The U.S. military began psychological screening in the early 20th century. During World War I, the Army Alpha and Beta tests and psychiatric interviews were used to screen the massive influx of military recruits needed to fight the war (
1). At that time, the personality and estimated intellectual functioning of each potential recruit were assessed, and recommendations were made regarding suitability for military service and service specialties. The decisions that were made largely reflected the belief that psychiatric symptoms and illnesses indicated a “weak personality”; individuals with psychoneurotic illness were not normal and thus were not capable of marshaling the defenses needed to serve during war (
1). Historians generally view this method of screening potential recruits for military service as a failure (
2).
In 1941, Harry Stack Sullivan was appointed as a psychiatric consultant to the Selective Service System and helped develop a more comprehensive screening system using screening interviews (
3). However, over the course of World War II, these screens came to be viewed as excessive and ineffective in accurately predicting resilience to the stresses of war, and it was thought that they resulted in a substantial and excessive loss of potential recruits (
4–
7). After World War II, psychiatric screening methods were modified to focus on identifying and disqualifying only those with gross psychiatric disorders. This general approach to recruitment or predeployment screening has remained in place since then.
Although screening continues, there is debate over the role that preexisting medical and psychiatric conditions have in making individuals more vulnerable to negative outcomes in times of stress. There are conflicting data as to whether preexisting psychological conditions are a contributing factor to psychiatric attrition in a combat zone and whether an effective screening mechanism exists (
8–
16). Common themes of previous studies of the subject include flawed methodology and outcomes based on the inconsistent screening application, use of personality or intelligence scales to identify vulnerability or predict future behavior, low thresholds for severity scales, and high false positive rates.
Since 1997, U.S. military units have conducted routine medical evaluations prior to deployment to ensure that soldiers do not have acute or chronic medical conditions that might impede performance during deployment. Those who are found to have a serious medical condition or who would be unable to receive the necessary level of medical care in theater are not cleared to deploy.
In 2006, media reports asserted that military psychiatrists and other medical providers were sending mentally unfit service members into combat zones (
17,
18). Later that year, the U.S. Department of Defense (DOD) developed a minimum mental health standard for deployment. This policy provided guidelines for what conditions are acceptable for military medical providers to manage in theater and what level of treatment can be provided during a deployment (
19). Individuals being treated for psychotic or bipolar disorders are barred from deployment, and the deployability of those with other psychiatric and behavioral conditions are assessed using an algorithm based on symptom severity, duration of treatment, stability of the condition, and level of care required.
Table 1 summarizes the key details of the policy and includes additional guidance from the Central Command responsible for the Iraq and Afghanistan combat theaters (
19,
20). Congress recently expanded the requirement for predeployment mental health screening to include “PTSD [posttraumatic stress disorder], suicidal tendencies, and other behavioral issues” in order to determine which service members need additional care or treatment (
21). However, there are virtually no scientific studies to help guide the military in how to do this most effectively.
While the DOD policy and new Congressional requirements mandate predeployment mental health screening on all deploying U.S. military personnel, these policies have not been based on evidence supporting the effectiveness of screening, and very little research has been conducted in this area.
We are aware of only one study (
22) that systematically assessed the effectiveness of predeployment screening in relation to recent operations in Iraq and Afghanistan. In this U.K. study, psychological symptom scales with thresholds designed to indicate distress were used to detect common mental disorders. The aim was to predict subsequent disorders 2 to 3 years after deployment. Like previous studies, it focused on trying to predict the development of mental disorders rather than seeking to identify or effectively manage the disorders during a deployment. The authors concluded that screening for mental disorders before deployment to Iraq would not have reduced subsequent morbidity, but they did not rule out the possibility that screening could be beneficial if the prevalence of deployment-related mental health conditions were higher (
22). The study did not look at U.S. military units working in areas with high-intensity combat engagement, which have been reported to have higher rates of PTSD and other mental health problems compared with U.K. forces (
23,
24).
