Few studies have examined the natural history of illicit drug use and drug use disorders in the U.S. general population, despite their being associated with extensive costs, harms, disability, and deaths (
1–
9). Although data on the prevalence of illicit drug use and disorders (
10) are critical to the allocation of health resources, cross-sectional prevalence data confound initial drug use with recurrent drug use and confound progression from use to problem use with chronic problems, leading to divergent characterizations of the course of drug use and drug use disorders (
10–
12). In light of recent evidence that different genetic factors may influence initiation of drug use and progression to dependence (
13), and in order to determine whether unique public health responses are required to address each of these processes, there is a need to elucidate risk factors specific to each or common across all. Because only a select minority of individuals with drug use disorders obtain drug treatment (
9,
10), it is critical to examine transitions within the general population.
Most epidemiologic studies of substance use initiation have focused on the high-risk period of adolescence (
14–
16). One recent study examining adults, based on the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), found that the odds of initiating illicit drug use over a 3-year follow-up interval were significantly higher among respondents with a history of childhood abuse; familial substance use problems; mood, personality, and alcohol use disorders; and nicotine dependence. The odds of initiating use were lower among women, Asians/Pacific Islanders, and Hispanics and greater among unmarried individuals (
17).
Data from the NESARC also have been used to study transition from first use to dependence for cannabis and cocaine (
18). For both drugs, the odds of progressing from use to dependence decreased with age, income, and education but were greater among those who were unmarried, initiated use before age 14, and had lifetime psychiatric and substance use disorders. For cannabis only, progression to dependence was more likely among men. Similarly, data from the National Comorbidity Survey (
19) showed that male cannabis users were more likely than female users to develop cannabis dependence shortly after initiation of use, whereas onset of cocaine dependence among cocaine users showed little variation by sex. Two additional NESARC-based studies showed that independent major depression was associated with a higher odds of relapse to cocaine dependence (
20) and that antisocial, borderline, and schizotypal personality disorders were associated with persistent cannabis abuse and dependence (
21).
Data from general population samples have shown varying correlates of drug use cessation and remission from drug use disorders. In a longitudinal community sample of lifetime marijuana users, cessation of use by ages 34–35 was negatively associated with male sex, use of other illicit drugs, and delinquency and positively associated with education, age at first use, presence of depressive symptoms, and getting married or becoming a parent for the first time (
22). In an analysis of NESARC respondents with prior lifetime cannabis and cocaine dependence (
23), the odds of having achieved remission during the year before the baseline interview were lower for men and those with other drug dependence and higher among those 18–29 years of age compared with those age 45 and older for both substances. For cannabis only, remission was positively associated with lifetime conduct disorder and negatively associated with personality disorder and alcohol dependence. For cocaine only, remission was positively associated with nicotine dependence and negatively associated with black race/ethnicity.
Inconsistent findings across past studies reflect not only their focus on different drug transitions, but also the effects of sample composition, study design, follow-up interval, and definition of drug use and problem use. Even among studies sharing a common sample (
17,
18,
20,
21,
23), comparisons may be confounded by the focus on different drugs, different potential correlates, and whether prospective or retrospective study designs were used. Standardizing these elements would reduce the “noise” confounding comparisons across studies.
