Method
Sampling and Data Sources
Data were assembled to measure administrative, legal, and court-related costs of assisted outpatient treatment programs, inpatient and outpatient mental health services utilization, medical treatment, and criminal justice system involvement for 634 individuals who started an assisted outpatient treatment order within 30 days of discharge from an index hospitalization between January 2004 and December 2005. As mentioned above, the data were examined for the year before and 2 years following initiation of assisted outpatient treatment.
We examined one sample of assisted outpatient treatment participants in New York City and a second sample drawn from Albany, Erie, Monroe, Nassau, and Rensselaer counties (
14). Selection criteria were as follows: 1) an index hospitalization of any length between January 2004 and December 2005; 2) no assisted outpatient treatment order 12 months before discharge from the index hospitalization; and 3) an assisted outpatient treatment court order that went into effect no more than 30 days after discharge from the index hospitalization. The vast majority of assisted outpatient treatment orders originate around hospitalizations (
5). Any eligible persons who met these criteria were included, which produced a sample of 520 persons from New York City and 114 persons from the five counties, for a total of 20,003 person-month observations. The process of selection identified new court orders and represented approximately one-third of all active cases.
Data were collected from state psychiatric hospital admission files, the Tracking for Assisted Outpatient Treatment Cases and Treatments database, and Medicaid service claims. (The Medicaid cost analysis includes all Medicaid payments; thus, references to state costs should be understood to include the federal contribution to the state Medicaid program.) Participating Mental Hygiene Legal Service departments and individual assisted outpatient treatment programs provided budgetary information on program administrative, legal, and court-related costs associated with assisted outpatient treatment. Matching records of arrests and jail and prison stays were obtained from local sheriffs’ offices, the New York State Division of Criminal Justice Services, and the New York State Department of Corrections and Community Supervision.
Assisted outpatient treatment programs assist individuals in obtaining Medicaid, and the large majority of assisted outpatient treatment recipients (about 87%) are enrolled in Medicaid. All of the sampled participants in this study were Medicaid enrollees. Medicaid covers a wide range of services in New York State, including outpatient, partial, and inpatient care and pharmacy costs. Additional utilization and per diem cost information was obtained for inpatient psychiatric treatment at psychiatric hospitals licensed by the New York State Office of Mental Health.
To compare cost effects that may be associated with assisted outpatient treatment with those that may result from voluntary participation in intensive community-based mental health services, we also estimated the net effect of receiving assertive community treatment or intensive case management among individuals who did not qualify for assisted outpatient treatment and who resided in the same regions described above (N=255; 14,182 person-month observations). In this analysis, we used equivalent data (i.e., received assertive community treatment or intensive case management within the first 30 days after discharge from an index hospitalization and no assertive community treatment or intensive case management in the 12 months before the index hospitalization) for persons who did not receive assisted outpatient treatment orders but otherwise had the same psychiatric diagnoses and were in the same systems of care during the same years as the two assisted outpatient treatment samples.
This project was approved by the institutional review boards of Duke University Medical Center, Policy Research Associates, the New York State Office of Mental Health, and the Biomedical Research Alliance of New York.
Measures
Assisted outpatient treatment program costs for New York City and the five counties were obtained from program administrators. The average cost per case of assisted outpatient treatment was calculated from each program’s assisted outpatient treatment budget, reported expenditures on cases, and the number of participants served. The case-rate administrative expense was prorated to an average monthly charge for months when assisted outpatient treatment was active. A similar approach was used to calculate Mental Hygiene Legal Service and court costs, which were prorated across active assisted outpatient treatment months. Mental Hygiene Legal Service costs for activities not associated with assisted outpatient treatment, such as involuntary inpatient proceedings or litigation, were excluded.
Mental health services costs were obtained for the following categories: New York State Office of Mental Health facility hospitalization; Medicaid-paid hospitalization; psychiatric emergency department visits or crisis services; outpatient programs including assertive community treatment and continuing day treatment; case management (including intensive, blended, and supportive types); outpatient prescription medication; clinician visits (including billed encounters with psychiatrists, psychologists, and clinical social workers); chemical dependency treatment; transportation to treatment; and partial hospitalization. Except for hospitalization in New York State Office of Mental Health facilities, costs for mental health treatment were paid by Medicaid. Costs for New York State Office of Mental Health hospitalization stays were calculated as the product of the length of stay and the state average cost per bed day. Hospitalizations paid by private insurance were uncommon and were not included in these analyses. Other medical costs covered by Medicaid were included for nonpsychiatric hospitalizations, emergency department visits, outpatient treatment visits, and outpatient prescription medications.
