The ability to quickly anticipate, respond to, and recover from recurrent stressors is fundamental to a healthy homeostatic system and essential for long-term behavioral and psychological health. In particular, stress recovery is critical to the optimal functioning of military personnel during deployment and integral to their postdeployment reintegration. Population-based studies of military personnel serving in combat indicate prevalences of stress-related mental health disorders between 11.3% and 19.1% (
1). Military operations in Iraq and Afghanistan now span a decade, marking America’s longest sustained combat operations. Studies of trauma-related pathology and resilience highlight the fact that while intense stress chronically perturbs homeostatic mechanisms for some individuals, others are able to recover (
2–
4). Available neuroscientific evidence suggests that maladaptation to stress is associated with disruption of neural networks that communicate and integrate information about the response to stress (
5). However, our understanding of these mechanisms is incomplete, and a translational knowledge gap remains regarding whether brain-behavior relationships can be reliably modified prior to stressful experiences in a way that confers an enhanced ability to recover.
Successful recovery from stress is multifaceted, with complex interactions between brain, behavior, and environment. The brain is the central organ of stress response and recovery, and essential to these processes is an individual’s awareness of his or her internal physiological state, also known as interoception (
6,
7). Interoception, which is functionally and neuroanatomically distinct from the traditional “five senses” (
8), is a process through which the brain monitors and updates the body about its overall physical state, including its ability to recognize bodily sensations, be aware of emotional states, and maintain physiologic homeostasis.
Inefficient interoceptive function has been shown to play a critical role in the development of mood and anxiety disorders (
9–
12). Conversely, interoceptive exposure, the intentional induction of symptoms of sympathetic arousal, has been shown to be effective in treating anxiety disorders (
13), panic disorder (
14,
15), posttraumatic stress disorder (
16), chronic pain (
17), and irritable bowel syndrome (
18,
19).
Functional neuroimaging studies have identified the insular cortex as a critical brain structure for modulating interoceptive function (
20,
21). A series of neuroimaging studies by our group has shown that altered insula activation differentiates individuals known to perform well under severe stress (e.g., “exceptional performers”) from healthy control subjects (
22–
25). In other words, more efficient functioning in the insular cortex and enhanced interoceptive processing distinguishes those who perform well under high-magnitude stress from those who do not.
Growing evidence suggests that deliberate modification of interoceptive function can be achieved through mindfulness training (MT). Mindfulness is a mental mode characterized by full attention to present-moment experience without elaboration, judgment, or emotional reactivity. It includes the ability to pay attention to, describe, and act with full awareness of sensations, perceptions, thoughts, and emotions (
26). MT programs that offer exercises and didactic instruction to help participants cultivate this mental mode.
Modification of insula activation has been reported in experienced practitioners of meditation compared with nonpractitioners (
27), as well as in healthy participants in an 8-week MT course compared with control subjects (
28,
29). Other studies have shown that MT practice corresponds to “more efficient” functional activity profiles within prefrontal regions during attention-demanding tasks (
30). These results suggest that alteration of insula function may be associated with mindfulness-based improvements in the capacity to appraise emotion as “innocuous sensory information rather than as affect-laden threat to self requiring a regulatory response” (
29, p. 31).
Our primary aim in this study was to examine the capacity of a mindfulness-based intervention called Mindfulness-Based Mind Fitness Training (MMFT) (
31) to modulate mechanisms underlying recovery from stress in active-duty military personnel prior to deployment. We obtained evidence in multiple domains (physiological measures, biomarkers, fMRI, and self-report clinical measures), consistent with the multiple levels of investigation mandated by the Research Domain Criteria, to further elucidate the capacity for MT to modulate brain-behavior mechanisms involved in recovery from stress. We hypothesized that an MT program emphasizing interoceptive awareness, as MMFT does, could create desirable changes across several functional domains implicated in response to, and recovery from, stressful training.
Method
Study Participants
We conducted this study during the summer of 2011 at Marine Corps Base Camp Pendleton, Calif., and at the University of California, San Diego (UCSD) Center for Functional MRI. The institutional review boards of the Naval Health Research Center and UCSD approved the study protocol. Participants were recruited from a convenience sample of two Marine infantry battalions scheduled to undergo predeployment training. Within those battalions, eight platoons (N=287) were randomly selected for study assignment; four platoons were assigned to the MT group (N=153) and four to a training-as-usual control condition (N=134). Five Marines from each of the eight platoons (N=40) comprised the functional MRI (fMRI) subsample.
