Epidemiological research has demonstrated an association between childhood trauma and the development of psychotic disorder, psychotic symptoms, and subthreshold psychotic experiences—i.e., across the extended psychosis phenotype (
1,
2). However, two reviews suggest that methodological issues may limit the conclusions that can be drawn with regard to this putative association (
3,
4). Possible limitations include small study groups, the use of chronically ill patients, lack of comparison subjects, groups with mixed psychopathology, lack of validated assessment of trauma and psychosis symptoms, reporting bias (psychotic symptoms occasioning reporting of trauma), greater likelihood of childhood trauma due to genetic risk for schizophrenia (gene-environment correlation or genetic confounding), and reverse causality (overt psychosis causing victimization).
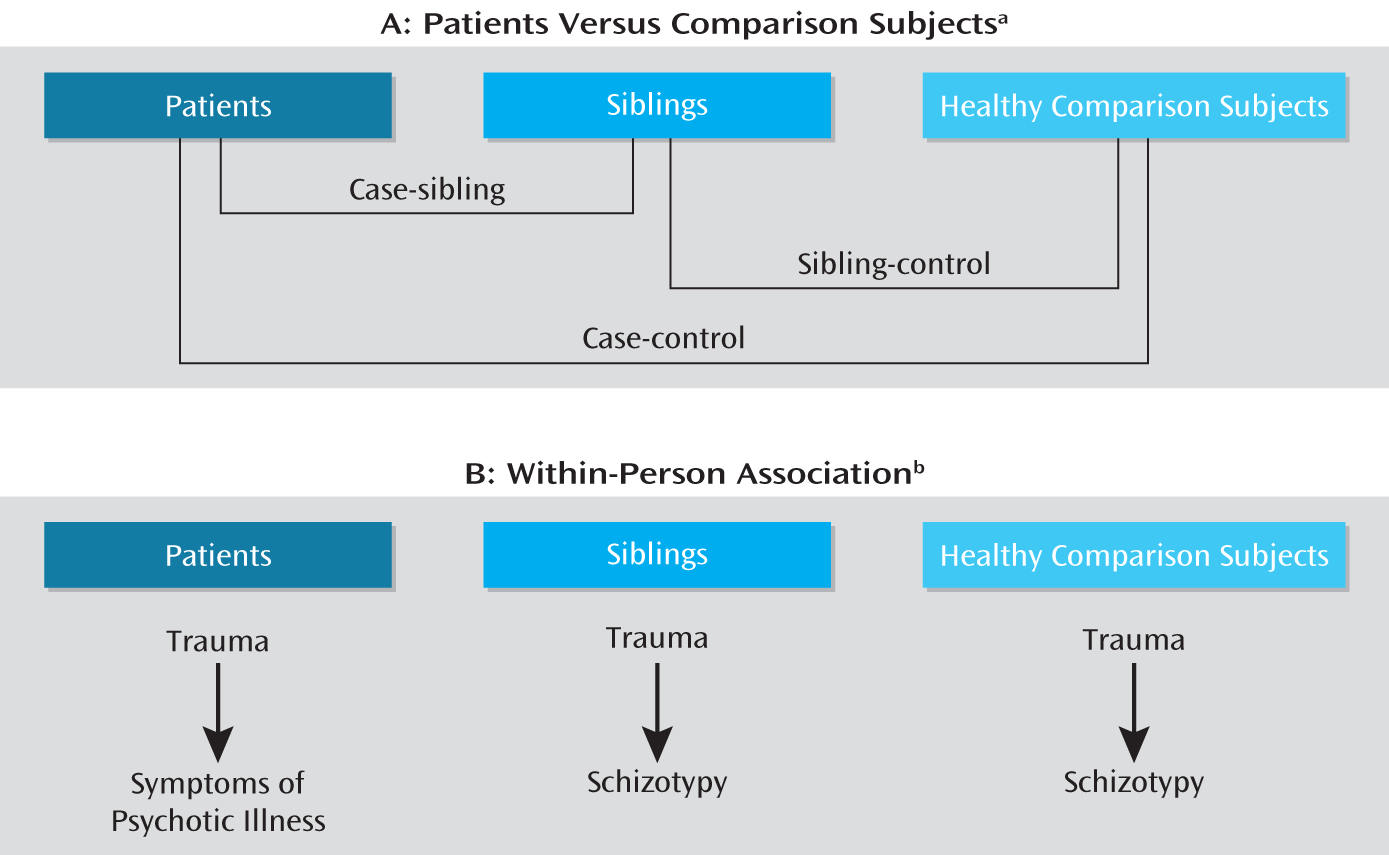
In the current study, a number of strategies were used in an attempt to estimate the true level of association between trauma and psychosis (
Figure 1). First, comparisons of patients and healthy subjects, patients and siblings, and siblings and healthy subjects were conducted to a) allow for adjustment for possible familial confounding, given the fact that siblings are matched on a range of measured and nonmeasured sociodemographic, parental, developmental, and genetic factors that may confound the association between childhood trauma and expression of psychosis (
5), and b) verify the validity of the patients' exposure reports, if the rate of trauma exposure in siblings is intermediate between the rates of patients and comparison subjects (
Figure 1A). Second, assessing the within-person association between trauma and psychosis across the groups with illness (patients), high vulnerability for psychotic illness (siblings of patients), and average vulnerability (healthy comparison subjects) allowed us to examine whether an association between trauma and psychosis is observed only in the ill group, possibly indicating reporting bias, gene-environment correlation, or reverse causality. These mechanisms are unlikely if associations between trauma and expression of (subthreshold) psychosis are also observed in the high- and average-vulnerability groups (
Figure 1B). Third, a well-validated measure of childhood trauma was used. Fourth, we focused on specific symptoms, which may represent a more valid outcome for this type of etiological research (
6). Given the fact that childhood trauma has been linked to increased reactivity to stress (
7,
8) and stress reactivity may contribute to the positive symptoms of psychosis (