In this article, we present data from a 2007 program evaluation of the effectiveness of a systematic method of predeployment mental health screening using the new DOD criteria to determine whether screening decreased negative outcomes for soldiers deployed in combat settings in Iraq. Although observational in nature, this study presents the only systematic assessment of predeployment screening of U.S. forces in Iraq and hence is of vital importance in understanding the potential impact of current predeployment screening policies in enhancing safety and ensuring continuity of care for deploying soldiers. This study and its methods depart from previous U.S. and U.K. studies, which focused on using mental health and personality scales to predict vulnerability and exclude individuals from deployment. Rather, we focus on predeployment psychiatric diagnoses, treatment needs, illness severity, and illness-related risks in order to improve mental health care for soldiers by linking them to ongoing treatment during deployment.
Method
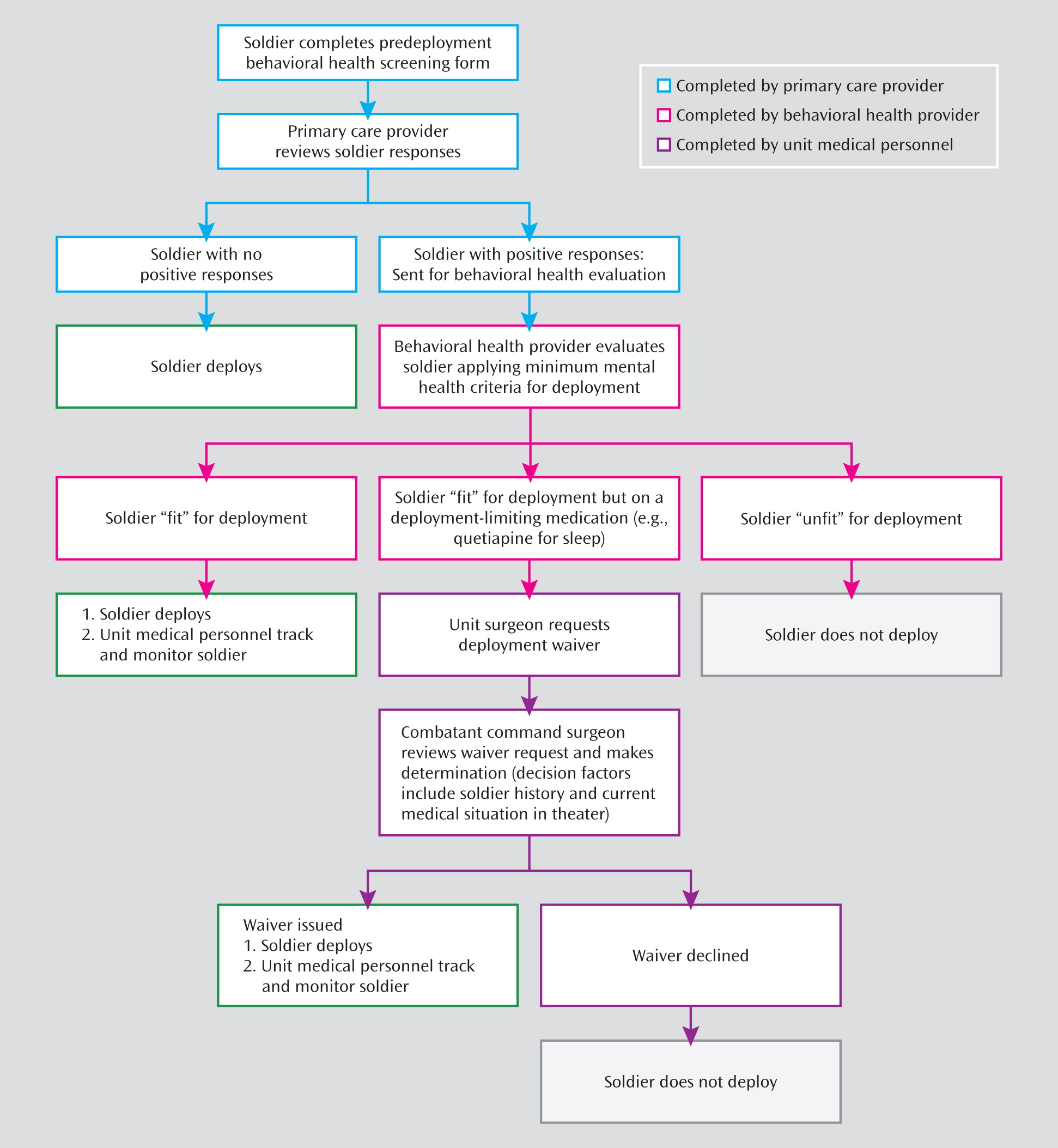
In this study, which was approved by the Eisenhower Army Medical Center institutional review board, we compared three infantry brigades from the Third Infantry Division deploying from Fort Stewart, Ga., to Iraq in early 2007 with three infantry brigades that were attached to the division from other posts. The mental health screening process was implemented in the three brigades from Fort Stewart according to the procedures outlined in
Figure 1. The process was not implemented in the three other brigades because of the complexity of merging the division together, the staggered deployment of brigades into Iraq over a period of 7 months, and the lack of sufficient time available between policy release and deployment for all brigades. Because the six brigades did not deploy at the same time but rather over a 7-month period, comparable outcomes could be tracked systematically only for the first 6 months of deployment for all six brigades, after which the Division Headquarters, including the clinical investigators, returned home from deployment.
