Interpersonal Psychotherapy for Depression: A Meta-Analysis
Abstract
Objective:
Method:
Results:
Conclusions:
Method
Search Strategy
Inclusion and Exclusion Criteria
Quality Assessment
Analyses
Power Calculation
Results
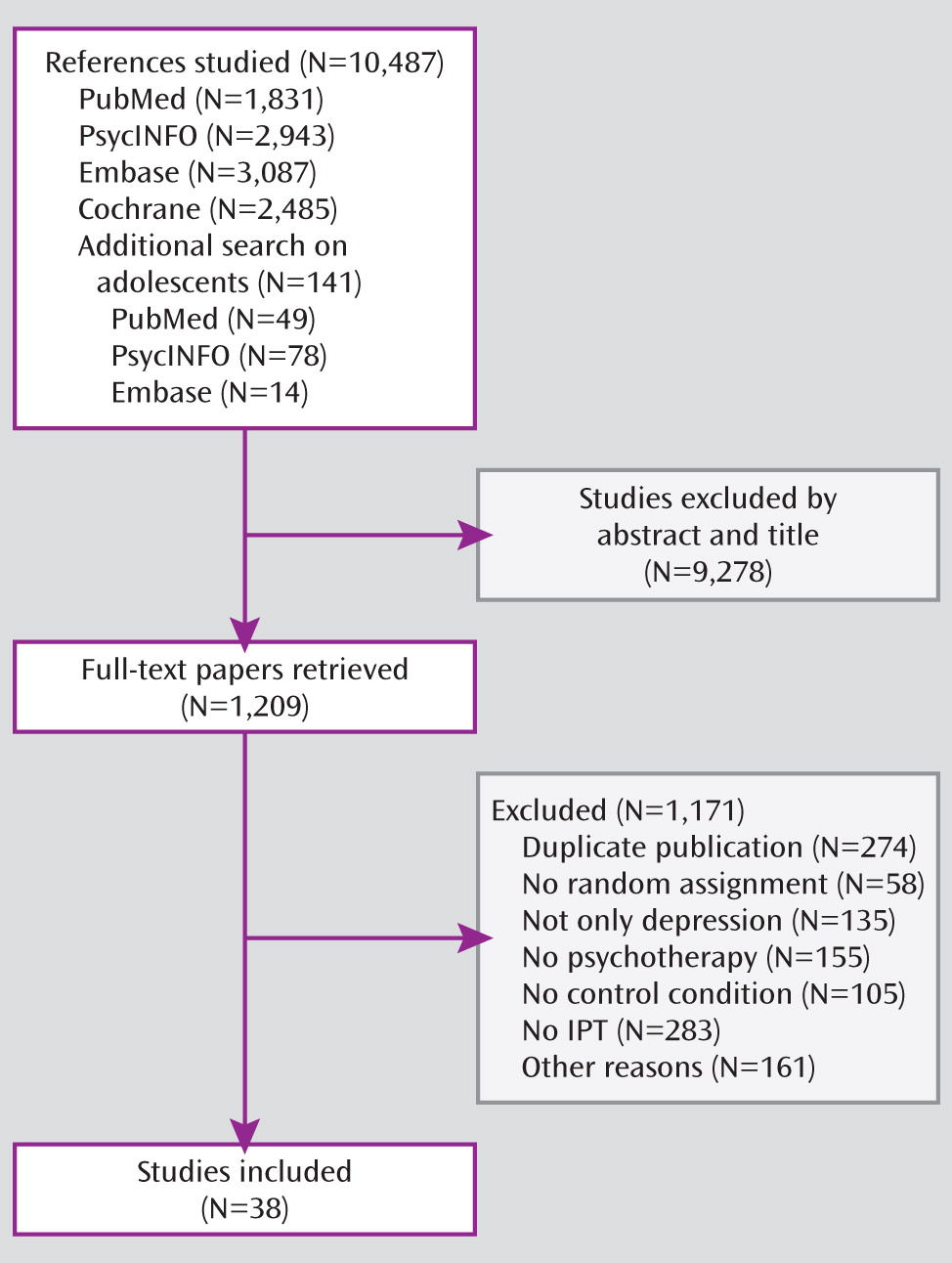
Selection and Inclusion of Studies
Characteristics of Included Studies
| Study Authors (Reference Number) | IPT Typea | Diagnosis (Basis of Diagnosis)b | Target Group | Study Interventionsc (N) | Formatd | Sessions (N) | ITTe | Outcome Measuresb | Countryf |
|---|---|---|---|---|---|---|---|---|---|
| Bellino et al. (36) | O | Major depression (clinical judgment) | Adults with borderline personality disorder | IPT+PHA (N=20); PHA (N=19) | IND | 24 | N | HAM-D | IT |
| Blom et al. (37) | O | Major depression (SCID) and HAM-D ≥14 | Adult outpatients | IPT (N=50); IPT+PHA (N=49); PHA (N=47); IPT+PLA (N=47) | IND | 12 | Y | HAM-D, MADRS | NL |
| Bodenmann et al. (38) | O | Major depression or dysthymia (SCID) | Adults over age 60 (and their partners) | IPT (N=20); COCT (N=20); CBT (N=20) | IND | 20 | Y | HAM-D, BDI | SW |
| Bolton et al. (39) | A | Major depression or subsyndromal depression (clinical interview) | Adults | IPT (N=107); UC (N=117) | GRP | 16 | Y | Specially developed measures for local use | UG |
| Bolton et al. (40) | A | Major depression or subsyndromal depression (clinical interview) | Adolescent survivors of war and displacement | IPT (N=105); WL (N=104); creative play (N=105) | GRP | 16 | Y | Specially developed measures for local use | UG |
| Browne et al. (41) | O | Dysthymia (SCID) with or without major depression | Adults | IPT (N=178); IPT+PHA (N=212); PHA (N=196) | IND | 10 | N | MADRS | CA |
| De Mello et al. (42) | A | Dysthymia (clinical interview), major depression permitted | Adults | IPT+PHA (N=16); PHA (N=19) | IND | 16 | N | HAM-D, MADRS | BR |