Criminal justice cost information was obtained for arrests and jail and prison days. Arrest costs were based on inflation-adjusted published estimates described by Clark et al. (
15). These estimates included costs for police, booking, court, attorney services, and transportation. Jail costs per day were obtained from individual county jail cost of operation worksheets, which are completed by jails on an annual basis and submitted to the state. All completed worksheets were for the fiscal year 2008–2009. We also included costs for medications prescribed in jail. This cost information was obtained from interviews with key jail personnel. Prison costs per day were based on information obtained from the chief fiscal officer of the New York State Department of Corrections and Community Supervision for the fiscal year 2005–2006.
Current legal status was obtained from the New York State Office of Mental Health Tracking for Assisted Outpatient Treatment Cases and Treatments database. Start and end dates for court-ordered treatment were used to classify each month as being before, during, or after assisted outpatient treatment. This classification was used in a person-month regression analysis to estimate the adjusted effect of assisted outpatient treatment status on total cost. In addition, a person-level analysis was conducted to summarize and compare utilization and costs for the 12-month period before assisted outpatient treatment began with the subsequent two 12-month periods after treatment began.
Medication possession ratio, a commonly used proxy for medication adherence, was constructed using Medicaid pharmacy fill records (
13–
18). We calculated the number of days in a given month in which an individual had a supply of a prescribed psychotropic medication that was clinically appropriate for his or her current diagnosis, as determined by a psychiatrist blind to participants’ identity. Consistent with previous research, the months in which the filled supply of medication was enough to cover 80% of days were considered high-possession months, compared with low-possession months when the filled supply covered less than 80% of days. (Depot injectable medication claims were coded as a complete fill for the given month.)
Data on race/ethnicity, sex, and age were obtained from the New York State Office of Mental Health. In the regression analysis, participants of Hispanic ethnicity and African Americans, Asians, and persons from other racial/ethnic backgrounds were compared with non-Hispanic whites. Men were compared with women, and individuals older than the median age were compared with those younger than the median age.
Psychiatric diagnosis and information on monthly receipt of assertive community treatment and intensive case management were obtained from Medicaid claims. Primary diagnoses were obtained from these claims and grouped into four categories: schizophrenia spectrum disorder, bipolar disorder, major depressive disorder, and other. We counted the number of claims with each diagnosis; the most frequent diagnosis type over the study period was then used to classify the participant. For the five-county analysis, costs for persons residing in Albany, Erie, Monroe, and Rensselaer counties were compared with costs for persons residing in Nassau County as the reference category.
Data Analysis
We first calculated rates of services utilization and the mean cost per person for each type of service used in three time periods: 1) the 12 months before discharge from the index hospitalization when assisted outpatient treatment was initiated; 2) the first 12 months after discharge from the index hospitalization; and 3) the second 12 months (i.e., the period from 13 to 24 months after discharge from the index hospitalization). Because assisted outpatient treatment orders varied in length, these subsequent 12-month periods represented costs incurred after assisted outpatient treatment was initiated, whether or not an assisted outpatient treatment order remained in place; this resembles an intent-to-treat analysis. Mean costs are presented in two ways: first as the average cost among those using the service (i.e., with nonusers removed from the denominator) and second as the average cost per person in assisted outpatient treatment (i.e., with all sample participants in the denominator.)
We also conducted a longitudinal multivariate regression analysis to assess the adjusted effect of assisted outpatient treatment status on total and mental health costs. The unit of analysis for these regression models was the person-month, reflecting multiple repeated observations for each participant. Assisted outpatient treatment status was coded as a time-varying descriptor for each monthly observation in the analysis. Monthly costs were regressed on dummy variables associated with monthly assisted outpatient treatment status (i.e., current or postassisted outpatient treatment compared with pre-assisted outpatient treatment).
A negative binomial model was estimated to accommodate dispersion in the cost data (
19). We examined the negative binomial dispersion parameter to confirm that the negative binomial model was a better-fitting model than the Poisson model. We estimated robust standard errors to account for the nonindependence of observations. All analyses were conducted with SAS, version 9.2 (SAS Institute, Cary, N.C.). Separate analyses were conducted for samples from New York City and the five counties for both the assisted outpatient treatment group and the samples of individuals who did not qualify for assisted outpatient treatment. To examine the effect of missing data, we used several approaches to impute missing data and found that no approach appreciably affected the cost estimates.