All six brigades were deployed to the same region of central Iraq from 2007 to 2008 as part of that period's surge of forces. All were comparably sized active-duty brigade combat teams with more than one prior deployment to Iraq (although nearly half of the soldiers had no prior deployments), and all were assigned to the same division (Multi-National Division–Center) for operational control. Combat exposure, as assessed by enemy attack rates, was similar among the brigades, and tour lengths were all 15 months in duration. Available mental health resources were consistent among the brigades, and all evacuations were routed through and evaluated by the same senior mental health providers who deployed with the division.
Primary Care Evaluation
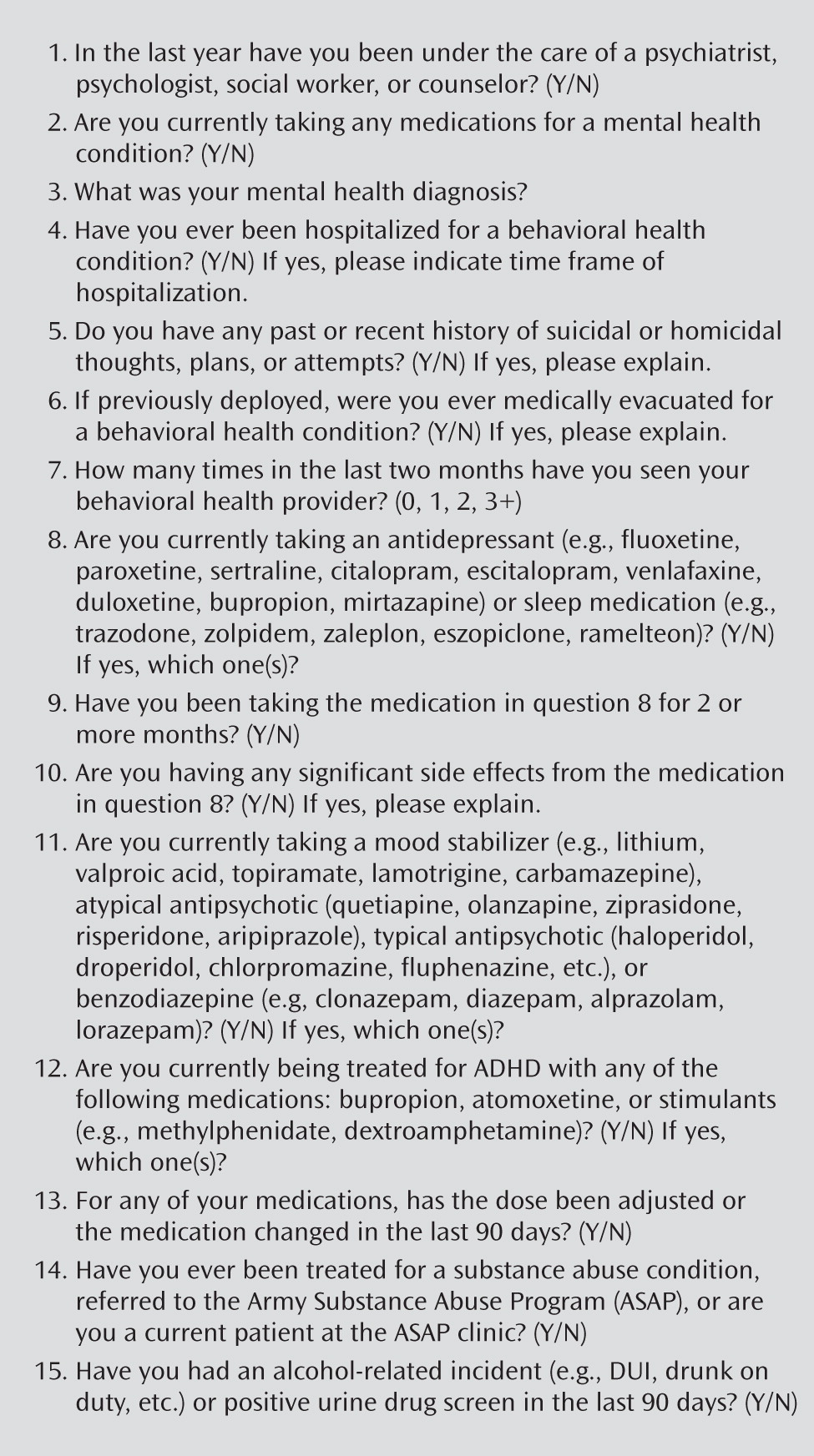
Each deploying soldier at Fort Stewart completed the predeployment behavioral health screening form as part of the standard face-to-face evaluation with a primary care provider during the soldier medical readiness evaluation (response rate, 100%). Key questions from this form are outlined in
Figure 2. The form was designed to identify any of the deployment-limiting criteria in the DOD criteria outlined in
Table 1. Soldiers with any of these issues were referred for an on-site mental health evaluation.
Mental Health Evaluation
The mental health evaluation was conducted immediately after the face-to-face evaluation with the primary care provider. A mental health provider (psychiatrist, clinical psychologist, or licensed clinical social worker) further evaluated the stability of medication treatment and all other deployment-limiting issues identified on the screening form; all cases involving psychiatric medications were reviewed with a psychiatrist. The outcomes of these evaluations were provided in writing to the medical officer in charge of each unit and documented in the soldier's electronic medical record.
On the basis of the evaluation, the mental health provider determined the soldier to be “fit” (able to deploy—for example, a soldier who was stable for at least 3 months on a psychiatric medication), “unfit” (not able to deploy because of a serious psychiatric condition or an unstable medication regimen), or “fit but on a deployment-limiting psychiatric medication” (if the soldier had been on a new psychiatric