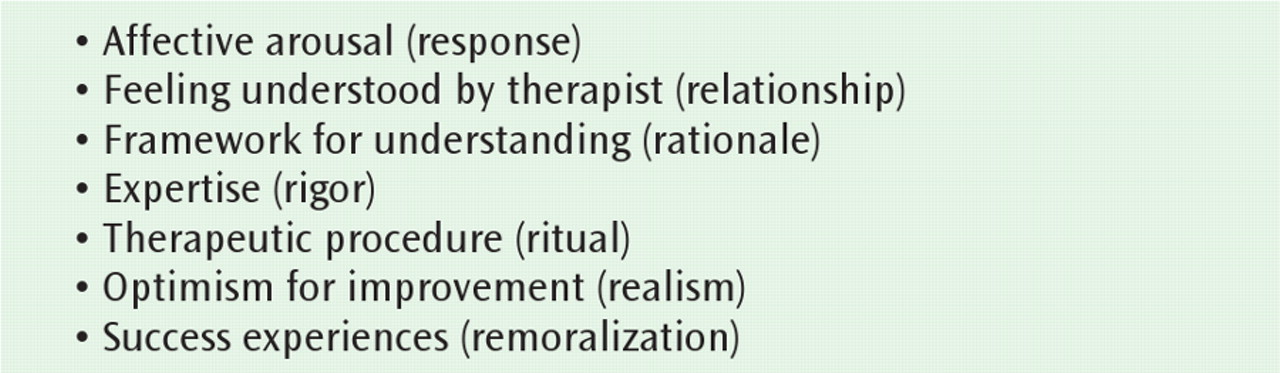
“Common factors,” so termed because all effective therapies reputedly share them, include common-sense aspects of engaging a patient in treatment (
Figure 1). These factors, which underlie the crucial formation of a clinician-patient therapeutic alliance, explain at least half the outcome variance in psychotherapy trials (
2) and equally mediate effective pharmacotherapy (
3). Most important among them—and, in our estimation, at greatest risk of attenuation in current training—is the therapist's ability to understand and respond emphatically to negative affective arousal. Affective arousal is central to engaging the patient, making psychotherapy meaningful. A psychotherapist's ability to respond to a patient's negative affect without flinching is a key aspect—sometimes the key aspect—of conducting successful psychotherapy, independent of modality. The therapist who tolerates such affect has the chance to understand it, help the patient understand it, and approach its resolution.
Every psychotherapist can find patients' negative affects stressful: a wave of depression, anger, or panic can feel overwhelming to therapists, as it does to patients themselves. Because many patients are affect-phobic and see their emotions as dangerous or “bad,” the capacity to respond to such affective blasts with empathy and poise is a crucial therapeutic skill. It allows patients to ventilate; to identify their inchoate feelings and articulate them in words; and then to achieve some distance from the affect and, in so doing, to recognize that feelings are potent but are not inherently dangerous. The therapist provides a support and a model: if you tolerate the feelings, they will diminish, lose toxicity; you can verbalize them, understand them, integrate them, gain control over them, even use them to understand and change your life situation (
4). Meeting strong negative affect with empathy and without retreat is an active intervention crucial to treating the grief of complicated bereavement (
5), the anxiety that habituation requires in exposure (
6), the anger of the patient with borderline personality (
7,
8) or bipolar disorder, and the acute anxiety in panic disorder. Sharing negative affect with a patient in effect demonstrates empathy. Conversely, to change the subject when emotion becomes uncomfortably intense tacitly conveys that the patient's feelings are in fact dangerous and best avoided.
Examples
Vignette 1
Therapist: Good to see you. How are you?
Mr. A: It's been a bad week. I've been feeling depressed. I haven't been feeling well. Nothing seems to be going right.
Therapist: [Brightly] Well, that's what we're here to work on. Let's talk about how you've handled it.
Mr. A: Well, it was hard. I've really been feeling horrible. I can't sleep, I'm really suffering…
Therapist: I'm sorry, I was thinking about what you said about your mother in the last session. Let's talk about that....
(Or, alternatively:
Therapist: Were you able to do the homework exercises?
Or:
Therapist: Do you need more medication?)
