training cases (three per treatment). Fidelity monitoring consisted of review of randomly selected audiotapes (20%), rated by independent experts in both treatments using the Problem-Solving Therapy Adherence Scale (
28) for problem-solving therapy and the California Psychotherapy Assessment Scale (
29) for supportive therapy. Average therapist ratings for both treatments were excellent and ranged between excellent and exceptional. No differences in quality ratings were observed for any therapist for either treatment.
Data Analysis
Two separate analyses were performed on data from all participants who completed the baseline assessment (the intent-to-treat sample). First, profiles of pretreatment and weekly HAM-D scores over 12 weeks were compared for the two treatment groups using mixed-effect models for longitudinal data. These models included time-trend parameter(s), treatment assignment, site, site-by-treatment assignment interaction, time-by-treatment assignment interaction, and other baseline variables reflecting possible differences in patients' demographic and clinical characteristics across sites. Second, endpoint analyses were conducted with outcomes of “response” and “remission.” Response, defined as a reduction of ≥50% in HAM-D score, is commonly used in clinical trials as a measure of change since baseline. In contrast, remission has traditionally been used as a measure of a treatment's ability to produce a state approximating an asymptomatic state. In this study, we defined remission as a HAM-D score <10 for 2 consecutive weeks, a cutoff point commonly used in geriatric clinical trials (
30). Logistic regression was used to model factors associated with these endpoint outcomes. The omnibus statistic was used to test time-by-treatment interactions using intent-to-treat contrasts of response and remission at weeks 3, 6, 9, and 12. To assess moderation, baseline variables were checked for interactions with treatment effects. To determine the clinical utility of problem-solving therapy, number needed to treat was calculated for participants who completed assessments. Analyses were conducted using SAS, version 9.1 (SAS Institute, Cary, N.C.).
Discussion
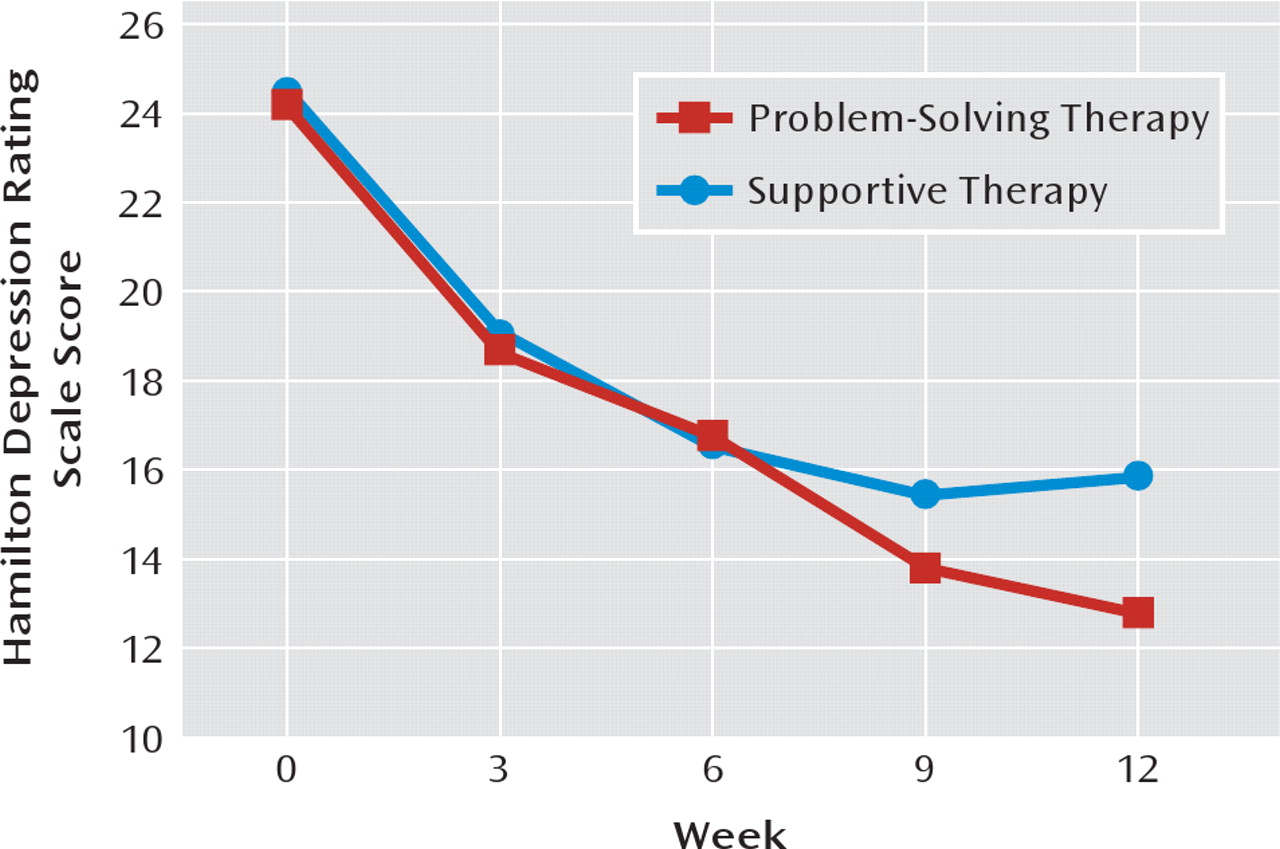
The principal finding of this study is that problem-solving therapy was more effective than supportive therapy in reducing depressive symptoms and produced greater response and remission rates in older patients with major depression and executive dysfunction. This population is usually more disabled than older depressed patients without executive dysfunction and has greater disability because of the cognitive deficits. By