| Elkin et al. (43) | O | Major depression (RDC) and HAM-D ≥14 | Adults | IPT (N=61); CBT (N=59); PHA (N=57); PLA (N=62) | IND | 16 | Y | HAM-D, BDI | US |
| Finkenzeller et al. (44) | A | HAM-D ≥14 | Stroke patients | IPT (N=27); IPT+PHA (N=23); PHA (N=24) | GRP | 8 | Y | HAM-D, HADS | GE |
| Frank et al. (45) | M | Recovered from major depression (RDC) after acute treatment (PHA+weekly IPT)c | Adults | M-IPT+M-PHA (N=25); M-PHA (N=28); M-IPT (N=26); M-IPT+PLA (N=26); PLA (N=23) | IND | Monthly | Y | Recurrence rate after 3 years | US |
| Lespérance et al. (46) | O | Major depression (SCID) and HAM-D-24 ≥20 | Patients with coronary artery disease | IPT+PHA (N=67); PHA (N=75); IPT+PLA (N=75); PLA (N=67) | IND | 12 | Y | HAM-D | CA |
| Klerman et al. (47) | M | Clinical improvement after acute treatment (PHAc) for neurotic depression (DSM-II) | Adults | M-IPT+M-PHA (N=25); M-IPT+PLA (N=25); M-IPT (N=25); M-PHA (N=25); PLA (N=25); clinical management only (N=25) | IND | Weekly | Y | Recurrence rate after 8 months | US |
| Levkovitz et al. (48) | M | Recovered from major depression (DSM-IV) after acute treatment (PHAc) | Adults | M-IPT+M-PHA (N=7); M-PHA (N=7) | GRP | 18 | Y | HAM-D score at 6-month follow-up | IS |
| Luty et al. (49) | O | Major depression (SCID; DSM-III-R) | Adults | IPT (N=91); CBT (N=86) | IND | 16 | Y | MADRS | NZ |
| Markowitz et al. (50) | A | HAM-D-24 ≥15 and clinical judgment of depressive symptoms | HIV patients | IPT (N=24); SUP (N=24); CBT (N=27); SUP+PHA (N=26) | IND | 11 | Y | BDI, HAM-D | US |
| Markowitz et al. (51) | A | Dysthymia (SCID) and HAM-D-24 >13 | Adults | IPT (N=23); IPT+PHA (N=21); SUP (N=26); PHA (N=24) | IND | 16 | Y | BDI, CDRS, HAM-D | US |
| Markowitz et al. (52) | A | Dysthymia (SCID) and HAM-D-24 >13 | Adults with secondary alcohol use disorder | IPT (N=14); SUP (N=12) | IND | 16 | Y | BDI, CDRS, HAM-D | US |
| Marshall et al. (53) | O | Major depression (SCID) and HAM-D ≥10 | Adults | IPT (N=35); CBT (N=37); PHA (N=30) | IND | 16 | N | HAM-D | CA |