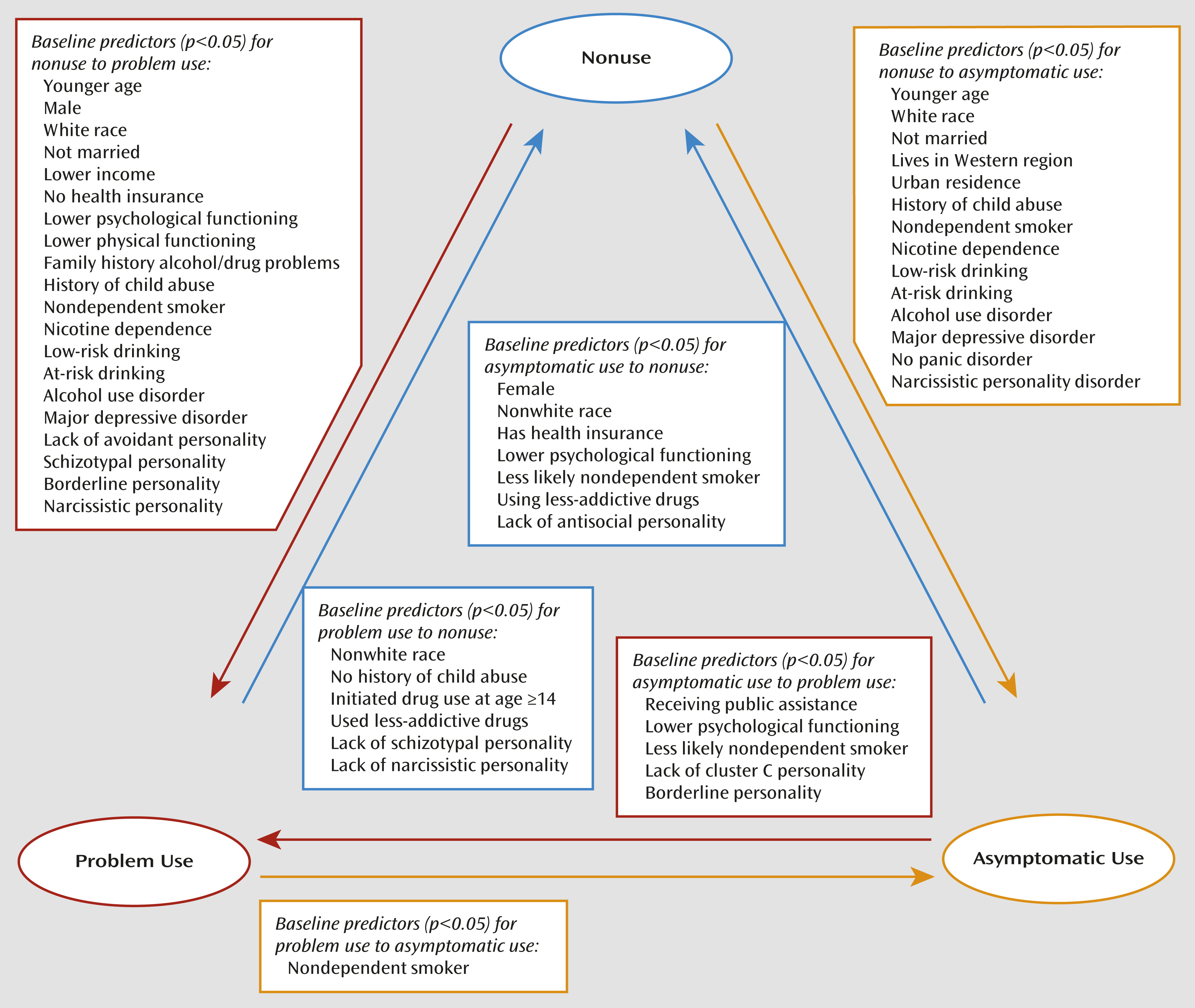
In this study, we prospectively examined a range of transitions in past-year drug status across the 3-year follow-up interval between two waves of a U.S. general population study, using a consistent set of potential correlates for all transitions and pooling 10 illicit drug categories in order to preclude identification of correlates relevant for only a single drug. Based on growing evidence that drug dependence may reflect an arbitrary cutpoint on an inherently dimensional scale of drug use problems (
6,
24–
26), as well as evidence from natural-history studies of common transitions among use, abuse, and dependence (
11), we distinguished problem use from asymptomatic use by the presence or absence of symptoms that operationalize the DSM-IV drug abuse and dependence criteria. Finally, we adopted a statistical modeling approach that evaluated risks for competing drug transitions, simultaneously identifying predictors of transitions to asymptomatic use and problem use among nonusers, predictors of progression to problem use and cessation of use among asymptomatic users, and predictors of transitions to asymptomatic use and nonuse among those who had problem use at baseline (
Figure 1). For all models, the referent group for transitions comprised individuals whose past-year drug status remained the same at waves 1 and 2.