the end of the 12-week trial, more than half of the patients who received problem-solving therapy met criteria for treatment response, and more than 45% met criteria for remission. Problem-solving therapy led to one more remission than supportive therapy for every 5–6 patients receiving these treatments. This is a robust difference, considering that in clinical trials comparing active antidepressant treatments, response rates are closer to 35% and the number needed to treat one person to remission is 10 (
31). The efficacy demonstrated by problem-solving therapy is particularly important because depressed elderly patients with executive dysfunction have poor or slow response to pharmaco-therapy (
3–6).
This is the first study to demonstrate the efficacy of problem-solving therapy in older patients with major depression and executive dysfunction. Our findings are consistent with previous research demonstrating that problem-solving therapy is effective for depressed, cognitively unimpaired older patients (
11), older medical patients (
12), older adults with macular degeneration (
13), and older adults receiving home health care (
32). In addition to efficacy in geriatric depression, problem-solving therapy has been shown to reduce psychopathology and distress in nondepressed patients with disorders accompanied by executive dysfunction, such as schizophrenia (
14,
33). While problem-solving therapy was more efficacious than supportive therapy, supportive therapy led to substantial reductions in the severity of depressive symptoms and to acceptable response and remission rates by the end of the 12-week trial. In fact, supportive therapy was as efficacious as problem-solving therapy during the first 6 weeks of the trial. Supportive therapy has previously been shown to lead to clinically meaningful symptomatic improvement even when the comparator was found more efficacious (
34,
35). As a consequence, supportive therapy has been recommended as an active intervention for some depressive disorders, including postpartum depression (
36), and depression in day hospital patients (
37). Therapeutic factors common to supportive therapy and problem-solving therapy may explain their comparable performance early in treatment. In both treatments, therapists are empathic, provide a safe environment for patients to discuss their concerns, and offer hope. These nonspecific therapeutic strategies are also important in facilitating continued engagement in psychotherapy and have a beneficial effect on mood over time (
38), and they may explain why differences between the two treatments did not occur until later in the intervention.