medication for less than 90 days). If determined to be fit for deployment with a stable psychiatric medication, the soldier was provided with a 3-month supply of medication, and coordination of in-theater mental health follow-up was to be monitored by the unit medical officer. If the soldier was found to be “fit but on a deployment-limiting medication,” then further consultation occurred involving the infantry unit medical and line leadership to assess for evidence of performance impairment. If there was agreement that the soldier was fit to deploy but had been taking a new medication for less than 90 days, then the unit was required to submit a formal waiver request to the Central Command Surgeon for a final determination (
25).
If the soldier was deemed unfit for deployment, one of two actions would occur. Either the soldier would be referred for a medical disability separation process following standards outlined in medical fitness for duty regulations (
26) or a meeting would be conducted with the soldier's commander to explain the recommendations about the soldier's condition and duty/deployment limitations. The mental health provider was instructed to clearly articulate to the commander why the soldier was not medically cleared for deployment, as permitted under Health Information Portability and Accountability Act exceptions involving military occupational duties (
27). The commander received information on the soldier's duty limitations and prognosis for being able to return to duty after treatment.
Outcomes
During the deployment from 2007 to 2008, outcomes were monitored through the Surveillance of Combat and Operational Stress Reactions (
28), a standardized mandatory reporting and tracking system used throughout the Iraqi theater of operations. This system required all mental health teams to maintain statistical information on their encounters, including nature of contact (combat operational stress reaction versus psychological/mental disorder), primary inciting event/factor, parasuicidal behaviors, limitations in duties placed on the soldier, and disposition. To ensure a standardized system throughout the deployment environment, all deploying mental health providers received training on this system as part of a mandatory combat operational stress course prior to deployment.
