There has been a resurgence of interest in early-life risk factors for schizophrenia (
1). Recent results from genetics studies converge with existing evidence from epidemiology and point to a neurodevelopmental etiology for schizophrenia (
2). Given the multifactorial nature of the causal pathway to schizophrenia (
3), studies should move toward examining how early-life risk factors may interact with each other to set up a trajectory of aberrant development.
Evidence for childhood motor developmental abnormalities preceding schizophrenia onset are well documented in both high-risk studies and general birth cohort data (
4–
12). Early neuromotor deficits appear to be specific to schizophrenia (
7) and exhibit a dose-response relationship with risk of later development of the illness (
6,
9). Likewise, there is strong evidence for the role of obstetric complications in the etiology of schizophrenia (
13–
19), with a wide range of prenatal and perinatal risk factors associated with the risk of developing the illness. However, although some investigators have controlled for the presence of obstetric complications when studying developmental risk factors for schizophrenia (
7), no study has yet—to our knowledge—examined a possible association between obstetric complications and developmental delay in relation to schizophrenia outcomes.
One could conceptualize three possible explanations for the relationship between these two risk factors (or risk markers) for schizophrenia. First, obstetric complications and developmental delay could be manifestations of a common underlying aberrant developmental pathway or trajectory established early in fetal life (either genetic in origin or secondary to a prenatal insult, such as infection [
16] or nutritional deficiency [
17]). Second, obstetric complications and developmental delay may be independent risk factors for schizophrenia. Third, the relationship could be that of a “two-hit” interaction model, whereby obstetric complications would interact with an underlying developmental vulnerability.
We sought to examine these three possibilities using a large population-based data set from Finland. Our study design has several methodological advantages. First, we minimized selection bias by using register linkage between population-based registers. Second, our use of a nested case-control design is resource efficient and combines the advantages of both case-control and cohort study designs. Third, we minimized recall bias by obtaining both obstetric and developmental information from prospectively collected child health cards.
Method
Study Design
This was a matched case-control study nested within a 7-year birth cohort. All live-born individuals in Finland are assigned a unique personal identification number at birth. This personal identification number is used in all national registers, which ensures accurate linkage of information between registers. For this study, two registers were linked: the Finnish Hospital Discharge Register and the Finnish Population Register. The Finnish Hospital Discharge Register encompasses all public and private hospitals in Finland, and the discharge diagnoses for each admission are made by the attending physician. The diagnostic validity of the Finnish Hospital Discharge Register was examined against DSM-III-R criteria and has been found to have excellent (92%–100%) specificity for diagnoses of schizophrenia (
20). The Finnish Population Register records information on the date and place of birth, date of death, current residence, marital status, and first-degree relatives for each Finnish citizen. These registers are maintained in computerized databases by the National Institute for Health and Welfare in Finland.
Study Population
The base study population encompassed all individuals born in Helsinki between January 1, 1962, and December 31, 1969.
Case Definition
The primary outcome of interest was defined as having ever received a diagnosis of schizophrenia or schizophrenia spectrum disorder up to December 31, 2000.
Psychiatric outcomes were determined by linkage between the Finnish Hospital Discharge Register and the Finnish Population Register. Psychiatric diagnoses are recorded in the Finnish Hospital Discharge Register using the ICD system. Diagnoses before 1987 were determined using ICD-8, diagnoses between 1987 and 1995 were determined using ICD-9, and diagnoses since 1995 have been determined using ICD-10.
Our outcome measure was a broad classification of schizophrenia spectrum disorders that encompassed the following ICD categories: ICD-8/9 codes 295 (schizophrenia), 297 (delusional syndrome), 298 (reactive psychosis), and 299 (childhood origin psychoses) as well as ICD-10 codes F20 (schizophrenia), F21 (schizotypal disorder), F22 (delusional syndrome), F23 (psychotic episode), F24 (induced delusional syndrome), F25 (schizoaffective syndrome), F28 (other psychoses), and F29 (psychosis not otherwise specified).
Exposure Measurements
Child health care and monitoring in Finland are provided by public health nurses and primary care physicians. Infants receive an initial home visit from a public health nurse when they are 8–14 days old, after which they attend a child health center monthly for the first year of life. At every visit, nurses complete a standard form with measurements and information about milestones. This form, known as a child health card (or Terveyskortti), was introduced into general use in 1962. Child health cards are stored alphabetically by year of birth in the Child Health Archives. For this study, the records of all case subjects were manually identified, and the age (in months) at which children achieved the following motor milestones was extracted: 1) uttering first sound, 2) keeping head up, 3) grabbing at objects, 4) turning over, 5) sitting unsupported, 6) demonstrating thumb-finger grip (pincer grip), 7) standing with support, 8) walking with support, 9) standing without support, and 10) walking without support.