| Martin et al. (54) | O | Major depression (clinical judgment) and HAM-D ≥18 | Adults | IPT (N=13); PHA (N=15) | IND | 16 | Y | BDI, HAM-D | UK |
| Mufson et al. (55) | A | HAM-D-24 ≥15 | Adolescents | IPT (N=24); monitoring (N=24) | IND | 12 | Y | BDI, HAM-D | US |
| Mufson et al. (56) | A | Mood disorder (K-SADS) | Adolescents | IPT (N=34); UC (N=29) | IND | 12 | Y | BDI, HAM-D | US |
| Mulcahy et al. (57) | A | Major depression (DSM-IV, MCMI-III) | Women with postpartum depression | IPT (N=29); UC (N=28) | GRP | 10 | N | EPDS, BDI, HAM-D | AU |
| Neimeyer and Feixas (58) | O | Major depression (RDC) and BDI >15 | Adults | IPT (N=39); CBT+homework (N=32); CBT, no homework (N=31) | GRP | 10 | N | HAM-D | US |
| O'Hara et al. (59) | A | Major depression (SCID) and HAM-D ≥12 | Women with postpartum depression | IPT (N=60); WL (N=60) | IND | 12 | Y | BDI, HAM-D | US |
| Ransom et al. (60) | A | Major depression or dysthymia (PRIME-MD) | Rural HIV patients | IPT (N=41); UC (N=38) | TEL | 10 | Y | BDI | US |
| Reynolds et al. (61) | A | Major depression (SADS, SCID) | Bereaved adults (age 50 or older) | IPT+PHA (N=16); PHA (N=25) | IND | 16 | Y | HAM-D | US |
| Reynolds et al. (62) | M | Recovered from major depression after 16-week acute treatment (PHA + weekly IPT)c | Older adults | M-PHA+M-IPT (N=25); M-PHA (N=28); M-IPT+PLA (N=25); PLA (N=29) | IND | Monthly | Y | Recurrence rate after 3 years | US |
| Reynolds et al. (63) | M | Recovered from major depression after 22-week acute treatment (PHA + weekly IPT)c | Older adults | M-PHA+M-IPT (N=28); M-PHA (N=35); M-IPT+PLA (N=35); PLA (N=18) | IND | Monthly | Y | Recurrence rate after 2 years | US |
| Rosselló and Bernal (64) | A | Major depression and/or dysthymia (DISC) | Adolescents | IPT (N=23); CBT (N=25); WL (N=23) | IND | 12 | Y | CDI | PR |
| Rosselló et al. (65) | A | Major depression (DISC) or CDI ≥13 | Adolescents | IPT (N=60); CBT (N=52) | IND+ GRP | 12 | Y | CDI | PR |