Results
The demographic and clinical characteristics of the two samples are summarized in
Table 1. The mean age of participants was 40 years in the New York City sample and 42 years in the five-county sample. The majority of participants in both samples were men. Substantially more of the participants in the New York City sample were African American compared with the five-county sample. Four-fifths of those in the New York City sample (82%) and three-fourths of those in the five-county sample (75%) had a diagnosis of a schizophrenia spectrum disorder. More than one-third of the five-county sample resided in Nassau County; the remainder of these participants were distributed fairly evenly among the other four counties.
The average rates of services utilization per person for the three 12-month periods, by sample, are presented in
Table 2. For each category of service, we report the number and percent of the sample with any utilization during the period (i.e., at least one Medicaid claim for the type of service listed, at least one hospital admission in the case of New York State Office of Mental Health inpatient treatment, or at least one arrest, jail day, or prison day in the case of criminal justice involvement).
The main finding is that hospitalization declined markedly during the first 12 months after assisted outpatient treatment was initiated, while increases were seen in utilization of case management, assertive community treatment, other outpatient services, and psychotropic medication fills. In the second 12-month period, additional modest declines were observed for hospitalization rates, while case management and outpatient program participation also declined but remained above preassisted outpatient treatment levels. Declines were also seen in use of psychiatric emergency and crisis services, clinician visits, and criminal justice involvement. It is notable that, for the most part, increases in outpatient utilization rates were sustained into the third 12-month period of observation, during which many assisted outpatient treatment participants were no longer subject to court-ordered treatment. These observed patterns were similar in both the New York City and five-county samples.
The summary costs per person with any utilization in each category for the three periods, by sample, are presented in
Table 3. In the New York City sample, the average annual cost of New York State Office of Mental Health inpatient treatment per person hospitalized declined from about $142,000 to about $84,000 from the preassisted outpatient treatment period to the first 12 months after assisted outpatient treatment was initiated, and then it increased to about $119,000 per person hospitalized in the second 12 months after assisted outpatient treatment. A similar pattern was observed among New York State Office of Mental Health-hospitalized participants in the five-county sample, except the second year trend reversal was proportionally smaller than it was in the New York City sample.
Considering Medicaid-paid hospitalization, consistent declines in cost per person hospitalized were seen in both periods following initiation of assisted outpatient treatment, and in both samples, but with a proportionately greater second-year decline in the five-county sample. In the New York City sample, Medicaid inpatient costs declined from about $66,000 to about $46,000 per person hospitalized (i.e., comparing the year before assisted outpatient treatment began to the second year after assisted outpatient treatment was initiated). In the five-county sample, a comparable total decline was observed, from about $47,000 to about $18,000 annually per person hospitalized.
These patterns are consistent with a pattern of fewer hospitalizations per person, reduced length of stay, or both, moving from before to after initiation of assisted outpatient treatment. At the same time, while hospitalization costs declined, average annual costs for outpatient (or noninpatient) treatment increased, from about $6,000 per person served in the year before assisted outpatient treatment to about $14,000–$18,000 per person served after assisted outpatient treatment years began.
Overall, cost trends in the five-county sample resembled those observed in the New York City sample, with a few notable differences. The baseline annual cost per person served for all Medicaid-paid services was higher in the New York City sample, with about $60,000 per person served, compared with about $47,000 per person served in the five-county sample. However, both samples exhibited comparable proportional declines in per-person Medicaid costs across the three periods of observation: a 40% decline in the New York City sample and a 48% decline in the five-county sample from the year before initiation of assisted outpatient treatment to the second 12-month period after initiation of assisted outpatient treatment.
Average annual criminal justice costs (per person with any arrests or jail or prison days) revealed no clear pattern but mostly increased in both samples across the three periods. Thus, while there were fewer individuals involved with the criminal justice system during the periods after assisted outpatient treatment was initiated (as shown in
Table 2), those who were arrested or spent time incarcerated incurred approximately the same or higher costs over the three study periods.
In summary, combining all costs, the average annual cost per person declined substantially and consistently across the three periods of observation, in both samples. In the New York City sample, average costs declined 50%, from about $105,000 to about $53,000 per person, and in the five-county sample, average costs declined 62%, from about $104,000 to about $39,000 per person. Most of the decline was seen in the first year after assisted outpatient treatment was initiated, with a larger incremental second-year decline in the five-county sample than in the New York City sample.