Obstetric Complications
The Apgar score (
21) is calculated by rating newborns on a scale of 0–2 points for each of five separate indices of fetal well-being: heart rate, color, tone, breathing, and reflexes. An Apgar score between 7 and 10 is considered normal (
22), and a low Apgar score in a full-term, otherwise well infant indicates obstetric distress (
21). A score between 0 and 3 has been associated with poor neurological outcomes, such as cerebral palsy (
23), and a score <5, used in combination with other markers of asphyxia, has been shown to identify individuals at risk of developing seizures (
24). The Apgar score is reported at 1 minute and 5 minutes after birth. We used the score taken at 5 minutes because it is more predictive of long-term outcome than the score taken at 1 minute (
22). In this study, we defined a score ≤8 as a low score because there were too few individuals with a score <7 to give us enough power to carry out a valid analysis.
Selection of Comparison Subjects
The next Helsinki-born child of the same gender and with a different surname listed after each case subject in the Child Health Archives and without a diagnosis of schizophrenia or schizophrenia spectrum disorder up to the year 2000 was selected as a comparison subject. The child health cards are stored in alphabetical order by year of birth. If the next card also belonged to a case subject, the previous card was selected instead. Comparison subjects were therefore matched to case subjects on gender and date of birth.
Analysis Strategy
All statistical analyses were conducted using STATA, version 10 (
25). Descriptive frequencies for all exposure variables and the amount of missing data for each variable were calculated. A chi-square test was used to determine whether there was a significant difference in missing data between case and comparison subjects. Logistic regression models that took account of the matching variables of sex and year of birth were run separately for each developmental milestone variable to determine whether the variable was associated with schizophrenia. Our baseline group consisted of those individuals who achieved these milestones earliest. Models were fitted with the exposure as a categorical variable and then refitted with the exposure as a linear variable. The odds ratios and 95% confidence intervals (CIs) reported are from the categorical models, and the p values reported are based on the Wald test from the linear model. All exposure variables were tested for linearity using a likelihood ratio test; any evidence against the linear model being a good fit was noted.
Developmental Delay
Individuals were categorized as being delayed on a particular milestone if they reached that milestone later than the age at which the majority of comparison subjects attained it. The majority was defined as between 51% and 80% of the group, depending on the distribution of the milestone in question. For example, 32% of comparison subjects achieved the sitting unsupported milestone at 6 months, 36% at 7 months, 19% at 8 months, and 13% at 9 months. For the purpose of this study, the majority was taken to be the 68% of those who achieved the milestone at 6 or 7 months. For the cumulative developmental delay analysis, only individuals with no missing values were included.
