One of the conundrums in developmental child psychopathology stems from the fact that most of the defining clinical signs of psychiatric disorders also occur in normally developing children. This phenomenon has fueled controversy regarding the boundaries that define deviance and psychopathology, the point at which their joints lie, and where to carve them. Ambiguity regarding the limits between normalcy and pathology is not trivial, since it has been seized upon to call into question the whole enterprise of classifying psychiatric disorders and to claim that the nomenclature erroneously medicalizes normal variations of children's behavior. The phenomenal success of psychostimulants for attention deficit hyperactivity disorder (ADHD) has been particularly provocative and has led to accusations that the medications have the exclusive role of satisfying school personnel intolerant of normal exuberant behavior—never mind the child's unhappiness and failure to meet his own goals. Moreover, critics of ADHD do not take into consideration that childhood ADHD predicts specific patterns of dysfunction and multiple disadvantages (e.g.,
1–3). The main argument often advanced is that, in the absence of any “physical” abnormality, there is no justification for considering ADHD as a disorder.
The first brain volumetric studies of ADHD (
4), from the same research branch at NIMH as the study by Shaw et al. (
5) in this issue of the
Journal, documented that children with the disorder had significant cortical thinning and reductions of total brain volume. Longitudinal studies soon followed, showing that cortical thinning followed a developmental trajectory that differentiated children with ADHD and comparison youths (
6). Volumetric differences were replicated and extended to affected adults (i.e.,
7). Furthermore, cortical thinning was reported to be associated with a specific genetic variant,
DRD4 7-repeat allele, which in turn predicted a relatively favorable outcome. For the first time, genotype, clinical outcome, and cortical change were linked to the diagnosis of ADHD and its course (
8). There was a sense of relief that, at long last, research had documented brain abnormalities (read “physical”) in ADHD.
The Shaw et al. (
5) study tackles a different question: whether normal developmental cortical thinning differs as a function of diagnosed ADHD (as previous brain imaging studies suggested) or whether the rate of thinning is related to the level of ADHD behaviors across all children. The study reports that cortical thinning over time is inversely related to the degree of severity of hyperactivity/impulsivity by maternal ratings, even in the absence of a full diagnosis of ADHD. In all children, the more severe ADHD behaviors or symptoms, the slower the rate of cortical thinning. The finding of a linear relationship between levels of severity of ADHD symptoms and slower cortical thinning is a strong argument in support of the meaningfulness of the relationships found. Previous population and twin studies have obtained results indicating that ADHD severity lies on a continuum, but the Shaw et al. report is the first to link the latter to a neurobiological abnormality.
Do such findings revive the controversy regarding ADHD as a variant of normal development, rather than a distinct disorder, and do they invalidate or call into question current standards for establishing a diagnosis of ADHD? The Shaw et al. study confirms, as previous studies have shown, that 1) increased motor activity and impulsivity are symptomatic expressions of brain pathology and 2) the brain abnormality is developmental. Nonetheless, as real as the differential rates of normal cortical thinning are, they do not illuminate exactly how the brain fails to regulate impulse control and motor activity in ADHD. Nor does the study demonstrate that diagnosed ADHD is a simple quantitative difference along a continuum of underlying pathophysiology. It seems most unlikely that a complex, heterogeneous behavioral syndrome will be explained by a single neuroanatomical difference. Indeed, the authors of the article make no such claims and are right on the mark in noting that “alterations in cortical growth rates will be only one of the many neural changes shown to reflect or drive ADHD.”
The study stands out as the first to report on the developmental course of one of these differences (i.e., slower timing of thinner cortices). The body of work from this NIMH research group is important in highlighting that ADHD, at least in some instances, may be a developmental disorder, with delay in the timing of normal brain changes. If so, we should expect children with ADHD to reach levels of function similar to their normal peers, albeit later in life. Indeed, this expectation is consistent with findings that ADHD symptoms remit in late adolescence or early adulthood in a proportion of diagnosed children. It is not yet established that volumetric brain studies fully inform the identification of different long-term trajectories in ADHD, but there is evidence that they are contributory (
8). Developmental brain studies, such as this one, have great potential for providing key information to elucidate the marked variations found in the long-term outcome of children with ADHD.