7,
9), it was hypothesized that childhood trauma is associated specifically with the positive symptoms of psychosis, as suggested by some studies (
10,
11). Fifth, we examined two types of childhood trauma. Most studies have treated childhood trauma as a single exposure. However, childhood abuse and childhood neglect may be associated with different symptoms (
12), given their possible differential effects on the brain. Sixth, we examined whether sex moderated the association between trauma and psychosis. One study has suggested that the association between childhood trauma and psychosis may be sex specific (
13), but this was not replicated in another study (
14). We hypothesized the following:
1. Positive associations with trauma would be evident, in a dose-response fashion, in the comparisons of patients and healthy subjects, patients and siblings, and siblings and healthy subjects, regardless of sex.
2. If the patient reports of trauma are valid, then the healthy siblings, growing up in the same environment, would share some of the trauma reported by the patients (
15) (i.e., an association in this direction would be expected in the comparison of siblings and healthy subjects); however, the siblings would also have lower rates of exposure than the patients.
3. Trauma would be associated with expression of psychosis in all three groups, indicating that the association is not likely the result of genetic risk for psychotic disorder (as the healthy comparison subjects were not at genetic risk), reporting bias, or reverse causality (as the siblings and healthy comparison subjects were not ill).
4. Abuse and neglect would be associated with different symptoms.
Method
Participants
The study group consisted of patients with a diagnosis of nonaffective psychotic disorder, their siblings, and healthy comparison subjects from the general population in the context of the Dutch national Genetic Risk and Outcome in Psychosis (GROUP) project (
16). In selected representative geographical areas in the southern part of the Netherlands and Belgium, patients were identified through a number of representative clinicians whose caseloads were screened for the inclusion criteria. Subsequently, a group of patients seen consecutively at these services as either outpatients or inpatients were recruited for the study. Siblings were recruited through the participating patients. Comparison subjects were recruited through random mailings (75%) and local newspaper advertisements (25%) in municipalities reflecting the mix of urbanization levels in the catchment areas of the mental health institutions.