Study Design
Written informed consent was obtained from all participants prior to the baseline assessment. Additional written consent for the subsample of participants undergoing fMRI was obtained prior to the baseline scan. Participants were assigned a unique study participant identification number for use throughout the study. A second assessment was conducted 8 weeks after baseline, and a third assessment was conducted 5–10 days after that (at approximately 9 weeks), at the Infantry Immersion Trainer (IIT) facility, during and after stressful combat training. Participants in the fMRI subsample underwent a second scan within 2 weeks of completing training exercises at the IIT facility (at approximately 10 weeks).
IIT facility.
The primary platform for evaluating recovery from stress was the IIT facility. Marine units preparing for deployment spend 1 day training at this facility as part of the standard predeployment training cycle. The IIT facility is a 32,000 square-foot compound located at Camp Pendleton. It comprises several one- and two-story huts, a religious center, a marketplace, and numerous walls, gates, and alleyways modeled on those typically found in a rural Middle East village. The IIT facility exposes Marines to close-quarters combat scenarios with the aid of foreign-national role players and realistic sensory (e.g., smells, sounds) and environmental (e.g., interpreters, pyrotechnics) stimuli. Real-time scenarios include a variety of operational challenges that vary in intensity and duration. For the present study, participants were exposed to three specified scenarios, each increasing in complexity. The first scenario involved a passive village patrol; the second focused on meeting village leadership (“a key leader engagement”); and the third required responding to a complex ambush.
MT Intervention
MMFT is a 20-hour course taught over 8 weeks, including eight 2-hour sessions of classroom instruction, an individual practice interview in week 3, and a 4-hour workshop with a longer session of silent practice to refine mindfulness skills in week 6. Outside of class sessions, participants are asked to complete at least 30 minutes of daily mindfulness and self-regulation exercises, divided into several practice periods each day. MMFT provides a novel approach to MT designed for individuals with prior exposure to prolonged significant stress. The program emphasizes interoceptive awareness by cultivating attentional control and tolerance for challenging experience, both external (i.e., harsh environmental conditions) and internal (e.g., physical pain, intense emotions, distressing thoughts). It also focuses on enhancing stress resilience, with didactic content and concrete skills for supporting self-regulation of the stress response and its effects. These skills and information incorporate and extend concepts from sensorimotor psychotherapy and somatic experiencing, and they inform the model of resilience taught in MMFT. The program was designed for the high-stress organizational context, with ways to integrate practices into the work setting, and with didactic content focused on the relationship between mindfulness, military stress inoculation, and complex decision making.
Measures
The primary physiological measures were heart rate and breathing rate. These were measured at the IIT facility and included continuous monitoring through the following sequence of periods: rest (45 minutes), anticipatory (10 minutes), stress (30 minutes), recovery (10 minutes), and rest (45 minutes). The primary biomarkers of interest were plasma concentrations of neuropeptide Y and norepinephrine. Neuropeptide Y is co-released with norepinephrine and at low concentrations is a secondary indicator of sympathetic activation. It is also released at high concentrations during intense or prolonged sympathetic activation and is a well-known stress modulator (
32).
For the fMRI component of the study, an emotion face processing task (
33) was used to assess quantitatively the functional status of the neural circuitry that has been implicated in emotion processing and interoception. This task examines brain activation when individuals process emotional faces when compared with simple geometric shapes and reliably produces insula activation. Previous studies of exceptional performers have shown altered activation patterns in this circuitry consistent with more efficient interoceptive processing (
22,
25). Behavioral characteristics of resilience were assessed with the Response to Stressful Experiences Scale, a self-report measure that was developed and validated in a large active-duty military and veteran sample (
34).
Procedures
Physiological monitoring (heart rate and breathing rate), blood draw, and self-report measures (including the Response to Stressful Experiences Scale) were completed at baseline, at 8 weeks, and during and after the stressful IIT session at approximately 9 weeks. A mobile lab was established at the study site, and samples were spun in a refrigerated centrifuge within 20 minutes of being drawn. Plasma was aliquotted and immediately placed on dry ice until transfer to a −80 freezer at the end of the training day. A subset of participants (N=40) underwent fMRI scanning at baseline and again within 2 weeks after the stressful IIT session, at approximately 10 weeks.
Analysis
Groups were contrasted on demographic variables. The interaction of group and time was analyzed for physiological, neuroendocrine, fMRI, and self-report data. The threshold for statistical significance was set at 0.05, with adjustments made for multiple comparisons. Main effects and interactions were analyzed using a general linear model for repeated measures and mixed-factorial designs. Brain imaging was analyzed using the AFNI software package (
http://afni.nimh.nih.gov/afni/). fMRI is predicated on cerebral blood flow and hemodynamic properties of deoxygenated hemoglobin, known as the blood-oxygen-level-dependent signal (
35). Based on our own and other studies with elite performers and anxious individuals and on pharmacological studies, we used a priori brain regions of interest (i.e., entire regions of the insula, the dorsal anterior cingulate cortex, and the medial prefrontal cortex) and restricted our analyses to those regions. Robust (Huber) regression analyses were performed between fMRI data and key variables to establish relationships between changes in brain activation patterns and neuroendocrine and physiological variables.