Method
Sample
We used data from waves 1 and 2 of the NESARC. Only individuals who consented to participate after receiving written information about the nature of the survey, uses of the survey data, the voluntary nature of their participation, and the legally mandated confidentiality of identifiable survey information were interviewed. The research protocol received full ethical review and approval from the U.S. Census Bureau and the U.S. Office of Management and Budget. The nationally representative 2001–2002 wave 1 sample comprised 43,093 U.S. adults (age 18 and older) living in households and noninstitutional group quarters. The 2004–2005 wave 2 follow-up sample included 34,653 of the original respondents, 86.7% of those eligible for reinterview (cumulative response rate, 70.2%). Information on the sample design, field work, and weighting is available elsewhere (
5,
27,
28). This study is based on three subsamples of respondents: those who did not use any illicit drugs in the year preceding the wave 1 interview (N=32,675, including 5,740 former drug users), wave 1 past-year asymptomatic drug users (N=861), and individuals with wave 1 past-year problem use (N=1,117).
Measures
Drug use status and drug use transitions.
Past-year drug use was based on ten categories of drugs: sedatives, tranquilizers, opiates, and amphetamines when used without or beyond the limits of a prescription; cannabis; cocaine/crack; hallucinogens; solvents/inhalants; heroin; and other drugs. Problem use was defined as past-year occurrence of any of 40 symptoms (expanded to include two additional withdrawal symptoms in wave 2) operationalizing DSM-IV drug abuse and dependence criteria. Cross-tabulating wave 1 by wave 2 drug status (nonuse, asymptomatic use, problem use) yielded nine transition categories (
Figure 1).
Background and health covariates.
Standard background characteristics included wave 1 age, sex, race/ethnicity, marital status, educational attainment, family income, geographic region, urban/rural residence, receipt of public assistance, and health insurance coverage. Psychological and physical functioning were represented by the norm-based mental and physical component scales of the 12-Item Short-Form Health Survey (
29), rescaled to a U.S. general population mean of 50 and a standard deviation of 10. Number of life stressors was derived from a list of 12 past-year events. Familial substance use problems comprised respondent-reported alcohol or drug problems in any first- or second-degree relative. Childhood abuse comprised physical and/or sexual abuse before age 18.
Substance use and psychopathologic covariates.
Former drug use reflected use prior to, but not during, the year preceding the wave 1 interview. Tobacco use reflected five tobacco types and distinguished use with and without DSM-IV nicotine dependence (
30). Past-year alcohol use was divided into four categories: individuals with DSM-IV alcohol abuse or dependence (
31); risk drinkers who exceeded the National Institute on Alcohol Abuse and Alcoholism low-risk drinking guidelines of ≤14 drinks per week and ≤4 drinks on any day for men and ≤7 drinks per week and ≤3 drinks on any day for women (
http://rethinkingdrinking.niaaa.nih.gov/); low-risk drinkers who did not exceed these limits; and nondrinkers. Early drug use was defined as first use before age 14 (
32). Drug use typology distinguished less-addictive drugs (sedatives, tranquilizers, hallucinogens, and solvents/inhalants), more-addictive drugs (marijuana and opiates), and highly addictive drugs (amphetamines, cocaine/crack, and heroin), based on the proportion of past-year users with drug dependence (
33). Past-year mood, anxiety, and personality disorders were assessed in accordance with DSM-IV criteria. Their derivation, reliability, and validity are available elsewhere (kappa values, 0.40–0.74 for axis I disorders and 0.40–0.71 for axis II disorders) (
34–
36).