The session's tone has been set. This may seem a caricature of psychotherapy, but it mirrors a not uncommon therapist retreat from affect. The therapist is brisk, efficient, cheerful, and encouraging, cutting off the patient (an empathic failure) and imposing a structure that limits patient feedback while pressing the therapist's agenda. Therapists of all backgrounds can do this. At particular risk may be some cognitive-behavioral therapists who, taking the “learning theory” approach to psychotherapy too literally, aim simply to impart the lesson, to perform the psychic equivalent of physical therapy. This stance can result in a somewhat chipper, almost salesman-like, “fix-it” approach to psychotherapy “clients.” In contrast:
Vignette 2
Therapist: Good to see you. How have you been?
Mr. B: It's been a bad week. I've been feeling depressed. I haven't been feeling well. Nothing seems to be going right.
Therapist: [After a brief pause] I'm sorry to hear that. What's been happening?
Mr. B: Oh, you know. Things have been busy at work, I'm putting in my hours, but it's hard to concentrate, I don't feel like I'm doing a good job. [Stops]
Therapist: Why not?
Mr. B: I feel the tension with Fred over that project that's approaching deadline. It's a rat race, I'm on a treadmill, and I don't have the stamina for it. Fred keeps tripping me up and seems to take pleasure in it. Then when I get home, Millie's after me for being late, and the kids are too loud, and I'm in a lousy mood. And life seems pointless and hopeless.
Therapist: [After a pause, looking concerned] That really sounds awful.
Mr. B: Yes, it is…
Therapist: How did Fred trip you up this time?
Mr. B: He comes to my desk, leans over me, and says in this threatening voice, “Where's the report?” I say, “It's not due for another week. You know I'm waiting for the data from Charlie…” And he just rolls his eyes, like I'm a bozo.
Therapist: And what are you feeling then?
Mr. B: That he thinks I'm an idiot. That I'm never going to get anywhere if I have to work with him. And also, that he's the idiot: what does he think he's accomplishing—he knows I can't do anything until the figures arrive. I'd like to trip him and watch him fall on his face. But that's terrible.
Therapist: You mean you're angry at him.
Mr. B: Frustrated, annoyed…maybe a little anger.
Therapist: Is it terrible to acknowledge that you feel angry?
Mr. B: You know, it's mean of me to want someone to get hurt. I hate myself that I can have such ideas.
What is missing from the first vignette and evident in the second? The second therapist sounds far more interested in the patient's emotional experience between sessions, inquires about particulars, and reflects back the patient's emotional state. The therapist demonstrates an awareness and attempted understanding of the patient's feelings (sometimes termed “mentalization” [9]), thereby improving their mutual understanding and the therapeutic alliance. The session with Mr. B may now proceed in any number of directions: focusing on the patient's affect and normalizing anger as an appropriate response to bullying (a supportive psychotherapy model), on interpersonal relationships (how can Mr. B handle Fred? [interpersonal psychotherapy]), on cognitions (“He thinks I'm an idiot”; “I'm never going to get anywhere” [cognitive-behavioral therapy (CBT)]), on emotional underpinnings that begin to explain why anger feels so uncomfortable (psychodynamic psychotherapy), or on behavior.
Where the session leads depends on the treatment modality, but wherever it moves, the therapeutic alliance will be stronger than in vignette 1 because the patient will feel better understood and hence cared for by the therapist, a basic empathic intervention. Any good therapy should include this. The progression from abstract statement about general feelings to a description of specific incidents, identifying and articulating particular affects, and sitting with them at least briefly are hallmarks of good psychotherapy, across modalities. This sets the stage for whatever may follow, and the patient's affective engagement itself makes the session emotionally memorable.
The vignettes demonstrate therapists ignoring and beginning to explore patient affect, respectively. One might imagine some patients tolerate the first approach, whereas others feel ignored. Larger problems can arise when patients express stronger negative feelings:
Vignette 2—Continued
Mr. B: …So I come home, by now it's 9:30 p.m., and Millie's furious. She's mad at [the children], and at me for not being around. I'm already not in a good mood, and I just don't want to be there. So I take my dinner to the TV.
Therapist: Uh-huh.
Mr. B: After a minute or two she comes in and starts screaming at me about how I'm always late. I just want her to go away. I tell her I can't hear the show, can she please be quiet. I guess that just made her madder. She stands in front of me, blocking the TV, and starts yelling that I'm a bad husband, I never help, I'm always late… [Pauses and looks at therapist]
Therapist: [Maintaining eye contact, frowning with empathic, vicarious frustration] What are you feeling?