Results
Participant Flow
U.S. Marine Corps predeployment training requirements are intensive, and Marines’ training schedules are generally full and complex, and as a result, not all participants were able to attend each of the assessments. The scheduling conflicts cited below were related to training schedules, medical appointments, and temporary assigned duty to other locations. In addition, a few Marines declined the blood draw or the questionnaire containing the Pittsburgh Sleep Quality Index and the Response to Stressful Experiences Scale. The participant flow through the study is summarized below, as well in Figure S1 in the
data supplement that accompanies the online edition of this article.
MT group.
From the four platoons assigned to the MT group (N=153), 151 Marines were present at the baseline assessment (two had scheduling conflicts). Of these, four declined questionnaires and nine declined blood draw. Because of time constraints, 22 Marines in the MT group were unable to participate in the heart and breathing rate assessments. A total of 147 Marines consented to participate in the MT intervention, and all of them completed the intervention.
At the 8-week assessment, 134 Marines in the MT intervention group were present (13 had scheduling conflicts). Of these, 10 declined blood draw and eight were unable to participate in the heart and breathing rate assessments because of time constraints. For eight Marines, questionnaire data were lost by unintentional overwriting.
At the IIT assessment, 118 of the 147 Marines in the MT intervention group were present (29 had scheduling conflicts). Of these, three declined questionnaires and 10 declined blood draw. During the IIT session, heart and breathing rate data could be collected for only 54 Marines in the MT group because of the time constraints of the training and the time required to download data from sensors and transfer the monitoring harnesses to Marines in the next training group.
Control group.
From the four platoons assigned to the control group (N=134), 113 Marines were present at the baseline assessment (21 had scheduling conflicts). Of these, four declined questionnaires, six declined blood draw, and 22 were unable to participate in heart and breathing rate assessments because of time constraints.
At the 8-week assessment, 121 Marines from the control group were present (13 had scheduling conflicts). Of these, two declined blood draw, and 12 were unable to participate in the heart and breathing rate assessments because of time constraints.
At the IIT assessment, 95 of the 134 Marines in the control group were present (39 had scheduling conflicts). Of these, three declined blood draw. During the IIT session, heart and breathing rate data could be collected for only 53 Marines in the control group because of competing demands of training and time required to download data and transfer harnesses.
fMRI subgroup.
A total of 40 Marines—20 from the MT group and 20 from the control group (five from each of the eight platoons)—were randomly selected for fMRI assessments. All 40 Marines in the fMRI subgroup underwent scanning at baseline. At the follow-up fMRI assessment at approximately 10 weeks, one Marine from the control group was absent because of a scheduling conflict.
Sample Characteristics
The baseline characteristics of study participants are summarized in
Table 1. The MT and control groups did not differ significantly in age, duration of military service, race, education, height, or weight. The MT group had a smaller proportion of Marines who were married. Physical fitness did not differ significantly between the groups, except that the MT group had a slightly faster 3-mile run time. There were no differences between the groups regarding military operational specialty, number of combat deployments, combat exposure, or proportion taking prescribed medication. Self-report of resilience characteristics (based on the Response to Stressful Experiences Scale) did not differ between the groups at baseline. In both the overall study sample and the fMRI subsample, Marines in the MT group reported significantly worse quality of sleep at baseline compared with those in the control group. The fMRI subsample did not differ from the larger sample in age, duration of military service, combat exposure, height, weight, or physical fitness.
MT Intervention
Attendance was recorded for each platoon at each of the eight MT classroom sessions and the 4-hour workshop. The mean attendance rate for all sessions was 92.6% (SD=8.1, range=68−100). The mean practice time in excess of the 20 hours of classroom instruction was 205.1 minutes (SD=243.5, range=0–1750). Attendance rate and practice time did not differ significantly between platoons.
Stress Exposure
IIT scenario duration did not differ significantly between groups; the mean duration was 30.9 minutes (SD=10.3) for the MT group and 29.2 minutes (SD=11.1) for the control group.