Within the surveillance system, combat and operational stress reaction contacts were defined as those related to deployment, and psychological/mental disorder contacts were defined as “disorders/issues that would occur in the absence of deployment.” Duty limitations, a measure of occupational dysfunction, included temporary actions such as short-term weapons restrictions; permanent duty restrictions, such as restricting soldiers to work only on the forward operating base; and medical evacuations for mental health conditions. For the purposes of this system, suicidal ideation was defined as expressing thoughts about taking one's life, while parasuicidal behaviors included any attempts or gestures toward taking one's life, including self-mutilation, pointing a weapon at oneself, and sublethal overdoses.
Each individual brigade mental health team tracked this information within their area of operations, and monthly summary reports were submitted to the division psychiatrist. The reports were cross-referenced for accuracy with other patient tracking systems that include mandatory reports for parasuicidal behaviors and air evacuations for behavioral health reasons. Prevalence rates with 95% confidence intervals (CIs) were computed, and chi-square tests were conducted to determine whether there were significant differences in behaviors between the two cohorts.
Results
In the six brigades, a total of 21,031 soldiers were deployed, of whom 10,678 received predeployment mental health screening.
Table 2 summarizes the demographic characteristics of the two cohorts. No significant differences were observed between the screened and unscreened cohorts, except a slightly greater number with one prior deployment in the unscreened group (χ
2=6.84, df=1, p<0.001).
Of the 10,678 soldiers in the three screened brigades, 819 (7.7%; 95% CI=7.2–8.2) required further mental health evaluation before deployment. Of these 819 soldiers, 472 (4.4%, 95% CI=4.0–4.8) were or had recently been under the care of a mental health provider and were not taking medications, and 347 (3.4%, 95% CI=2.9–3.6) were currently taking a psychotropic medication
Of the 347 taking psychotropic medications, 266 (76.7%, 95% CI=72.2–81.1) used antidepressants (mostly serotonin reuptake inhibitors), 108 (31.1%, 95% CI=26.3–35.6) used medications for chronic insomnia or sleep disturbances, 43 (12.4%, 95% CI=8.9–15.9) used stimulants for attention deficit problems, 23 (6.6%, 95% CI=4.0–9.3) used benzodiazepines for chronic anxiety symptoms, seven (2.0%, 95% CI=0.5–3.5) were on antipsychotics for psychotic disorders, 17 (4.9%, 95% CI=2.6–7.2) were on mood stabilizers for conditions other than bipolar disorder, and nine (2.6%, 95% CI=0.9–4.3) used mood stabilizers for bipolar disorder. A total of 114 (32.9%, 95% CI=27.9–37.8) had prescriptions for two or more psychotropic medications.
Of the 347 taking medication, 26 (7.5%, 95% CI=4.7–10.3) were delayed 1 to 2 months for medication stabilization before deploying, 32 (9.2%, 95% CI=6.2–12.3) were not cleared for deployment because they were unlikely to quickly stabilize, and 16 (4.6%, 95% CI=2.4–6.8) were not cleared for deployment because of their diagnosis (psychotic and bipolar disorders). Another 96 soldiers (27.7%, 95% CI=23.0–32.4) were deemed not fit to deploy because of their current medication, although they were stable and performing required duties without impairment, making them eligible for waiver consideration. This subgroup included soldiers who were taking stimulants for attention deficit problems, soldiers who had recently been started on a selective serotonin reuptake inhibitor but were otherwise stable, and soldiers who were taking low doses of atypical antipsychotics for insomnia. All of these soldiers were able to perform their assigned duties, and most were considered to be essential to the mission. The 96 waiver requests to Central Command specified length of time on the medication and outlined how the soldier would be monitored by mental health services during deployment. All 96 soldiers received waivers and were subsequently deployed. During the deployment, the division mental health team and the brigade surgeon ensured that each of the soldiers was seen at least monthly (based on clinical indications); all remained stable, functioned well in their duties, and successfully completed their deployment. Those soldiers who were receiving mental health treatment and were found fit for deployment had treatment plans for care in theater coordinated before deployment and were tracked by their mental health teams.