The inclusion criteria included fluency in Dutch and age between 16 and 55 years. The patients were also required to have a DSM-IV diagnosis of nonaffective psychotic disorder, assessed by clinical interview with the Comprehensive Assessment of Symptoms and History (
17), and a first contact with mental health facilities within the last 10 years. For each participating patient, at least one sibling had to take part in the study. This criterion was fulfilled for 86% of the patients. Siblings were included irrespective of participation by their ill relatives, but almost all siblings (96%) were matched by at least one patient relative. Sibling nonpatient status was defined as the absence of any lifetime psychotic disorder according to the Comprehensive Assessment of Symptoms and History. For the healthy comparison subjects, the occurrence of any psychotic disorder in either the subject, according to Comprehensive Assessment of Symptoms and History, or any first-degree family member, as determined with the Family Interview for Genetic Studies (
18), constituted an exclusion criterion. After complete description of the study to the subjects, written informed consent was obtained in conformance with the local ethics committee guidelines.
Measures
Childhood trauma was assessed with the Dutch version of the 25-item short form of the Childhood Trauma Questionnaire (
19), consisting of 25 items rated on a 5-point Likert scale (1=never true, 5=very often true). Emotional, physical, and general childhood abuse were assessed, along with emotional and physical neglect; five items covered each trauma type (
19). The mean score for all 25 items was used as the total trauma rating (range=1.00–4.28); the abuse rating was the mean score on the 15 abuse items (range=1.00–4.53), and the rating of neglect was the mean score on the 10 neglect items (range=1.00–4.10). As the trauma scores were highly skewed, the variables were dichotomized a priori into high trauma and low trauma. The cutoff was defined as the 80th percentile of scores for the healthy comparison subjects. For the total trauma rating, subjects having ratings of 1.56 or higher were in the high-trauma group. For the abuse scores the cutoff was 1.40, and for neglect it was 1.90.
The symptom dimensions of psychosis were assessed with the Positive and Negative Syndrome Scale (PANSS) (
20). The PANSS is a semistructured interview consisting of three subscales: positive symptoms (seven items), negative symptoms (seven items), and general psychopathology (16 items). All items are scored on a scale of 1 (not present) to 7 (severe). The mean scores for the positive symptom items, negative symptom items, and general psychopathology items were used in the analyses.
The subclinical psychosis symptom dimensions were assessed with the Structured Interview for Schizotypy—Revised (
21), a semistructured interview containing 20 schizotypal symptoms (verbal responses to standardized questions) and 11 schizotypal signs (behaviors rated by the interviewer), rated on a 4-point scale. The questions and rating procedures are standardized. The item scores were reduced a priori to two dimensional scores (
22), representing the mean scores for positive schizotypy items (referential thinking, psychotic phenomena, derealization, magical ideation, illusions, and suspiciousness; range=0.00–2.57) and negative-disorganized schizotypy items (social isolation, sensitivity, introversion, restricted affect, disturbances in associative and goal-directed thinking, poverty of speech, eccentric behavior; range=0.00–1.25).
Statistical Analysis
In order to investigate the relationship between trauma and psychotic disorder by comparing patients and healthy comparison subjects, patients and siblings, and siblings and healthy comparison subjects, multilevel logistic regression models were estimated. Multilevel analyses were used since the patients, siblings, and some healthy comparison subjects were related, violating the assumption of independence of observations. The data were analyzed by using the XTGEE routine in Stata 11.1 (Stata, College Station, Tex.). Furthermore, the interaction between trauma and sex (0=male, 1=female) was tested. All analyses were a priori corrected for the possible confounding effect of age. In order to assess whether associations between total trauma and psychosis displayed a dose-response relationship, the continuous trauma scores of the patients, siblings, and healthy comparison subjects were divided by the quartile values of the distribution of the total trauma score in the healthy comparison subjects, thus creating four quartile groups for the exposure variable.
In order to examine the association between childhood trauma and clinical symptoms in the patient group, multilevel logistic regression models were estimated with binary childhood trauma (abuse or neglect) as the dependent variable and the three PANSS symptom dimensions as independent variables, first separately and later jointly in order to assess the independence of associations; the analyses were a priori corrected for age and sex. Similar analyses were conducted in the sibling group and in the healthy comparison group by using the two schizotypy dimensions as independent variables. In order to assess whether associations between trauma and psychopathology displayed a dose-response relationship, the rating of dichotomous trauma exposure was examined across quartile groups of psychopathology.