Autonomic Physiology
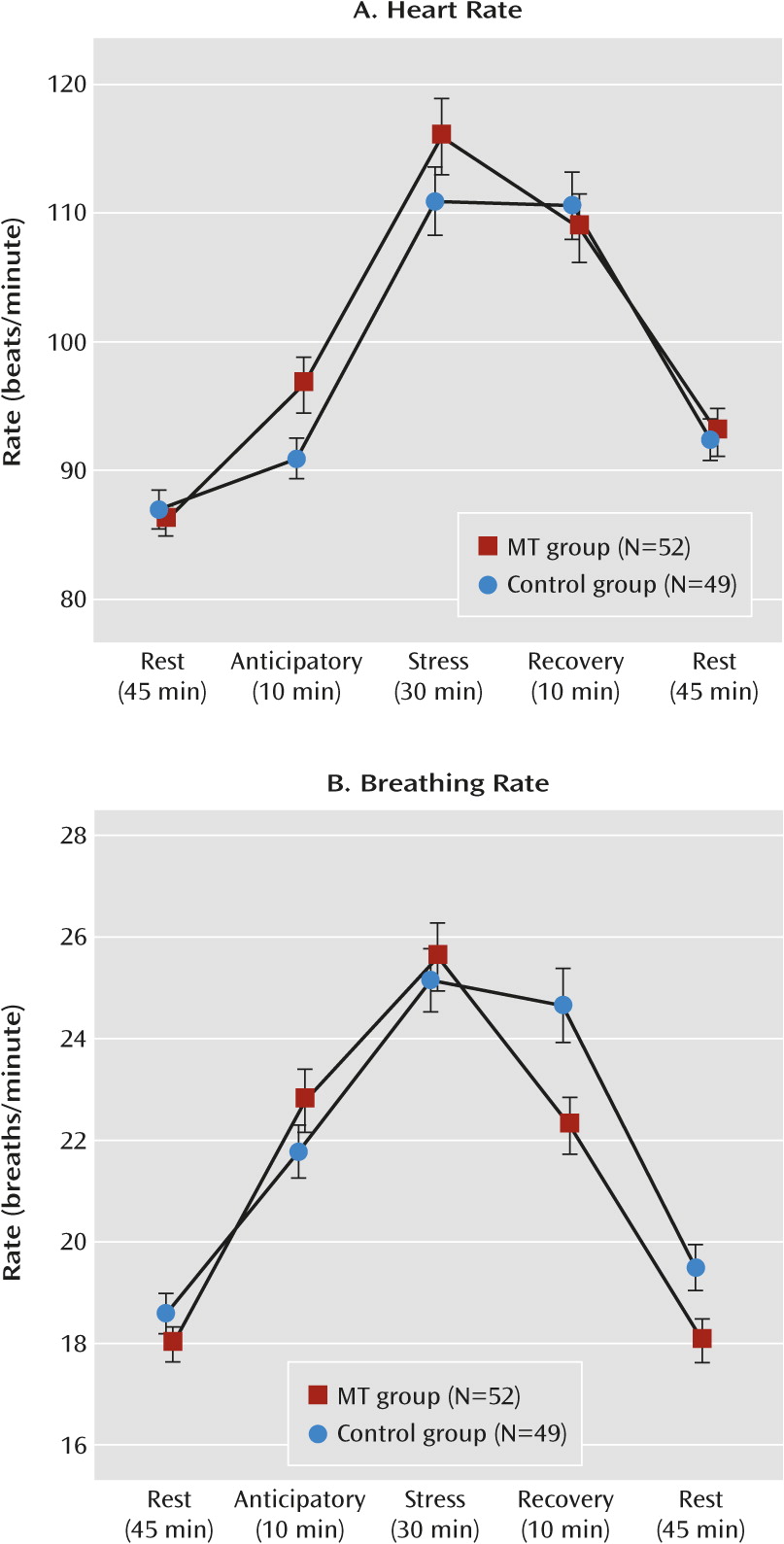
Heart rate.
Using data collected at the IIT facility, we tested for group differences during the anticipation (t=2.13, df=99, p=0.036), response (n.s.), and recovery phases (n.s.), with results suggesting that the groups were significantly different only during anticipation (
Figure 1A). However, we also separately tested the rate of recovery (recovery heart rate minus response heart rate) within each group. The rate of recovery differed significantly between the groups, with the MT group showing a sharper reduction in heart rate (mean=−7.1, SD=14.5; t=3.52, df=51, p<0.001) than the control group (mean=−0.3, SD=10.6; n.s.).
Breathing rate.