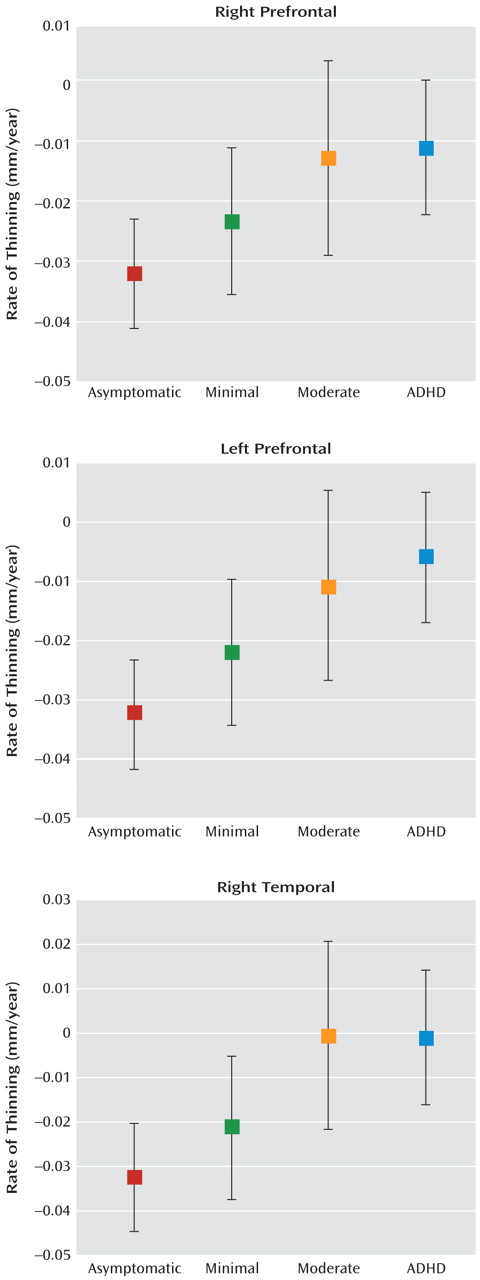
Shaw et al. present striking data showing that the rate of prefrontal cortical thinning is significantly different, indeed almost nonoverlapping, between those with no ADHD symptoms and those who meet full diagnostic criteria, reaffirming the evidence for a neurobiological basis of the diagnosis of ADHD (see
Figure). Use of these developmental data as clinical biomarkers for ADHD would be premature, however, until effect size, specificity, and sensitivity as well as the effects of outliers can be fully established. We can also see from Figure 3 in the article that there is considerable overlap in cortical thinning across groups with different levels of ADHD symptoms. This pattern of findings indicates that we have not reached the goal of identifying a marker for ADHD. To put it differently, the developmental differences found in rates of cortical thinning, albeit impressive, do not have clinical implications for the diagnosis or care of individuals with ADHD symptoms. A longitudinal study of children with ADHD (
9), who now have been followed at age 41, is relevant to this caveat. The as yet unpublished findings confirm thinner cortices in ADHD subjects than in non-ADHD comparison subjects, including in regions that underpin attentional control. However, there was no difference in cortical thicknesses between those whose ADHD had remitted and those in whom it had persisted, suggesting that the anatomical differences found are not sufficient to explain the clinical phenomenon.
Thus, Shaw et al. present us with an important finding about the developmental biology of ADHD. Their work identifies a long-sought biological element of the biopsychosocial model of ADHD, but it is only one element. Decisions for individual patients faced with ADHD, whether they be prevention, diagnosis, treatment, or prognostic estimates, still require our clinical hats.