The therapeutic advantage of problem-solving therapy over supportive therapy became apparent at weeks 9 and 12 of treatment. Most patients require approximately six sessions to learn the principles of problem solving. In subsequent sessions, patients consolidate use of the entire problem-solving therapy model by solving problems on their own in addition to those worked on with the therapist. The therapeutic effects of problem-solving therapy over supportive therapy occurred after the 6th week, at a time when participants were expected to have acquired adequate problem-solving skills. Therefore, a potential explanation for the late onset of therapeutic advantage of problem-solving therapy is development of new problem-solving skills through the problem-solving model. Our study's design does not allow us to determine whether problem-solving therapy owes its efficacy to improved problem-solving skills or to other components of the treatment, such as increased hopefulness, self-efficacy, problem resolution, and behavioral activation (
10). Developing measures of these variables suitable for cognitively compromised older populations and identifying mediators of the efficacy of problem-solving therapy would be useful next steps. Beyond its theoretical value, such a study would identify the most salient features of problem-solving therapy, allowing further refinement of its use in community settings.
This study's main findings should be viewed in the context of its limitations. First, our therapists provided both treatments, a design that might have permitted therapist bias to influence the efficacy of interventions. As in other psychotherapy studies using our design, we attempted to mitigate bias by selecting therapists who did not have previous experience with either intervention, training them to high standards, and continuously monitoring their delivery of both treatments. Assigning each therapist to only one treatment arm would have resulted in a nested design requiring a very large sample size in order to control for therapist-specific effects (
39). Furthermore, a nested design does not guarantee elimination of bias; therapists providing supportive therapy may have realized that they were the control condition had their participants not responded as well as anticipated.
Approximately 21% of older adults who met the study's selection criteria failed to enter the study because of limited interest or poor adherence to study procedures. However, 91% of those who started treatment remained in treatment until the end of the trial. Thus, our findings may be generalized mainly to patients who have sufficient interest and ability to be engaged in therapy. Furthermore, our sample was highly educated, thus limiting the general-izability of our findings to those with a college education. Although we assessed age at first depressive episode and whether the current episode was a recurrence, we have no information on the duration of the current episode, which may influence treatment outcome.
Study participants had mild executive dysfunction of unknown etiology. It remains unclear whether problem-solving therapy can be administered successfully to patients with more severe executive dysfunction or whether it is effective in patients for whom executive dysfunction evolves into dementia. We did not include a control arm of participants without executive dysfunction, and hence we are unable to determine whether patients with major depression and mild executive dysfunction do as well in problem-solving therapy and supportive therapy as those without executive dysfunction.
This study does not offer information on the stability of problem-solving therapy and supportive therapy effects after the end of the 12-week trial. Our encouraging results need to be followed by investigations of the stability of antidepressant response related to problem-solving therapy, need of maintenance problem-solving therapy, and appropriate maintenance dose of problem-solving therapy. Such studies are particularly warranted in elderly patients with depression and executive dysfunction, a population with a high propensity for relapse and recurrence (
3). Finally, none of the participants were taking antidepressants; only a direct comparison of problem-solving therapy and antidepressant treatment can determine which intervention is better.
Of particular importance in understanding the role of a treatment is determining whether any patient characteristics influence how well patients respond to this treatment. Only a sparse literature exists on predictors and moderators of psychotherapy outcomes in depressed older adults. Comorbid personality disorder, generalized anxiety disorder, and early onset of first depressive episode have been found to compromise response to other psychotherapies (
40,
41). Our results suggest interesting avenues for future exploration regarding problem-solving therapy's effects for other older adult populations. Problem-solving therapy appeared to have a slight advantage over supportive therapy for older adults with recurrent depression and older adults with functional impairments. In fact, participants with these clinical characteristics who received supportive therapy experienced a slight worsening of depressive symptoms over time. These data suggest that there may be opportunities for the development of treatment selection algorithms based on the clinical characteristics of patients seeking psychotherapy. As the effects were small, and given the complexity of moderation analyses, these results should be reviewed with caution. Future research regarding effects of patient characteristics on relative response to different psychotherapies could inform efforts toward individualized treatment.