| Schramm et al. (66) | A | Major depression (SCID) and HAM-D ≥16 | Adult inpatients | IPT+PHA (N=63); PHA (N=61) | IND+ GRP | 23 | Y | BDI, HAM-D | GE |
| Schulberg et al. (67) | O | Major depression (DIS) and HAM-D ≥13 | Adults | IPT (N=93); PHA (N=91); UC (N=92) | IND | 16 | Y | HAM-D | US |
| Sloane et al. (68) | O | Major depression (RDC) and HAM-D ≥17 | Older adults | IPT (N=19); PHA (N=10); PLA (N=14) | IND | 6 | N | BDI, HAM-D | US |
| Spinelli and Endicott (69) | A | Major depression (SCID) and HAM-D-24 ≥12 | Pregnant women | IPT (N=21); parenting education (N=17) | IND | 10 | Y | BDI, EPDS, HAM-D | US |
| Swartz et al. (70) | A | Major depression (SCID) and HAM-D ≥15 | Mothers whose children receive psychiatric treatment | IPT (N=26); UC (N=21) | IND | 9 | N | BDI, HAM-D | US |
| Tang et al. (71) | A | BDI >19 | Adolescents | IPT (N=35); UC (N=38) | IND | 12 | Y | BDI | TW |
| Van Schaik et al. (72) | O | Major depression (PRIME-MD) | Older adults (age 55 or older) | IPT (N=69); UC (N=74) | IND | 8 | Y | GDS, MADRS, PRIME-MD | NL |
| Weissman et al. (73) | O | Major depression (SADS) and RTADS ≥7 | Adults | IPT (N=17); IPT+PHA (N=23); on-demand telephone support (N=21); PHA (N=20) | IND | 16 | N | RTADS | US |
Quality Assessment
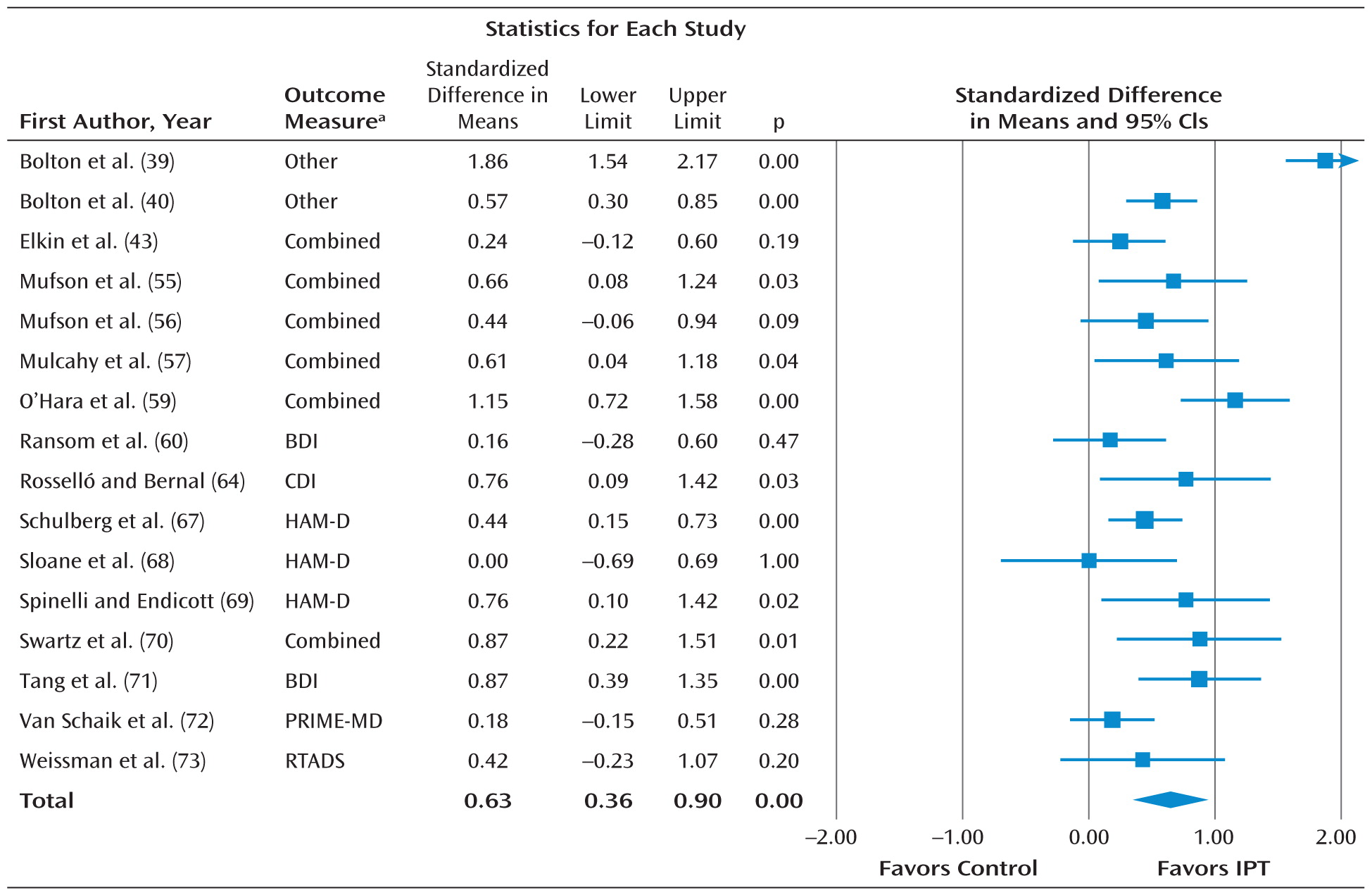
IPT Compared With Standard or No Treatment
| Comparison | Number of Comparisons | d | 95% CI | Heterogeneityb | pc | Number Needed to Treat |
|---|---|---|---|---|---|---|
| IPT versus control condition | ||||||
| All studies | 16 | 0.63*** | 0.36 to 0.90 | 82.96*** | 2.91 | |
| Outlier removedd | 15 | 0.52*** | 0.36 to 0.68 | 42.84* | 3.50 | |
| HAM-D only | 9 | 0.60*** | 0.39 to 0.81 | 40.47 | 3.05 | |
| BDI only | 7 | 0.60*** | 0.32 to 0.89 | 59.62* | 3.05 | |
| Subgroup analysese | ||||||
| Adapted manual | ||||||
| No | 5 | 0.29 | 0.12 to 0.47 | 0.00 | 0.004 | 6.17 |