Mr. B: I hate her! I just want to kill her! She makes me so mad…and then I feel I'm just a bad person to feel that way, that she's right I'm a bad partner. So I don't say anything. I just sit there and steam.
Echoing the patient's story, the office now feels charged with tension. Many therapists might feel uncomfortable and change the subject. The therapist might share Millie's and Mr. B's characterization of himself as a “bad partner,” complicating an empathic response. Such strong emotion can easily discomfit therapists, evoking countertransferential responses that can lead them to quail, change the subject, and avoid this sudden rageful onslaught. Yet if the therapist can stay with the patient's affect, the session offers great opportunities to help Mr. B explore and understand his anger, to recognize why he is angry and (depending on treatment modality) how to begin to identify more adaptive responses to it.
Whenever a patient speaks, the therapist must decide when to interrupt rather than let the narrative continue and how to intervene at that juncture. Interventions can be abstract or specific, can elicit affect (“What are you feeling?”) or not. Therapists who are comfortable with strong emotions can use them to deepen therapy. They can emotionally mirror patients with nonverbal reactions—in eye contact; in facial expressions such as drawn eyebrows showing concern; by nodding vigorously; in posture, leaning forward or sitting up in their chair; and in responsive gesture and impassioned vocal tone, discussing the situation in a balanced, more rational way than the patient heretofore could. Such actions communicate that the therapist is attending, is trying to understand and connect with the patient's experience, and cares about the patient (the therapist is “mentalizing” the patient's mind). These therapeutic maneuvers may provide helpful modeling for patients who, feeling incompetent and riddled with confused, uncomfortable feelings or questioning the validity of their emotions, avoid their own affective responses. Clarification or simple silence can be effective, allowing the dyad to sit with emotions so that they build in the room. Therapists who employ a chipper, blandly bright stance lose these opportunities and likely strike patients as well-meaning but distant. Modeling a very limited emotional range may reinforce the patient's sense that negative inner affects are “bad” and should be avoided.
Thus, when a therapist pauses and encourages the patient to pause, to consider affect underlying the narrative, the story gains emotional resonance and cohesion for the patient. This opportunity is easily missed by therapists who do not actively seek to foster it. We consider this emotional focus a fundamental therapeutic factor, applicable across treatments.
More directive therapies risk moving to action too quickly and eliding encouragement of the patient's emotional tolerance and understanding of situations. In interpersonal psychotherapy (
4), where the therapist wants to organize the patient to act in an interpersonal context, the first step should always help the patient identify his or her emotional response to a situation: to feel it, name it, understand it as connected to the encounter (anger at harassment, sadness at parting, anxiety from a threat), and only then proceed to exploring and role-playing options for communicating a response (
4,
5). To jump to options for action before articulating and tolerating the affect makes the process less meaningful, thus lowering the potential for the patient to grow from the encounter. Yet many interpersonal psychotherapy trainees, from residents to experienced psychotherapists, make that hurried leap.
The same issue affects CBT (
10), which should focus on “hot”—emotionally charged—cognitions (
11). Affect is an identified mechanism of change in CBT (
12). The patient should feel the heat for a moment, recognize that his or her cognitions have emotional power, before the therapist employs Socratic questioning to help the patient challenge or validate that thinking. Lacking this first step, CBT can feel mechanical and intellectualized. Therapists who are uncomfortable with strong affect may focus immediately on irrational thoughts rather than on painful emotions and may develop the habit of checking automatic thoughts in order to deflect affect. Premature problem solving may serve to avoid facing the patient's emotions, compromising therapy and limiting its scope. This problem is not specific to CBT or to any manualized treatment: psychotherapists of all stripes, in all situations, may use their techniques to avoid affect. Psychotherapy manuals crucially operationalize treatments and guide therapists, but they are not magic: all treatments require therapeutic common factor skills, including response to affects, to be effective.
Countertransference Across Therapies
A potential therapeutic crisis arises when the patient directs negative affect—rage and disappointment—at the therapist. Every therapy responds differently to this potential crisis (see reference
13, for example), but regardless of the maneuver, the same principles hold. The therapist must recognize what is happening, abide the affect, understand it in context, and address it. In vignette 2, Mr. B may have felt angry not only at Fred and Millie, but also at his therapist, who might subsequently have addressed the affect in treatment.