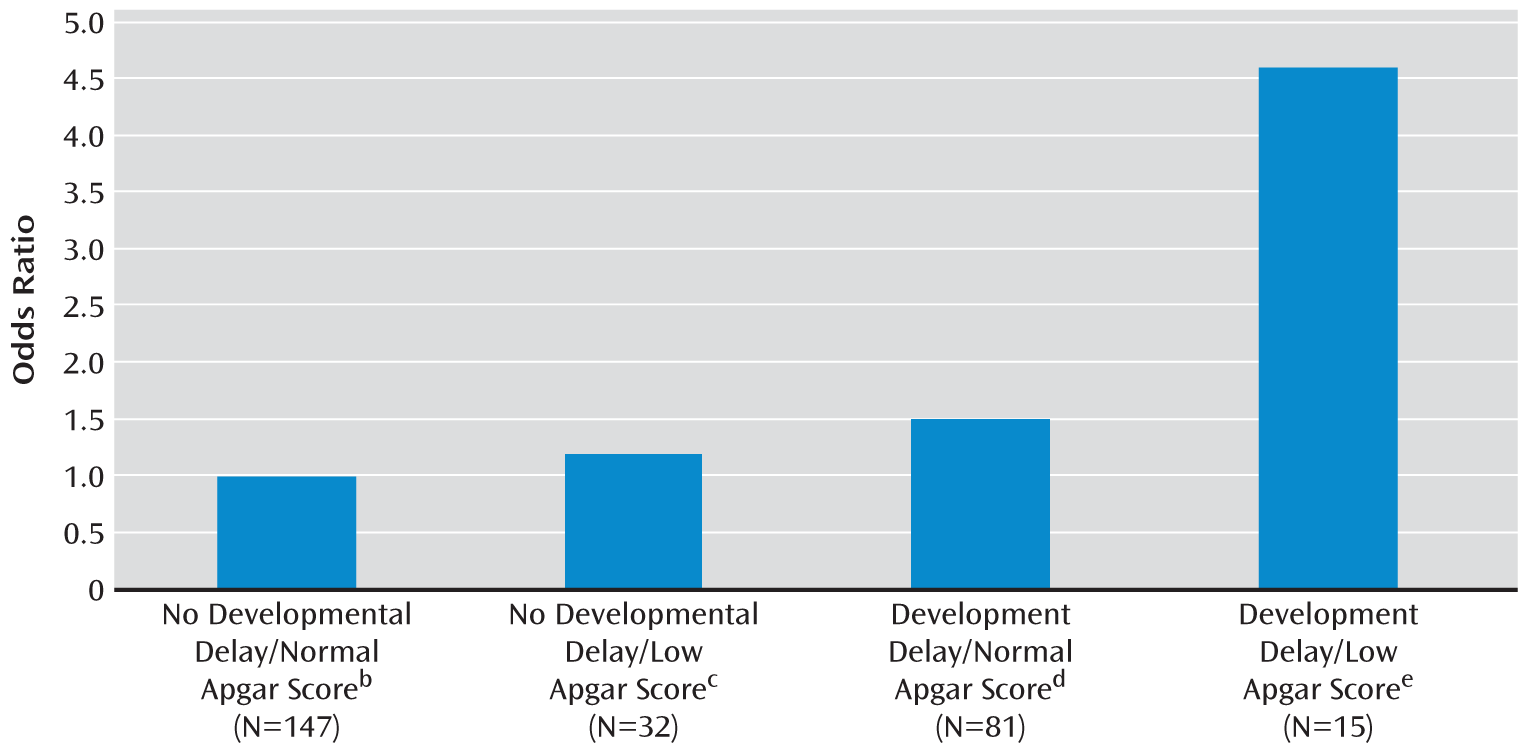
Interaction Analysis
In order to examine the additive effect of exposure to developmental delay and obstetric complications on risk of developing schizophrenia, the data were stratified on the basis of a high/low Apgar score, and we examined the effect of developmental delay within high and low score strata. Developmental delay was defined as being delayed relative to the majority of comparison subjects on at least three of the milestones. We then calculated the statistical additive interaction between developmental delay and a low Apgar score. For this we used an adaptation of an additive method that utilizes odds ratios instead of risk differences to produce an interaction contrast ratio (
26). Risk differences could not be calculated in this study because the baseline risk of schizophrenia is not available in a case-control study. Ninety-five percent confidence intervals and a p value for the interaction were calculated using the LINCOM technique in STATA (
25). The evidence indicates that additive interaction is the most appropriate method of assessing interactions in psychiatric epidemiology (
27–
29), and the majority of studies examining interactions in the etiology of psychiatric illness have used this additive approach (
30–
32).
Discussion
Our findings support previous evidence that delayed motor development in the first year of life is a relatively robust risk factor for later development of schizophrenia. In our sample, children who went on to develop schizophrenia were delayed in their attainment of motor milestones compared with children who did not develop schizophrenia. This association was present for milestones attained after age 6 months. There was no evidence that very early milestones were associated with later development of schizophrenia. The milestones that showed the strongest association with schizophrenia were those related to sitting, standing, and walking, as evidenced by strong linear trends for these milestones. Individuals who sat, stood, or walked later than the earliest developers had, on average, a two- to threefold increase in the odds of developing schizophrenia in adulthood. There was also evidence of a dose-response effect across all the milestones examined, such that the greater the number of milestones on which an individual was delayed, the higher the odds of developing schizophrenia.
Only two previous studies of schizophrenia included detailed prospective information on specific motor milestones in the first year of life: the Northern Finland 1966 Birth Cohort (
6,
10) and the Copenhagen Perinatal Cohort (
12). Our findings of delayed development across a range of early motor milestones are consistent with those from both these prior studies. The data from the Northern Finland 1966 Birth Cohort showed a dose-response effect between standing/walking and schizophrenia; the later the children stood or walked, the higher their odds of developing schizophrenia (
6,
10). Evidence from the Copenhagen Perinatal Cohort (
12) showed that infants who developed schizophrenia attained early milestones, such as sitting without support, later than those who did not develop the illness.