| Yes | 10 | 0.67 | 0.48 to 0.85 | 27.52 | 2.75 | |
| Target group | ||||||
| Adults in general | 3 | 0.37** | 0.15 to 0.58 | 0.00 | 0.214 | 4.85 |
| Adolescents | 5 | 0.63*** | 0.43 to 0.82 | 0.00 | 2.91 | |
| Specific target group | 7 | 0.53** | 0.19 to 0.87 | 68.11** | 3.42 | |
| Basis of diagnosis | ||||||
| Diagnostic interview | 12 | 0.57*** | 0.40 to 0.73 | 29.74 | 0.424 | 3.18 |
| Self-report | 3 | 0.38 | –0.04 to 0.80 | 67.73* | 4.72 | |
| Control group | ||||||
| Usual care | 6 | 0.50*** | 0.28 to 0.72 | 32.20 | 0.182 | 3.62 |
| Waiting list | 3 | 0.81*** | 0.42 to 1.20 | 59.63 | 2.30 | |
| Other | 5 | 0.38** | 0.14 to 0.62 | 0.00 | 4.72 | |
| Intent-to-treat analysis | ||||||
| Yes | 10 | 0.57*** | 0.38 to 0.76 | 51.56* | 0.718 | 3.18 |
| No | 4 | 0.50** | 0.16 to 0.84 | 12.97 | 3.62 | |
| IPT versus other psychotherapyf | ||||||
| All studies | 13 | 0.04 | –0.14 to 0.21 | 39.81 | 45.45 | |
| One effect size per study (highest) | 10 | 0.01 | –0.20 to 0.21 | 44.59 | 166.67 | |
| One effect size per study (lowest) | 10 | 0.00 | –0.20 to 0.19 | 41.11 | — | |
| HAM-D only | 10 | 0.12 | –0.07 to 0.31 | 19.04 | 14.71 | |
| BDI only | 7 | 0.28 | –0.02 to 0.57 | 45.46 | 6.41 | |
| Studies on dysthymia excluded | 11 | 0.01 | –0.18 to 0.20 | 42.09 | 166.67 | |
| Subgroup analysese | ||||||
| Adapted manual | ||||||
| Yes | 7 | –0.09 | –0.25 to 0.07 | 0.00 | 0.098 | 20.00 |
| No | 6 | 0.25 | –0.12 to 0.63 | 62.27* | 7.14 | |
| Comparison group | ||||||
| CBT | 9 | –0.04 | –0.23 to 0.16 | 39.72 | 0.113 | 45.45 |
| Other psychotherapy | 4 | 0.27 | –0.06 to 0.59 | 4.68 | 6.58 | |
| Target group | ||||||
| Adults | 8 | –0.08 | –0.24 to 0.08 | 0.00 | 0.116 | 21.74 |
| More specific group | 5 | 0.31 | –0.15 to 0.77 | 69.51* | 5.75 | |
| Intent-to-treat analysis | ||||||
| Yes | 9 | 0.16 | –0.06 to 0.38 | 35.74 | 0.106 | 11.11 |
| No | 3 | –0.13 | –0.40 to 0.15 | 0.00 | 13.51 | |
| IPT versus pharmacotherapyf | ||||||