We tested for group differences during the anticipation (n.s.), response (n.s.), and recovery phases (t=−2.59, df=99, p=0.011), with results suggesting that the groups were different only during recovery (
Figure 1B). We also separately tested the rate of recovery (recovery breathing rate minus response breathing rate) within each group. As with heart rate, the rate of recovery for breathing rate differed significantly between the groups, with the MT group showing a sharper reduction (mean=−3.3, SD=0.6; t=5.18, df=51, p<0.001) than the control group (mean=−0.5, SD=0.6; n.s.).
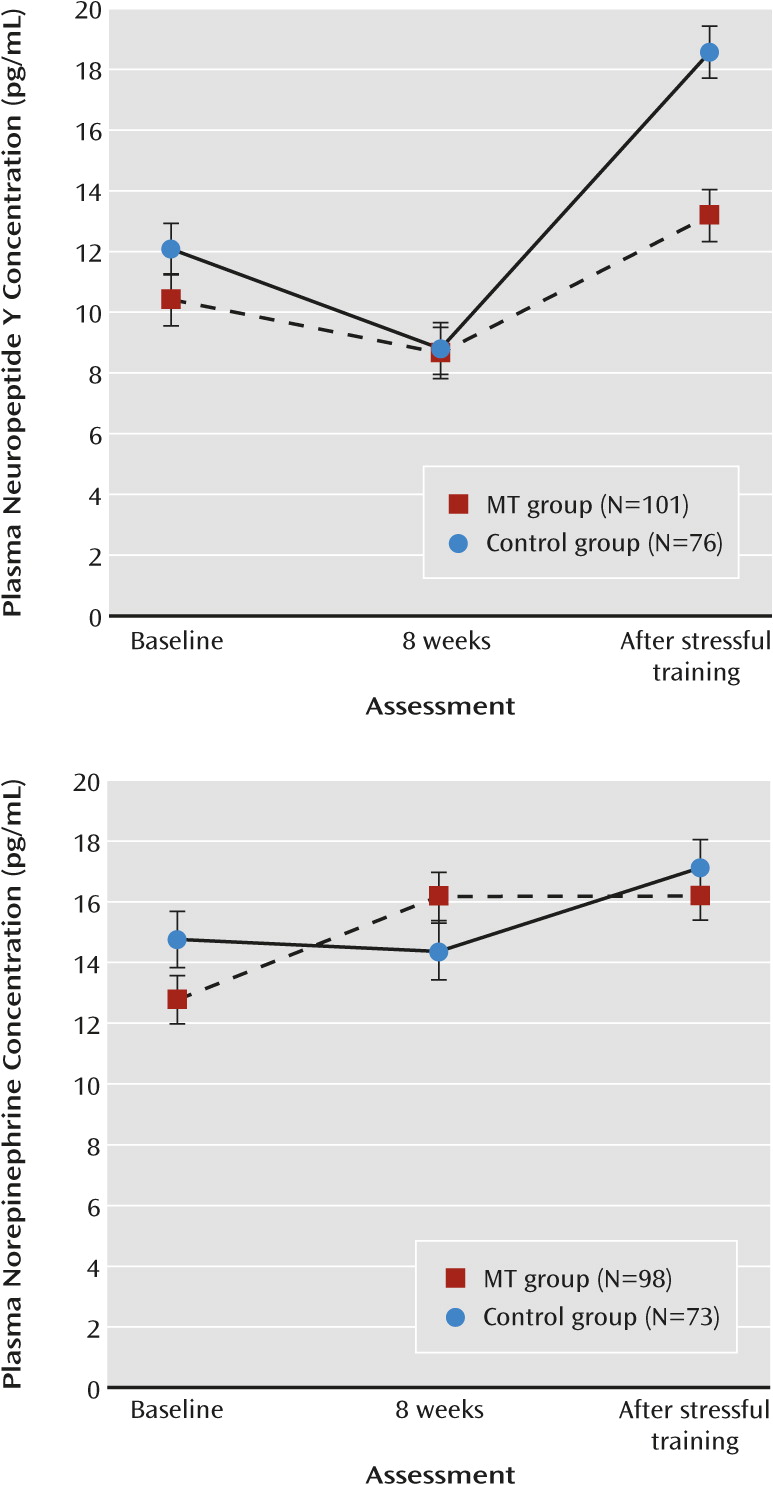
Biomarkers
Group-by-time interaction analysis revealed that plasma concentrations of neuropeptide Y did not differ significantly between the MT and control groups at baseline or at 8 weeks; however, after the stressful IIT session, the MT group had lower concentrations of neuropeptide Y than the control group (
Figure 2). The mean elapsed time from cessation of IIT scenario to plasma extraction did not differ significantly between the MT group (mean=48.2 minutes, SD=20.9) and the control group (mean=45.8 minutes, SD=11.6).