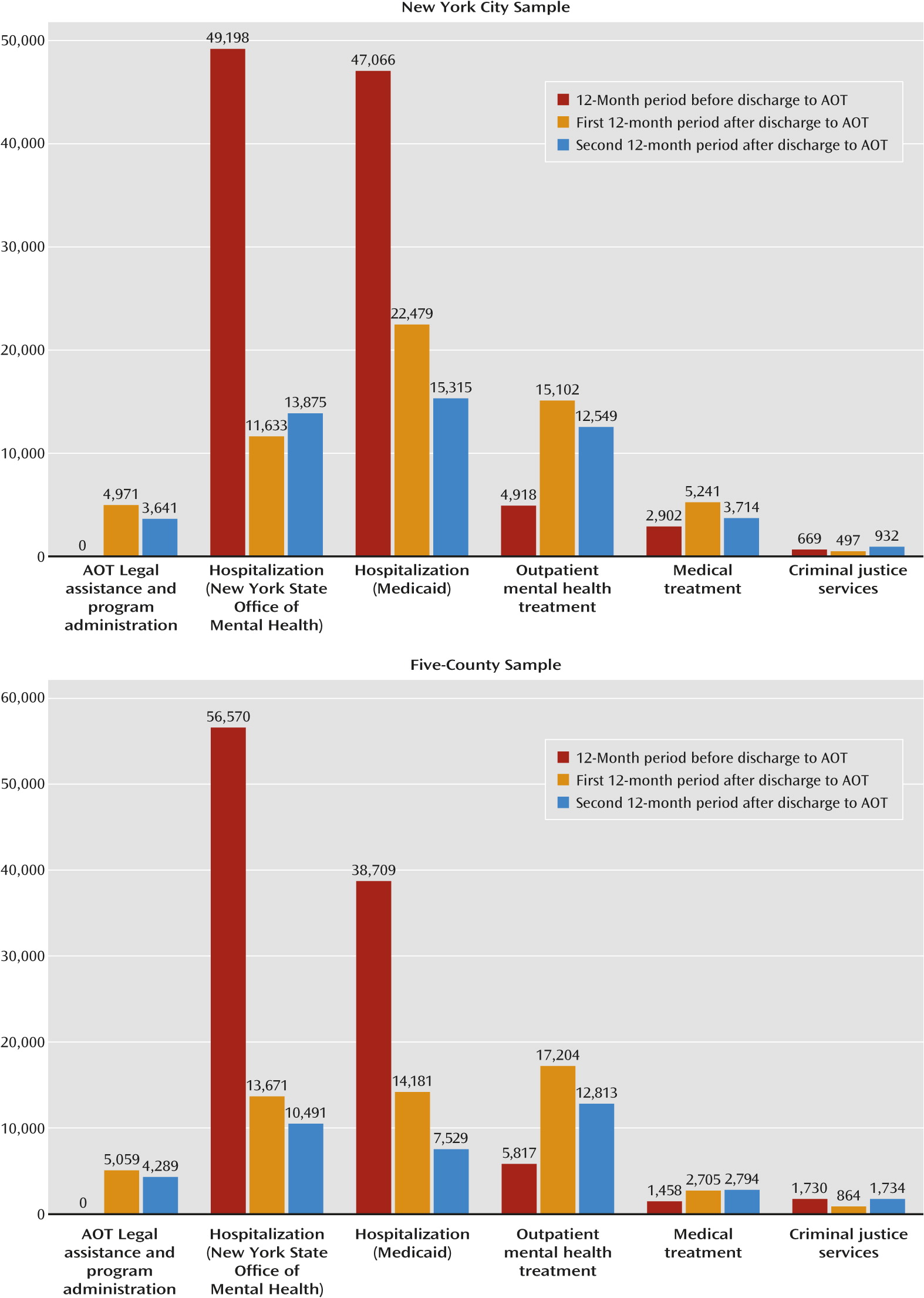
Costs by period and sample are presented in
Figure 1, in which the total assisted outpatient treatment sample is used as the denominator (in contrast to the average costs presented in
Table 3); this way of presenting the data spreads the costs across the entire assisted outpatient treatment group rather than only among those utilizing a particular service. In summary, both samples exhibited substantial shifts in service costs, apparently driven by an increase in outpatient treatment costs and a corresponding decrease in psychiatric hospitalization costs. The legal and administrative costs of the assisted outpatient treatment program were small in comparison to the large costs, and apparent shifts in cost, associated with inpatient and outpatient mental health services utilization.
Finally, results of longitudinal multivariate regression analyses conducted to assess net effects of assisted outpatient treatment participation on service costs over time, controlling for demographic and clinical covariates, are presented in
Table 4. Assisted outpatient treatment cost effects are presented in comparison to the analogous effects of voluntary participation in intensive community-based services (assertive community treatment or intensive case management) for the samples of persons with serious mental illness who did not qualify for assisted outpatient treatment in New York City and in the five counties. In these voluntary outpatient treatment comparison groups, average per-person costs for the New York City and five-county samples were $7,056 and $4,420, respectively, in the preintensive service 12-month period, and they declined to $4,549 and $3,457, respectively, in the first year and to $3,764 and $3,379, respectively, in the second year.