| All studies | 10 | –0.12 | –0.36 to 0.12 | 61.98** | 14.71 | |
| Outlier removedg | 9 | –0.19* | –0.38 to –0.01 | 30.95 | 9.43 | |
| HAM-D only | 8 | –0.16 | –0.43 to 0.11 | 57.39* | 11.11 | |
| BDI only | 3 | –0.31 | –0.72 to 0.09 | 40.39 | 5.75 | |
| Studies on dysthymia excluded | 7 | –0.12 | –0.33 to 0.09 | 23.78 | 14.71 | |
| Subgroup analysese | ||||||
| Medicationh | ||||||
| SSRI or SNRI | 3 | –0.39** | –0.68 to –0.11 | 14.18 | 0.037 | 4.59 |
| Tricyclic antidepressant | 4 | –0.02 | –0.22 to 0.19 | 0.00 | 83.33 | |
| Intent-to-treat analysis | ||||||
| Yes | 5 | –0.15 | –0.42 to 0.13 | 45.10 | 0.450 | 11.90 |
| No | 4 | –0.28* | –0.50 to –0.06 | 0.00 | 6.41 | |
| Pharmacotherapy versus combination treatmenti | ||||||
| All studies | 10 | 0.16 | –0.03 to 0.36 | 39.26 | 11.11 | |
| HAM-D only | 8 | 0.21 | –0.11 to 0.52 | 64.64** | 8.47 | |
| BDI only | 2 | 0.10 | –0.20 to 0.41 | 0.00 | 17.86 | |
| Studies on dysthymia excluded | 7 | 0.22 | –0.03 to 0.47 | 44.17 | 8.06 | |
| Subgroup analyses | ||||||
| Adapted manual | ||||||
| Yes | 5 | 0.23 | –0.04 to 0.51 | 50.15 | 0.494 | 7.69 |
| No | 5 | 0.08 | –0.25 to 0.41 | 40.50 | 21.74 | |
| Medication | ||||||
| SSRI | 5 | 0.07 | –0.27 to 0.41 | 64.96* | 0.562 | 25.00 |
| Tricyclic antidepressant | 2 | 0.33 | –0.11 to 0.76 | 0.00 | 5.43 | |
| Other/protocol | 3 | 0.27 | –0.00 to 0.54 | 0.00 | 6.58 | |
| Target group | ||||||
| Adults | 5 | 0.07 | –0.12 to 0.27 | 0.00 | 0.569 | 25.00 |
| More specific group | 5 | 0.19 | –0.16 to 0.54 | 61.35* | 9.43 | |
| Intent-to-treat analysis | ||||||
| Yes | 6 | 0.12 | –0.10 to 0.34 | 23.03 | 0.391 | 14.71 |
| No | 4 | 0.35 | –0.12 to 0.82 | 63.84* | 5.10 | |
IPT Compared With Other Psychotherapies
IPT Compared With Pharmacotherapy
IPT Compared With Combination Treatment
IPT as Maintenance Treatment
Discussion
Footnote
Supplementary Material
- View/Download
- 13.21 KB
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