Analysis
Chi-square tests and analysis of variance were used to assess bivariate associations. Multivariate multinomial regression models yielded adjusted associations of the covariates with transition status. Separate analyses were conducted among wave 1 categories of nonuse (contrasting wave 2 asymptomatic use and problem use with continued nonuse), asymptomatic use (contrasting wave 2 nonuse and problem use with continued asymptomatic use), and problem use (contrasting wave 2 nonuse and asymptomatic use with continued problem use). Covariates were entered in four blocks (sociodemographic characteristics, health measures, substance use, and psychiatric disorders), each partially reduced before adding the next block. The models were ultimately reduced to retain only covariates with p values <0.05 for at least one of the two competing transition outcomes or whose presence was necessary to retain the proper referent category for multicategorical variables. Because of small cell sizes, we combined bipolar I and II disorders, panic with and without agoraphobia, and all nonwhite racial/ethnic groups. In the models based on wave 1 asymptomatic use, we additionally combined all mood disorders, all anxiety disorders, and all cluster C personality disorders. The SUDAAN statistical software package (
37) was used to obtain variance estimates that account for complex multistage sample designs.
Results
In the year preceding the wave 1 baseline interview, an estimated 93.9% of U.S. adults (∼195.0 million individuals) did not use illicit drugs (17.1% were former drug users and 76.8% were lifetime nonusers), 2.6% (∼5.4 million) were asymptomatic users, and 3.5% (∼7.5 million) had problem use (
Table 1). Among baseline nonusers, 95.4% were continued nonusers at wave 2, 2.1% became asymptomatic users, and 2.5% developed problem use. Among baseline asymptomatic users, 66.6% had stopped using drugs at wave 2, 14.3% continued to be asymptomatic users, and 19.1% developed problem use. Nearly half (49.0%) of those with baseline problem use had stopped using drugs at wave 2, 10.9% were asymptomatic users, and 40.1% continued to have problem use.
Among baseline nonusers (
Table 2), age, psychological functioning, and percentage married or cohabiting decreased steadily across wave 2 nonuse, asymptomatic use, problem use, whereas the proportion of males and the prevalence of familial substance-use problems, number of life stressors, and prevalence of childhood abuse increased. Individuals who were attending or had completed college were overrepresented among wave 2 asymptomatic users, whereas individuals who received public assistance payments or had no health care coverage were overrepresented in the problem use category. Transitions to asymptomatic use and problem use were strongly associated with other substance use and psychopathology. Severity of drug involvement was positively related to severity of tobacco and alcohol use, and prevalence of most mood and personality disorders increased steadily across wave 2 nonuse, asymptomatic use, and problem use.
Among individuals with baseline asymptomatic use and problem use (
Table 2), age and childhood abuse demonstrated the same patterns as they did among nonusers. Mean psychological functioning was highest and public assistance and public health insurance coverage least prevalent among those who remained asymptomatic users at wave 2. Transitions from asymptomatic use and problem use were less strongly associated with other substance use and psychopathology than were transitions from nonuse, but they were strongly associated with wave 1 drug use characteristics. Individuals who developed or continued to have problem use were the most likely (and those who ceased drug use the least likely) to have initiated drug use before age 14 and to have used highly addictive drugs. Schizotypal, borderline, narcissistic, and antisocial personality disorders were overrepresented among individuals who continued to have problem use; borderline and antisocial disorders also were overrepresented among those who transitioned from asymptomatic use to problem use.
Most bivariate correlates remained statistically significant when adjusted for other covariates (
Table 3 and
Figure 1). Transitions from nonuse to asymptomatic use were negatively related to age, nonwhite race/ethnicity, marriage/cohabitation, and panic disorder but positively associated with living in a Western state or an urban setting, childhood abuse, smoking and drinking (especially with use disorders), major depressive disorder, and narcissistic personality disorder. Transitions from nonuse to problem use were negatively related to age, nonwhite race/ethnicity, marriage/cohabitation, income, psychological and physical functioning, and avoidant personality disorder and positively associated with male sex, no health insurance, familial substance use problems, childhood abuse, smoking and drinking, major depressive disorder, and schizotypal, borderline, and narcissistic personality disorders. When a dummy variable for former drug use was added to the analytic model, none of the other odds ratios significantly changed in magnitude (data not shown); however, a few parameters of marginal statistical significance fell short of significance. Former drug use itself doubled the odds of transitions to both asymptomatic use and problem use.