Results
Subject Characteristics
A total of 272 patients, 258 of their siblings, and 227 healthy comparison subjects were included in the analyses (
Table 1). Four patients had no data on the PANSS, and five siblings and four healthy comparison subjects had no ratings on the Structured Interview for Schizotypy—Revised; these subjects therefore were excluded from the analyses.
Sex was associated with dichotomously defined childhood abuse (women: 28%, men: 22%); the odds ratio was 1.32, with a 95% confidence interval (CI) of 0.95–1.84, although the difference was not statistically significant (p=0.10). Sex was associated with neglect to a similar degree, but in the opposite direction (women: 29%, men: 35%; odds ratio=0.74, 95% CI=0.55–1.01, p=0.06), and the relationship to overall trauma did not approach significance (men: 32%, women: 33%; odds ratio=0.89, 95% CI=0.66–1.21, p=0.47).
Between-Group Comparisons
Trauma was associated with psychotic disorder in the case-control (odds ratio=4.53, 95% CI=2.79–7.35, p<0.001), case-sibling (odds ratio=2.60, 95% CI=1.78–3.78, p<0.001), and sibling-control (odds ratio=1.61, 95% CI=0.95–2.61, p=0.05) comparisons, and there was evidence of a significant dose-response relationship across the trauma quartile groups (
Table 2). Similar results were apparent separately for neglect (case-control: odds ratio=4.05, 95% CI=2.51–6.52, p<0.001; case-sibling: odds ratio=1.96, 95% CI=1.37–2.81, p=0.009; sibling-control: odds ratio=1.85, 95% CI=1.16–2.96, p<0.001) and for abuse (case-control: odds ratio=4.38, 95% CI=2.71–7.06, p<0.001; case-sibling: odds ratio=3.43, 95% CI=2.22–5.28, p<0.001), with the exception of the sibling-control comparison of abuse, although this association was in the same direction (odds ratio=1.28, 95% CI=0.78–2.10, p=0.34).
Sex did not moderate the association between psychotic disorder and trauma. The effect was not significantly greater for female than male subjects in the case-control (odds ratio=0.73, 95% CI=0.27–1.98, p=0.55), case-sibling (odds ratio=1.22, 95% CI=0.57–2.64, p=0.61), or sibling-control (odds ratio=0.64, 95% CI=0.23–1.78, p=0.39) comparison.
Trauma and Symptoms in Patient Group
In the patient group, total childhood trauma was significantly associated with positive symptoms and general psychopathology (
Table 3). No significant association was found between total childhood trauma and negative symptoms. Entering positive symptoms and general psychopathology together in the model revealed that positive symptoms (odds ratio=1.85, 95% CI=1.18–2.91, p<0.007) but not general psychopathology (odds ratio=0.98, 95% CI=0.50–1.94, p=0.96) remained significantly associated with total trauma.
Abuse was associated significantly with both positive symptoms and general psychopathology but not with negative symptoms (
Table 3). Moreover, when both positive symptoms and general psychopathology were added to the model, only the association with positive symptoms remained (positive symptoms: odds ratio=1.73, 95% CI=1.12–2.67, p<0.02; general psychopathology: odds ratio=1.40, 95% CI=0.71–2.77, p=0.34).
For neglect, significant associations were found with positive symptoms and general psychopathology (
Table 3). However, the association with positive symptoms all but disappeared when general psychopathology was entered in the model (positive symptoms: odds ratio=1.14, 95% CI=0.74–1.75, p=0.56; general psychopathology: odds ratio=1.86, 95% CI=0.94–3.67, p=0.07).
Since abuse was associated most strongly with the positive symptoms of psychosis, a dose-response association was investigated by using quartile groups of the positive symptom dimension. A monotonic dose-response relationship was apparent, with increasing proportions of patients with childhood trauma across the quartile groups of positive symptoms (
Table 4).