Relationships Between Physiology and Biomarkers
Heart rate was positively correlated with plasma neuropeptide Y concentration during the response (r=0.49, p<0.001) and recovery periods (r=0.50, p<0.001). Breathing rate was negatively correlated with epinephrine concentration during the anticipatory period (r=−0.23, p<0.01).
fMRI
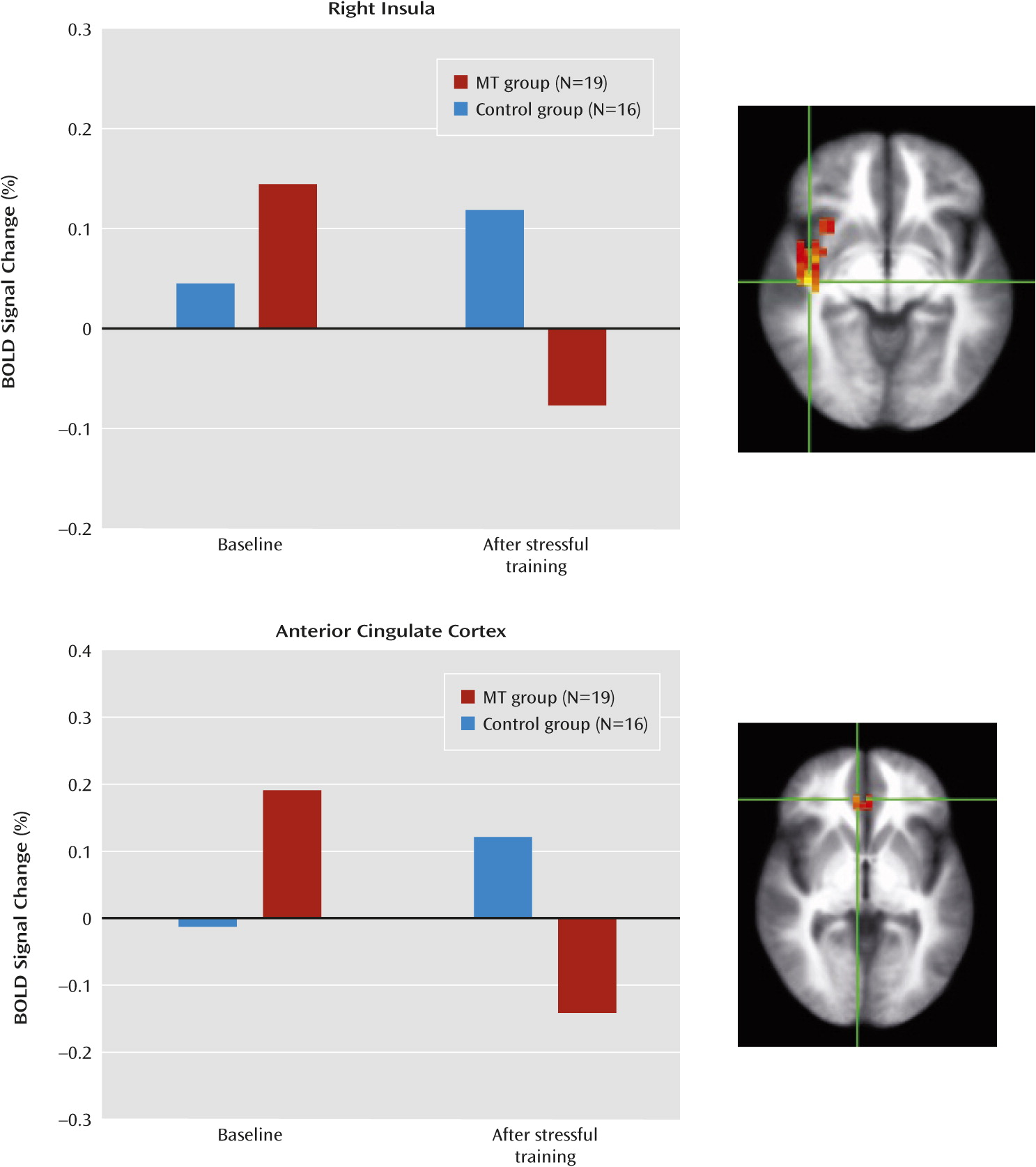
Group differences.
Participants in the MT group showed significant attenuation of brain activation, whereas those in the control group did not (
Figure 3). The MT group showed less activation to emotional faces in the right insula (F=7.88, df=1, 150, p=0.015; d=0.92) and the dorsal anterior cingulate (F=6.83, df=1, 150, p=0.02; d=0.86), which are regions that have been implicated in cognitive control, emotion regulation, reward monitoring, and interoception. Region-specific differences in the group-by-time interaction during the emotion recognition task are summarized in
Table 2.