Among baseline asymptomatic users, transitions to wave 2 nonuse were negatively associated with male sex, no health insurance, psychological functioning, nondependent smoking, use of more addictive drugs, and antisocial personality disorder and positively associated with nonwhite race/ethnicity. Transitions from asymptomatic use to problem use were negatively associated with psychological functioning, nondependent smoking, and cluster C personality disorders and positively associated with receipt of public assistance and a diagnosis of borderline personality disorder.
The transition from baseline problem use to nonuse occurred more frequently among nonwhites and less frequently among respondents who reported childhood abuse, initiated drug use before age 14, used more-addictive or highly addictive drugs (as opposed to less-addictive drugs), and met criteria for schizotypal or narcissistic personality disorder. The only significant correlate of transitioning from problem use to asymptomatic use was nondependent smoking.
Discussion
Transitions in drug status over a 3-year interval were associated with a wide range of factors, including sociodemographic and health characteristics, familial substance use problems, childhood abuse, tobacco and alcohol use, and psychopathology. For most of these, the association with progression from nonuse to asymptomatic use mirrored the association with progression from nonuse to problem use. Mood and anxiety disorders were associated with progression from nonuse to use (including problematic use), whereas factors related to poverty, health, family history, and personality disorders were significant only for transitions to and from problem use—that is, they appeared more strongly linked with persistent use than with casual, experimental use. Correlates of transitions to drug use were similar to those previously reported for first initiation of drug use (
17); however, the present study uniquely identified the specific mood, anxiety, and personality disorders underlying the broad associations previously reported and demonstrated the prognostic importance of alcohol and tobacco use even in the absence of alcohol and nicotine disorders.
Our findings regarding transitions
from asymptomatic use and problem use are difficult to compare with previous NESARC-based studies (
18,
23) because of differences in study design. Earlier studies used survival analyses of retrospective data to examine transitions over the life course, whereas we prospectively examined transitions over a 3-year follow-up period. Whereas previously identified correlates may reflect transitions occurring during adolescence, individuals in the present study were at least 18 years of age at baseline. Moreover, the previously identified protective effects of greater education and being married (for the risk of developing cannabis dependence) may reflect consequences of not developing dependence rather than direct preventive effects.
In the present study, the intensity of alcohol use had a linear association with transitions to drug use (including problem use) but no association with progression from use to problem use. Thus, the relationship with use may more strongly reflect common contextual correlates than common genetic liability. Similarly, nicotine dependence was associated with initiation of drug use but not with development of or remission from problem use. However, asymptomatic users who were nondependent smokers were less likely than nonsmokers to stop using drugs and less likely to have or develop problem use. Given problem use, they were at greater risk of reverting to asymptomatic use. Taken together, these results suggest the existence of a common resistance to nicotine dependence and symptomatic drug use, possibly reflecting similar delivery mechanisms for tobacco and cannabis, shared genetic liability or the lack thereof, or common effects on reward systems cross-sensitization (
38).
Extending prior studies of associations between any personality disorder and drug transitions, we found that these associations were driven by a handful of specific disorders. Consistent with two recent NESARC-based studies that examined the persistence of drug use disorder (
20,
21), we found that schizotypal and narcissistic personality disorders were negatively associated with drug use cessation among problem users; however, we did not replicate a similar effect of antisocial personality disorder that was reported in those studies. This discrepancy may reflect our adjustment for early drug use initiation, which may have mediated the effect of antisocial personality disorder. The negative associations of any cluster C personality disorder with transitioning from asymptomatic to problem use suggest that the fear and anxiety characteristic of this cluster may temper the intensity of drug use.