The present study, similar to previous work (
5,
6,
10,
12), also shows that those who develop schizophrenia do not form a readily identifiable developmental subgroup; examination of the distribution of any of the milestones presented in this study shows that individuals with schizophrenia, as a group, have a slight leftward shift in the distribution of attainment of milestones (
5,
9). This indicates the difficulty of using motor delay in childhood to identify those who will go on to develop schizophrenia in the general population. Childhood motor developmental delay, as a proxy of presumed underlying neural abnormalities, is neither a necessary nor a sufficient cause of schizophrenia, and these deficits have weak positive predictive power (
6,
8,
10,
12), as the majority of children with motor developmental delay do not go on to develop schizophrenia. However, deviations seen in the expected developmental trajectory will inform us about additional vulnerability factors that operate at critical windows in development. Our data show that the underlying vulnerability indicated by developmental delay can be amplified by the possible neurotoxic effects of obstetric complications increasing the risk of adverse outcomes.
Our study has a number of strengths. First, our nested case-control design ensured that an adequate number of cases were identified and that comparison subjects were representative of the population from which the case subjects were drawn. Second, the developmental milestone information was collected prospectively and independently of outcome status. Third, the developmental information we used was considerably more detailed than the information used in the majority of previous studies, and it was collected by trained public health nurses, using standardized measures and stored on standardized health cards, all of which gives our exposure measures a high degree of validity. A limitation of our work is the failure to find child health cards on all Helsinki-born case subjects identified from the registers. However, we have no reason to suspect that those who attended child health clinics outside the city of Helsinki differ in their risk of schizophrenia compared with those who attended clinics in Helsinki. A second limitation is the amount of missing data on individual variables on the child health cards. This is likely a result of mothers missing appointments for their infants. These assessments were frequent in the first year of life (approximately monthly), and it is quite possible that mothers were unable to make every appointment. However, there was no difference in the amount or pattern of this missing information from the child health cards for case and comparison subjects, and therefore it seems unlikely to have biased the results. A third limitation is the nonspecificity of the Apgar score in relation to the cause of obstetric complications. Knowledge of the exact cause of the obstetric complications would be informative about the specific mechanisms that may be involved in the effects we report. However, Apgar score is a recognized global measure of obstetric distress, and as such is likely to be more sensitive to the fetal condition than measurement of any one individual complication.
In our introduction, we proposed three explanations of the association between infant motor developmental delay and schizophrenia. The first hypothesis was that obstetric complications and developmental delay are manifestations of a common underlying aberrant cause (either genetic in origin or secondary to a prenatal insult, such as infection [
16] or nutritional deficiency [
17]). The second hypothesis was that obstetric complications and developmental delay are independent risk factors, and the third hypothesis was that there is an interaction between the two risk factors. The first hypothesis (common cause) is not supported by our data, since our findings show that obstetric complications do not predict developmental delay and indicate that these two risk factors for schizophrenia are not outcomes of the same underlying common cause. The second hypothesis is not supported because we found an additive effect of exposure to obstetric complications, such that when coupled with delayed motor development, the risk of schizophrenia is significantly increased relative to the risk from developmental delay without exposure to obstetric complications. Therefore, our data support the third hypothesis: an underlying vulnerability compounded by additional environmental adversity.
This is, to our knowledge, the first study to provide evidence that obstetric complications interact with developmental delay to further increase vulnerability to schizophrenia. There are a number of possible mechanisms that may explain our result. First, our findings may point to a gene-environment interaction, since motor developmental delay could be an expression of underlying genetic vulnerability (
4,
8). Second, our data could point to a genetic interaction in which the genes predisposing to a difficult birth interact with the genes for motor development or to a gene-environment correlation whereby the effects of obstetric complications and motor development seen here are under the same genetic control. However, evidence that the effect of obstetric complications on risk for schizophrenia is not a proxy for genetic risk has been shown in a number of studies (
33–
38). A third possibility is that developmental delay is not actually a genetically mediated risk factor but instead reflects some aspect of prenatal development, and our findings may represent a synergistic interaction between two or more environmental risk factors. A fourth possibility is that a single environmental process is at work, whereby an environmental factor, such as exposure to a prenatal event or stressor, could increase the likelihood of both obstetric complications and developmental delay. However, our two risk factors were not significantly associated with each other, indicating that they are probably not part of a single underlying neurodevelopmental state and that two vulnerability processes may be at work in tandem to synergistically increase risk of schizophrenia. We recommend moving away from considering risk factors in isolation and focusing on investigating aberrant trajectories of development from prenatal life through childhood and adolescence.