Vignette 3
Mr. C, a 39-year-old law partner with severe anxiety, was most comfortable thinking about “practical things.” He found his emotional life, particularly any negative emotion, extremely unsettling. He avoided thinking about or discussing his feelings with anyone. Nonetheless, early in therapy, it grew increasingly clear to both Mr. C and the therapist that he was furious at his older brother and that his brother was actively doing things that directly and negatively affected Mr. C's life.
Mr. C: I'm just going to have to confront him about what he's been doing. I have to talk to him, I can't avoid it anymore. He does make me angry.... Now I'm getting all dizzy and lightheaded right now as I tell you about it. I can't handle it. [Standing up] I'm just going to have to leave the office and walk around. I have to go back to work soon. I can't sit here with all this going on. I can't be here. Gotta go.
Therapist: I see how uncomfortable you're feeling, but I'm not sure why you feel you have to leave right now…this does sound pretty important, no?
Mr. C: I just don't feel good…I don't really think therapy helps anyway, or I don't really believe in it. And I just have no way of dealing with how sick I feel all of a sudden. I think I should go now.
Therapist: Why not stay, so we can talk about how upset you are feeling?
Mr. C: You're bugging me!
Therapist: I hear you. This is really difficult. We've been talking about how avoiding intense feelings has been the way you've gotten used to dealing with uncomfortable feelings like being so angry at your brother. It feels more comfortable to do that here, too, I can tell. But maybe rather than stalking out of here and feeling out of control because you're so upset, we can try to understand why being this mad at your brother is so intolerable for you. [Mr. C stands, indecisive] What's happening for you right now that's making it so hard to stay and talk?
Mr. C: [Long pause] I think…[pacing]…I may start crying....
Therapist: That's okay.
Mr. C: [Cries a little] I hate crying.... I feel…small, pointless…like nothing at all.
Rather than changing the subject, Mr. C's therapist continued to follow his affect, which gradually dissipated as Mr. C articulated his feelings.
Implications and Responses
Although no data exist on trends in the handling of patient affects, the seemingly growing therapist tendency to avoid strong affects complicates supervision and training of even experienced psychotherapists. We have found that therapists must often start over, learn to “sit on their hands” and listen, allowing strong affects to build rather than quickly, “actively” intervening with patients. Therapists have generally experienced this more reflective stance as challenging, sometimes anxiety provoking, yet interesting. They sometimes report changing their overall treatment approach as a result (
17). One small survey found CBT-oriented therapists to have greater frustration than non-CBT therapists (effect size=0.4-0.6) in adjusting to conducting supportive, affect-focused psychotherapy (
17). Process-outcome research on therapist handling of affect deserves attention in psychotherapy trials.
Some individuals are inherently more empathic, interested in other people's stories, and open to new experience. We believe empathy can be nurtured but not instilled. Some therapists are naturally gifted. Early training is formative, so empathic listening, toleration of affect, and curiosity about patients deserve attention in residency and other basic psychotherapy training. Among experienced therapists, too, ability and openness to new experience vary, as do interest in and willingness to learn new therapeutic tools. The sophistication level of teaching varies with therapist experience, but the basic principles remain similar.
How can therapists stretch their emotional outlook? To become good therapists, trainees should learn the common factors. Responding to negative affect may be a particularly difficult task. Psychotherapy instructors and supervisors must focus on this issue. Reading Frank (
1,
16) and Rogers on the client-centered approach (
18) may provide helpful background. A personal psychotherapy may broaden therapist self-understanding of inner emotions and empathic understanding of the other side of the therapeutic experience. Videotaping psychotherapy sessions is an invaluable teaching tool (
19), freeing therapists from distracting process notes (which we discourage taking during sessions) and demonstrating session process and tone to supervisors. Group supervision helps educate trainees who lack current treatment cases.
Although some newly available tools, such as videotaping, can improve psychotherapy teaching in the context of modern practice, there is no doubt that more traditional opportunities, like seeing a patient's response to an empathic interpretation over a series of sessions, may be harder to obtain. We believe that psychotherapeutic education will need to develop more new methods to teach the common elements of psychotherapy, including the response to affective arousal, in the clinical setting where our trainees now practice.