The positive association between major depressive disorder and initiation of use may reflect a form of self-medication, as suggested in a study of individuals with psychosis and substance use disorders (
39), whereas the negative association of panic disorder with initiation of use (significant only for panic with agoraphobia) could reflect discomfort with procuring illicit drugs.
This study did not replicate earlier findings of higher rates of drug use disorders among individuals with early-onset use (
32,
40), probably because individuals in this study were at least 18 years of age at baseline, by which time most disorders attributable to early use would already have occurred. However, the negative association between early-onset use and transitioning from problem use to nonuse suggests that the elevated prevalence of drug use disorders among early drug users reflects both increased onset and chronicity. Thus, these results support the importance of preventing early recreational drug use. Our finding of positive associations between social disadvantage and transition to problem use may reflect poverty-related exposure to illegal drug markets or lack of constraints that usually keep drug use within reasonable limits (e.g., job responsibilities) and are consistent with previously reported negative associations between income and the likelihood of developing cannabis and cocaine dependence (
18).
This study had a number of limitations that affect interpretation of its findings. By combining lifetime nonusers with former users, we may have failed to identify factors that differentially affect initiation and recurrence. However, controlling for former use had no meaningful impact on the other correlates of transitions from nonuse, and tests for effect modification revealed only a single, marginally significant (p=0.035) interaction of former drug use with other correlates, no more than would be expected by chance given the 34 correlates tested. Furthermore, by combining all illicit drugs, this study was unable to address variation by drug type, as has been suggested in past studies (
18,
23). Because cannabis was the drug most often used in this sample, correlates may apply to cannabis more than other drug-use transitions, and transitions for specific drugs will need further explication in other studies. Finally, this study focused on drug transitions during a relatively brief period, corresponding to ages well beyond peak drug use and drug use disorder for many respondents. Accordingly, the results of this study should be viewed as a complement to existing studies that have investigated transitions over the life course.
This study had a number of unique strengths. Its prospective design reduced the likelihood of false inferences regarding causality and ensured that associations with psychiatric disorders reflected those present at baseline and not those that may have developed after initiation of drug use or even after remission of problem use. Relative to survival models, which provide no information on individuals withdrawn from the risk of developing problem use (censored) because of drug use cessation, the models used in this study yielded correlates of drug use cessation that can inform efforts to prevent drug use and treat problem use. In addition, this study contrasted transitions to asymptomatic use and nonuse. Studies of remission from alcohol dependence (
41) have revealed distinct factors predicting abstinent and nonabstinent remission, a finding replicated in this study. Future studies might specifically address the impact of major life events, such as marrying and becoming a parent, which were significant predictors of nonabstinent remission from alcohol problems (
42) and marijuana use cessation (
22). In contrast to the similar rates of abstinent and nonabstinent remission reported for alcohol dependence (
41), this study found that problem users were more than four times as likely to transition to nonuse as to asymptomatic use. This finding, as well as the high ratio of problem users to asymptomatic users at baseline (i.e., a larger number of users with problems than of asymptomatic users), could reflect the low threshold of any drug use problems used in this study, or it may indicate that drug users are more susceptible to problems than alcohol users for reasons related either to their illegality or to unique physiological effects.
For clinicians, the importance of personality disorders in drug use transitions is clear, perhaps especially for borderline personality disorder, which was associated with the development of problem use. The demonstrated overlap of alcohol and tobacco use with illicit drug use underscores the value of addressing all substance use in patient assessments and treatment planning. Overall, these results support a view of illicit drug use trajectories as varied (
10,
11) rather than demonstrating a strict linear progression from nonuse to use to problem use requiring formal drug treatment. Among baseline asymptomatic users, two-thirds had ceased use in the year preceding the wave 2 follow-up interview, and only one-fifth had progressed to problem use. However, among baseline nonusers, more than half of those who had initiated use during the 3-year follow-up interval had already experienced problems. These findings speak to both the importance and the potential of early intervention (e.g., in routine medical and emergency care settings) for forestalling the development of drug use disorders in the general population.