Trauma and Symptoms in Sibling and Healthy Comparison Groups
In the sibling group, total trauma was associated with neither the positive nor the negative schizotypy dimension (
Table 3). In the healthy comparison group, a significant association was found with the positive schizotypy dimension (
Table 3).
As in the patient group, abuse was associated significantly with the positive but not the negative schizotypy dimension, in both the sibling and comparison groups (
Table 3).
Neglect was associated significantly with the positive and negative schizotypy dimensions in the healthy comparison subjects but not in the siblings (
Table 3). When entered together in the model, positive but not negative schizotypy symptoms remained associated with neglect in the comparison group.
A dose-response association was found, with a progressively greater proportion of abuse exposure in both siblings and healthy comparison subjects across the quartile groups of subthreshold positive symptoms (
Table 4).
Discussion
Reviews on the association between childhood trauma and psychosis have not been consistent (
1–
4). Since these reviews were published, however, an explosion of methodologically strong studies have all demonstrated associations between childhood trauma and psychotic symptoms or psychotic disorder (
11,
13,
23,
24); these include a number of prospective studies (
14,
25–
28).
The findings of the current study agree with the more recent results and extend them, showing that 1) patients diagnosed with a psychotic disorder within the first 10 years of their illness reported significantly more childhood trauma compared to not only healthy comparison subjects but also the patients' siblings; 2) the rates of reported trauma were higher for the patients' siblings than for the healthy comparison subjects, thus validating the reporting of trauma by the patients; 3) the association between trauma and psychopathology was constant regardless of whether it was examined in individuals with illness, high genetic risk, or average genetic risk, making it unlikely that the findings are the result of gene-environment correlation, illness-related reporting bias, or reverse causality; 4) dose-response associations were found, showing progressively higher levels of abuse in participants with greater levels of clinical or subthreshold positive symptoms, which may support, but does not prove, causality (
29); 5) childhood trauma in the form of abuse was associated specifically with positive symptoms of clinical psychosis, whereas the results for neglect were less clear; and 6) women tended to report higher levels of abuse, but no sex differences were found in the association between trauma and psychosis.
Childhood Trauma and Psychosis
In the current study we attempted to overcome several of the methodological problems that were identified in previous reviews (
1,
3,
4). We used a large, representative group of patients with nonchronic psychosis (i.e., with a duration less than 10 years and less than 5 years in most cases) and healthy volunteers selected through random mailings and sibling comparison subjects. Siblings are far more likely than population comparison subjects to provide adequate control for a range of unmeasured familial confounding factors, particularly early-life factors that are shared by siblings (
5), most notably a family history of psychiatric disorder. In addition, both childhood trauma and clinical and subthreshold psychotic symptoms were assessed with validated measures and interviews (
19,
21). Consequently, the results of the current study provide strong additional support for an association between childhood trauma and development of psychosis.
The siblings reported significantly less abuse and neglect compared to their ill relatives. This strongly suggests that discordance in psychotic illness among siblings may be associated with discordance in trauma exposure. It has been shown that harsh parental behavior directed at one person in the family may have protective effects for other children in the family, a phenomenon called the “sibling barricade” (
30). This suggests that, given shared genetic liability, differential exposure to trauma may result in illness in only one of a sibling pair (
15). It is interesting that the comparisons with the healthy subjects suggested that the patients may have been exposed more to abuse than their siblings, while the siblings may have experienced more neglect than the patients.
The higher trauma rates in the patients could be due to recall bias, i.e., the patients may have recalled traumatic events that never took place or were exaggerated. However, several studies have shown that retrospective self-reports of childhood trauma in both healthy subjects and psychiatric patients are valid (
31) and are more likely to be an underestimation of the true prevalence of childhood maltreatment (due to forgetting or unwillingness to report the maltreatment) than an overestimation (
32).