Significant cost-reducing effects associated with assisted outpatient treatment were found for mental health treatment costs and total state costs in both the New York City and five-county samples. Medication adherence also was associated independently with lower service costs in these samples. Regression analyses for the voluntary treatment sample from New York City revealed significant declines in costs associated with voluntary participation in intensive services, although these declines were smaller and of less significance, about half as large as the declines related to assisted outpatient treatment. In the five-county analyses, in contrast to assisted outpatient treatment, voluntary participation in intensive services was not significantly associated with declines in mental health costs or total state costs.
Discussion
Assisted outpatient treatment remains controversial despite evidence of its effectiveness. Forty-five states now permit outpatient commitment in some form, yet the practice has been implemented only sporadically, if at all (
20). Several factors may explain the low penetration of assisted outpatient treatment (
7,
21–
23). Vocal mental health consumer advocates oppose it, and some mental health clinicians and administrators raise liability and operational concerns. Furthermore, some view outpatient commitment as diverting resources from voluntary service recipients, a claim that might be refuted if assisted outpatient treatment reduces overall treatment costs (
24–
26).
The question of cost comes into play in policy arguments for and against assisted outpatient treatment. If assisted outpatient treatment is a net drain on resources or precipitates “queue jumping” in a zero-sum game for public resources, then it may be difficult to justify this type of program even if it “works” for a small number of people. However, if assisted outpatient treatment offsets other medical costs, such as reducing hospitalizations for state-supported clients, then policy makers may be on firmer ground in arguing in favor of funding it. In the end, assisted outpatient treatment may benefit not only the people who receive court-ordered treatment but also those who will be served in a more efficient public behavioral health care system, a system with greater capacity that produces better outcomes for a broader population in need (
27).
Our analyses for New York State suggest that assisted outpatient treatment reduces total state costs for those it serves, mainly by shifting patterns of service provision from repeated inpatient episodes to regular outpatient care and improved receipt of appropriate psychotropic medications. In the New York City sample, total combined costs for the assisted outpatient treatment program, mental health and medical treatment, and criminal justice services declined 43% in the first year after assisted outpatient treatment began and an additional 13% in the second year. In the five-county sample, these declines were even greater: 49% in the first year after treatment initiation and an additional 27% in the second year. However, these results from New York may not generalize to other states, where this type of program may operate differently and where the public system may be less generously funded; even in New York, the gains may not be sustainable if treatment resources are substantially reduced. Our analyses estimate net treatment and programmatic costs, and we did not attempt to estimate a host of other costs and savings that may result from reduced family or caregiver burden or other costs to society.
Parallel analyses for a sample of voluntary participants in intensive community-based services produced mixed results. In the New York City comparison sample, voluntary participation in assertive community treatment or intensive case management was associated with significant net declines in mental health service costs and total state costs, although the relative declines were not as dramatic as the declines related to assisted outpatient treatment. However, in the five-county comparison sample, no significant declines in costs were associated with voluntary community-based service participation.
The nonrandomized comparison of assisted outpatient treatment with voluntary treatment effects is limited; the fact that one group qualified for assisted outpatient treatment and the other group did not means that the groups differed in ways that could not be observed and controlled for. However, the before-and-after adjusted time-series comparison for the assisted outpatient treatment group is a quasi-experimental design capable of accounting for time-invariant differences across groups. Furthermore, our comparison uses the large number of person-period observations that are available for the periods before, as well as during and after, assisted outpatient treatment. Because of this relatively long period of observation before the start of the court-ordered treatment, these results are unlikely to be a result of regression to the mean, and because the program has been in place for several years, these results are also unlikely to be a transient response to programmatic change.
In short, these cost estimates provide crucial information to help public policy makers decide whether assisted outpatient treatment is warranted from both fiscal and clinical perspectives. Results of this study reveal significantly reduced overall costs under New York’s assisted outpatient treatment program, attributable mainly to a marked shift in patterns of mental health services provision from inpatient to outpatient care settings. For a large proportion of baseline services, costs were associated with lengthy hospitalizations preceding assisted outpatient treatment, which suggests that averting extended inpatient treatment could yield significant savings. However, while assisted outpatient treatment programs typically start after inpatient admissions, this is not a program requirement. Assisted outpatient treatment programs that are not preceded by a hospitalization may not result in as significant a savings. Finally, for persons with serious mental illnesses who do not legally qualify for assisted outpatient treatment, voluntary participation in intensive community-based services may also reduce overall service costs over time, at least in a population and mental health system resembling that of New York City.