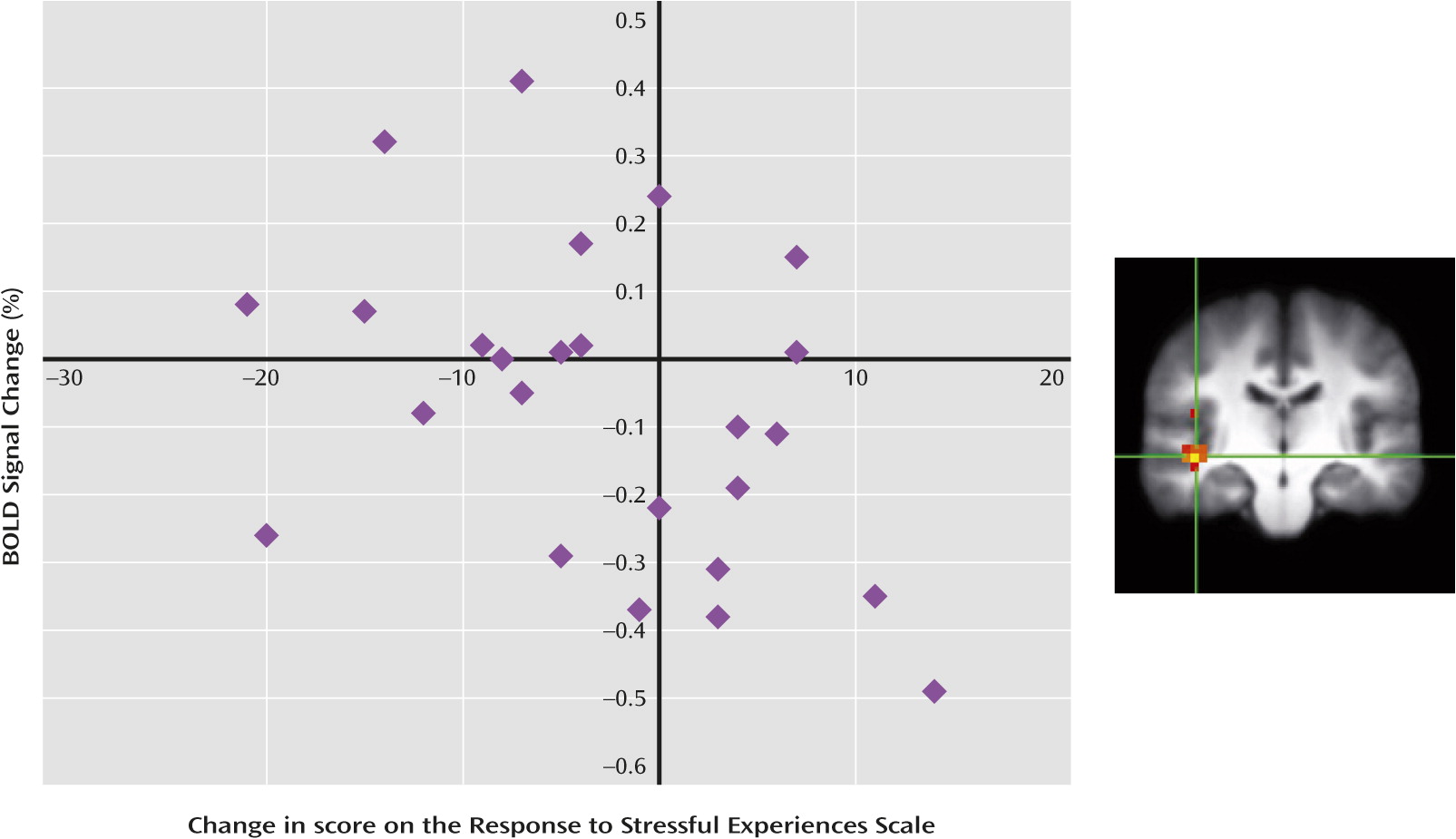
Individual differences.
Interestingly, those individuals who reported greater resilience improvements after MT (as measured by the Response to Stressful Experiences Scale) also showed the greatest reduction of brain activation in the right anterior insula (r=−0.42, p<0.05) (
Figure 4).