Abuse and Positive Symptoms
The current study adds evidence to the notion that childhood trauma is specifically associated with the development of positive psychotic symptoms. These data fit with the results of several other studies showing an association between childhood abuse and the positive symptoms of psychosis (
12). One study did not find an association between trauma and positive psychotic symptoms; however, these authors reported on a small, all-female patient group (
33). In addition, the current study showed that childhood abuse, more than childhood neglect, is associated significantly with both clinical and subthreshold positive psychotic symptoms, which is in accordance with findings in other studies (
34). Childhood neglect, on the other hand, was associated with general psychopathology in the patient group. From a neurodevelopmental perspective, abuse and neglect are believed to have distinct effects on the developing brain. Neglect is defined as an absence of adequate care or protection during childhood, and from a neurobiological perspective this means that the developing brain is deprived of stimulating positive experiences. Growing up under neglectful circumstances is shown to be related to several cognitive and psychosocial deficits in children, e.g., language problems, low intelligence, and poor mentalizing ability (
35). Childhood experiences of abuse are considered highly stressful and are assumed to alter the brain systems that are responsible for mediating the stress response (
36).
Childhood trauma is associated with a range of mental health outcomes, notably affective disorders (
37). Given the strong association between psychosis and affective dysregulation (
38), part of the link between trauma and psychotic disorder may be mediated by affective dysregulation.
Gender Differences in Trauma Exposure and Associated Symptoms
The finding that women tended to report more abuse than men is in agreement with the observations of Fisher and colleagues (
13). However, in contrast to the findings in that study, the associations between trauma and psychosis were significant in both men and women, as reported in another recent study (
14).
Limitations
First, childhood trauma was measured by using a retrospective, self-report questionnaire. While this may raise the issue of reliability, as previously discussed, studies on the use of self-report, retrospective measures of childhood abuse in patient groups indicate that such reports are reliable (
31,
39). Furthermore, we used the Childhood Trauma Questionnaire, a well-validated and reliable measure of childhood trauma. Nevertheless, it does not take into account the subject's age at the occurrence of the trauma, the subject's relationship to the perpetrator, or the severity of the experience, all of which may influence the association with psychosis. Also, other forms of childhood trauma—such as bullying, loss of a parent, and exposure to domestic violence—were not considered in this study. Second, the correlational and retrospective design of the study allows for conclusions about association but cannot be used to establish a causal link between the trauma and psychosis. However, a causal association may exist, given the relatively strong effect sizes, the evidence of a dose-response relationship, some evidence for biological plausibility, and the temporal order, i.e., childhood trauma preceding the development of positive symptoms (with the limitation that the Child Trauma Questionnaire does not assess the age at occurrence, and so some expressions of schizotypy may have preceded childhood trauma). Third, not all possible mediating factors were assessed and taken into account. Fourth, while the results of the comparison of the siblings and healthy subjects and the associations between trauma and psychosis within the siblings and within the healthy subjects argue against an association between trauma and chronicity, rather than onset of psychotic illness, we conducted post hoc analyses to look for an association with childhood trauma (abuse or neglect) in the case-control comparison, restricting the patient group to those with prodromal or clinical symptoms for less than a year (N=28) or less than 3 years (N=98). The resulting odds ratios remained large and significant although somewhat attenuated (symptoms <1 year: odds ratio=2.80, 95% CI=1.04–7.57; symptoms <3 years: odds ratio=1.93, 95% CI=1.06–3.49). Fifth, case-control studies are sensitive to selection bias. Only 70% of the mental health institutions in the selected area participated in the study, which may have introduced differential selection that affected the results. If trauma affects outcome in patients, the use of a prevalence sample may inflate exposure rate. The rate of refusal by healthy comparison subjects (in those written to) was well in excess of 50%. To the degree that participation of comparison subjects in studies may be influenced by self-selection of individuals with subthreshold syndromes, the reported comparisons of the patients and comparison subjects may be considered conservative. On the other hand, it is possible that comparison subjects with a history of trauma are less likely to take part in a study, possibly resulting in an overestimation of the effect. However, the patient-sibling analysis excluded bias due to differential nonparticipation, as members of each pair were compared together or not, precluding differential nonparticipation. Finally, the association between childhood trauma and PANSS scores in the patients is interpretable to the degree that essentially cross-sectional PANSS scores pick up trait differences in the level of positive symptoms between patients. This analysis has low sensitivity, given the fact that the PANSS is also sensitive to fluctuating state differences in psychopathology, creating “noise” that may easily obscure trait associations.