Antiepileptic Drugs for Bipolar Disorder and the Risk of Suicidal Behavior: A 30-Year Observational Study
Abstract
Objective:
Method:
Results:
Conclusions:
Method
Participants
Assessments
Classification of Antiepileptic Exposure
Statistical Analysis
Primary analyses: safety models.
Propensity for antiepileptic exposure.
Results
Study Sample
| Characteristic | ||
|---|---|---|
| N | % | |
| Gender | ||
| Female | 122 | 61.3 |
| Male | 77 | 38.7 |
| Marital status | ||
| Never married | 70 | 35.2 |
| Married | 77 | 38.7 |
| Divorced, separated, or widowed | 52 | 26.1 |
| Hollingshead socioeconomic status scalea | ||
| I | 4 | 2.0 |
| II | 28 | 14.1 |
| III | 68 | 34.2 |
| IV | 56 | 28.1 |
| V | 43 | 21.6 |
| Intake site | ||
| New York | 31 | 15.6 |
| St. Louis | 41 | 20.6 |
| Boston | 29 | 14.6 |
| Iowa City | 56 | 28.1 |
| Chicago | 42 | 21.1 |
| Intake status | ||
| Inpatient | 178 | 89.4 |
| Outpatient | 21 | 10.6 |
| Major depressive episodes before study intake | ||
| 0 | 43 | 21.6 |
| 1 | 32 | 16.1 |
| 2 | 30 | 15.1 |
| 3 | 19 | 9.5 |
| 4 | 17 | 8.5 |
| 5 or more | 58 | 29.1 |
| Manic episodes prior to study intake | ||
| 0 | 93 | 46.7 |
| 1 | 30 | 15.1 |
| 2 | 21 | 10.6 |
| 3 or more | 55 | 27.6 |
| Mean | SD | |
| Global Assessment Scale score | 32.2 | 11.1 |
| Hamilton Depression Rating Scaleb | 25.5 | 8.2 |
| Age (years) | 36.7 | 12.9 |
| Duration of follow-up (years) | 21.0 | 8.2 |
Antiepileptic Exposure
Propensity for Antiepileptic Exposure
| Variable | Odds Ratio | 95% CI | z | p |
|---|---|---|---|---|
| Hollingshead socioeconomic status scaleb | ||||
| I or II | 1.00 | |||
| III | 1.52 | 0.62–3.75 | 0.91 | 0.364 |
| IV | 0.64 | 0.23–1.79 | –0.85 | 0.394 |
| V | 0.36 | 0.13–1.02 | –1.92 | 0.055 |
| Marital status | ||||
| Married | 1.00 | |||
| Never married | 2.25 | 1.04–4.84 | 2.07 | 0.038 |
| Divorced, separated, or widowed | 0.97 | 0.44–2.14 | –0.08 | 0.934 |
| Site | ||||
| New York | 1.00 | |||
| St. Louis | 2.94 | 0.94–9.16 | 1.86 | 0.063 |
| Boston | 1.67 | 0.43–6.53 | 0.74 | 0.459 |
| Iowa City | 5.93 | 1.85–18.95 | 3.00 | 0.003 |
| Chicago | 3.28 | 1.08–9.97 | 2.10 | 0.036 |
| Gender | ||||
| Female | 1.00 | |||
| Male | 1.72 | 0.87–3.40 | 1.55 | 0.121 |
| Severity of mania | 3.83 | 2.39–6.14 | 5.59 | <0.001 |
| Severity of hypomania | 5.93 | 2.09–16.86 | 3.34 | 0.001 |
| Antipsychotics in week prior to exposure interval | 0.50 | 0.32–0.79 | –2.97 | 0.003 |
| Suicide attempt between intake and start of exposure interval | 1.66 | 0.93–2.95 | 1.71 | 0.086 |
| Age | 1.06 | 1.03–1.08 | 4.68 | <0.001 |
| Cumulative morbidity | 1.01 | 1.00–1.02 | 1.61 | 0.108 |
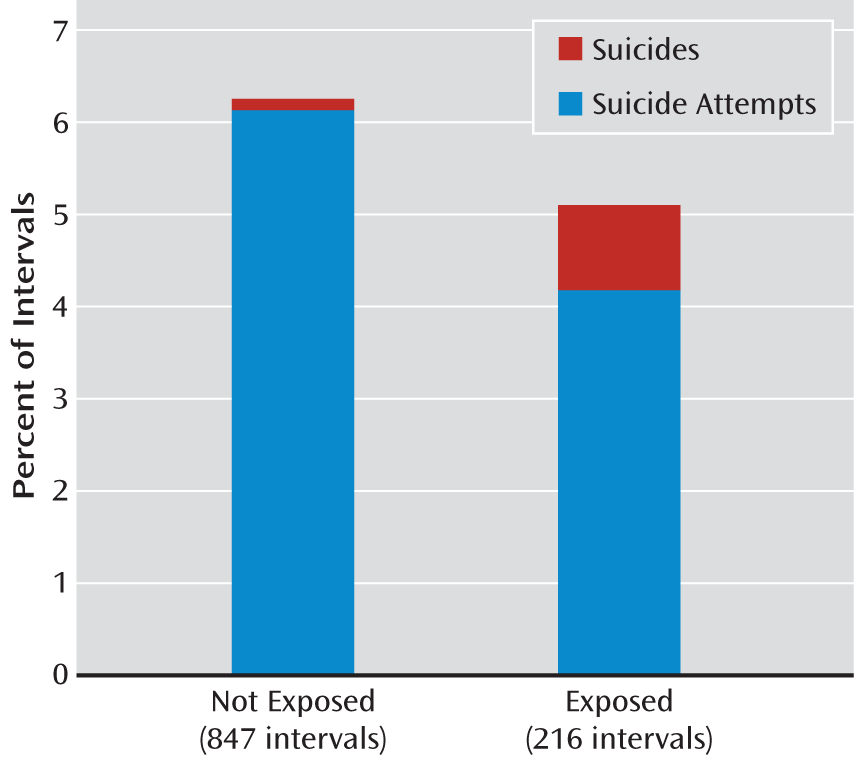
Primary Results: Safety Analyses
Discussion
Conclusions
Footnotes
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