Discussion
To our knowledge, this is the first study of the effect of MT utilizing multiple domains of measurement to examine mechanisms underlying recovery from stress in active-duty military personnel prior to deployment. We used a multidimensional approach assessing brain-behavior relationships in a stressful military training environment (Infantry Immersion Training) with high ecological validity (see
Table 3 for a summary of results). Our investigation yielded three main results. First, MT altered heart rate and breathing rate recovery following stressful training. Second, MT modulated a strongly correlated set of peripheral biomarkers before, during, and after exposure to a stressful training session. Third, the neuroimaging results support the hypothesis that MT affects brain structures that are important in integrating information about the internal physiological state and the body’s response to stress. Thus, MT demonstrated beneficial effects across multiple domains indicating enhanced recovery from stress. Moreover, these effects were observed in a nonclinical sample and suggest that responses to stress may be improved through training prior to stress exposure, even in individuals without a mental health condition. Given these results, it is reasonable to speculate that even stronger treatment effects may be observed in treatment-seeking clinical populations. Taken together, these findings constitute evidence for the prevention and treatment of stress-related pathology. In addition, using measures in multiple domains, this study is an important step toward the application of Research Domain Criteria and neuroscience-based diagnoses. The results also have important implications for stress-related mental health research and evidence-based foundations for nonpharmacological prevention and treatment options.
The profile of heart and breathing rate reactivity with MT indicates a more potent response to stress followed by quicker recovery, an effect that remained after controlling for baseline differences in self-reported aerobic fitness as indicated by 3-mile run time. This result is consistent with evidence indicating that cardiorespiratory fitness is associated with greater reactivity to stress followed by enhanced recovery (
36). Furthermore, physiological results from this study directly support the idea that flexibility within a system facilitates adaptive response to stress.
Heart rate and breathing rate are controlled via regions of the brainstem under the influence of higher-order brain regions like the insula. That we found changes in insula function suggests that MT alters function in higher-order brain regions that in turn modulates autonomic outflow to heart rate and breathing rate control centers. This, too, is consistent with evidence suggesting that individuals who adapt well to stress have more efficient deployment of neural processing resources and autonomic responses to stress (
37). Relative to Marines in the control group, those who received MT showed lower sympathetic activation during recovery from stressful immersive training.
Brain activity changes on fMRI in the MT group are consistent with studies identifying a key role for interoceptive networks in responding to affective perturbation. Evidence indicates that higher self-report of mindfulness is associated with reduced activation in the right anterior insula while viewing negative affect images (
38). Similarly, Brefczynski-Lewis et al. (
30) found that relative to nonmeditators, experienced meditators showed attenuated posterior insula activation during a task of attentional control. There is also evidence for an inverse dose-response relationship between insula activation and benzodiazepine administration, suggesting that decreased insula function is associated with reduced perturbation of the interoceptive system (
39). Our findings were similar, with the MT group showing decreased activation in the right insula while responding to emotional faces. Taken together, these findings suggest that a mindful approach to affective perturbation requires fewer cognitive resources. However, such an interpretation regarding the directionality of insula function is incomplete. For example, Farb et al. (
28) found increased functional connectivity between the insula and the medial prefrontal cortex during tasks that demanded self-referencing. Differences in the directionality of activation may speak to functional differences between anterior and posterior insula. Evidence suggests that functional differences between anterior and posterior may correspond to distinctions in awareness of the internal self versus awareness and regulation of affective states (
40). It remains unclear whether self-referential states perturb homeostasis or are different from regulatory modes of interoception.
Relative to the control group, the MT group showed a pattern of altered activation in the right anterior insula and dorsal anterior cingulate cortex after the stressful training session similar to that observed in previous studies by our group in “elite performers” (in both military and civilian samples) relative to healthy subjects (
22–
25). These results suggest that MT may directly modulate interoceptive function toward more efficient processing of cues signaling perturbation of homeostasis and further facilitates improved response to stress.
A limitation of this study was the lack of an active control group. Predeployment training preparation was identical for the MT and control groups with the exception of the MT intervention. Thus, it is possible that some group differences had more to do with the extra time and attention spent on a focused task, not just with the MT content. However, the moderate interaction effect sizes for fMRI, neuropeptide Y, physiology, and sleep quality measures make this explanation less plausible and underscore the value of multidimensional outcome measures in mindfulness research. Moreover, these findings are consistent with independent fMRI studies showing mindfulness-based meditation effects on the anterior insula and anterior cingulate cortex. The extent to which these brain-behavior relationships remain modified as a result of MT and affect behavioral health remains unknown and is worthy of study.
Acknowledgments
John M. Schaldach provided curriculum development support for the intervention. The authors also acknowledge the assistance of Christopher Demuro, Karl Van Orden, Sante Kotturi, Akanksha Shukla, Leila El-kara, Robert Skidmore, Matt Fennell, Rose McDermott, Tom Liu, and Anet Petrosyan.