Table 3 outlines the rates of mental health sequelae during the first 6 months of deployment in the screened and unscreened cohorts. Soldiers in screened brigades had significantly lower rates than those in unscreened brigades for clinical contacts for suicidal ideation, combat stress, and psychiatric disorders, as well as lower rates of occupational impairment and air evacuation for behavioral health reasons.
Discussion
This is the first modern systematic program evaluation of the effectiveness of predeployment screening of U.S. military personnel. This is a timely and important study, considering the Congressional mandate to conduct such screenings uniformly in all deploying personnel. Unlike previous predeployment assessments, which focused on predicting vulnerability, this screening method focuses on identifying active psychiatric and behavioral health issues that may require a high level of care, impair a soldier's ability to perform his or her duties, or require ongoing close monitoring by mental health professionals working in the operational environment. Significant inverse associations were observed between predeployment screening and rates of mental health evacuations, suicidal ideation, combat operational stress reactions, and occupational impairment. These results show that an aggressive program of mental health screening, tracking, and coordination of care may enhance a unit's functioning while decreasing negative soldier outcomes.
The likely reasons for the apparent success of this program are several. The program involved several key components, including 1) primary care evaluation of all soldiers; 2) standardized criteria for identifying high-risk individuals based on current and past psychiatric diagnoses, illness severity, and treatment needs; 3) immediate on-site mental health evaluation of at-risk soldiers; 4) removal of the highest-risk soldiers from deployment; 5) comprehensive tracking of all at-risk soldiers and coordination of care into the deployment environment to ensure appropriate follow-up and mental health care; and 6) selection of relevant measures of effectiveness. Identified soldiers had a care management plan in place that was coordinated from the predeployment period into the deployment environment and were thus able to have close care management before, during, and after deployment. Moreover, the unit providers could coordinate with in-theater resources while developing individualized treatment plans. The design of this screening model also assisted commanders by providing rapid and clear recommendations from medical providers by means of a standardized decision-making process.
The most important scientific limitation of this program evaluation is that it did not involve a randomized design, and therefore the outcomes and conclusions are observational and dependent on the units being otherwise comparable. A randomized design was not possible here because the screening requirement had already been mandated by the DOD, and conducting such a randomized trial in military units deploying to a combat zone was not feasible. The phased implementation of the screening throughout the U.S. Army, coupled with the deployment timeline in close proximity to the implementation of the new DOD guidelines, allowed for a narrow window of evaluation of comparable populations. To address the limitation of a lack of randomized design, all data were gathered from units that deployed within the same area of Iraq during the same period (the 2007 troop surge), which ensured similar mission and combat exposure. All units were active-duty brigade combat teams, which have similar numbers of soldiers and comparable structure, mission, and demographic characteristics. No National Guard or Army Reserve units were included in this evaluation. All units had the same data monitoring and reporting requirements and had similar numbers and availability of mental health personnel. Evacuations from all six brigades went through the same senior mental health providers and clearance procedures.
Although this program required disclosure of medication use by soldiers, those who wanted to deploy may not have been honest in reporting their medications. While medications prescribed in the military system or through the DOD civilian network would be identified in medical records accessible during the primary care provider's screening, it is possible that soldiers paid for care or medications from outside resources that would not be apparent in medical records unless disclosed. However, if this led to a study bias, it should have been in the direction of failing to show any difference between cohorts.
Lastly, this study was not designed to identify rates of existing mental disorders prior to deployment or to predict development of new mental disorders after deployment. It was designed to evaluate the effectiveness of the DOD screening process in reducing negative outcomes during deployment. Furthermore, given the study's short time frame (6 months), our data do not allow us to assess whether the screening had longer-term benefits.
Conclusions
The predeployment time frame can be stressful for both soldiers and commanders. By creating a systematic process involving primary care staff, mental health care staff, and unit leaders, soldiers were provided with the care they needed and commanders had a way to provide input on important occupational considerations. This predeployment screening process was associated with a decreased need for clinical care for combat stress, psychiatric and behavioral disorders, and suicidal ideation. Although not a randomized study, this systematic program evaluation provides the first direct evidence to support the use of a service-wide program of predeployment mental health screening following this model.