Operations Iraqi Freedom and Enduring Freedom have deployed approximately 2.5 million troops to Iraq and Afghanistan, approximately 13%−20% of whom will develop posttraumatic stress disorder (PTSD) (
1,
2). The PTSD treatment with the most empirical support is prolonged imaginal exposure (
3). This comprises 8–12 individual therapy sessions involving repeated recounting of the traumatic memories, including emotional processing of the content and in vivo exposure (
4). Virtual reality exposure therapy, using head-mounted computer simulations of sights, sounds, vibrations, and smells tailored to the patient’s individual trauma, has successfully augmented imaginal exposure (
5,
6).
Repeated therapeutic activation of the trauma memory allows new information to be encoded, thus reducing the memory-associated fear and anxiety (
7). This learning is an active process involving synaptic modification in the amygdala that may be pharmacologically augmented to improve the extinction learning underlying therapy (
8).
d-Cycloserine is an
N-methyl-
d-aspartate (NMDA) glutamate receptor partial agonist (
8) shown to improve the efficacy and durability of exposure therapy when a single dose is given just before treatment for several anxiety disorders (
9–
13), although
d-cycloserine did not enhance a full course of cognitive-behavioral therapy (CBT) in a large trial of patients with social phobia (
14). In contrast, enhancing γ-aminobutyric acid (GABA) activity with benzodiazepines may interfere with fear extinction (
15). However, it is unknown whether benzodiazepines diminish the efficacy of exposure therapy in PTSD patients. This question is important clinically because benzodiazepines remain widely used in PTSD (
16), contrary to the treatment guidelines of the Department of Veterans Affairs (VA) and Department of Defense (
17).
In a civilian PTSD group, overall outcomes of prolonged imaginal exposure were not significantly improved with added
d-cycloserine, compared with placebo, although there was greater symptom reduction among patients who required more sessions (
18). In a recent study of veterans of Operations Iraqi Freedom and Enduring Freedom,
d-cycloserine added to prolonged exposure produced less improvement than placebo (
19). Most recently, the combination of virtual reality exposure with
d-cycloserine was superior to placebo in the treatment of civilians with PTSD (
20).
An important potential biomarker of treatment outcome is hypothalamic-pituitary axis reactivity, specifically, increased cortisol reactivity to a psychosocial stressor. In women with PTSD, open-label treatment with serotonin-selective reuptake inhibitors reduced cortisol reactivity to a cognitive challenge (
21), but no PTSD study of which we are aware has been a randomized controlled trial with cortisol reactivity as an outcome measure. Another physiological marker is exaggerated startle, a cardinal symptom of PTSD (
22), although it has not been examined as a treatment outcome measure. Because startle response can serve as a measure of reactivity in both humans (
23) and animals (
8), it may function as an indicator of treatment mechanism in exposure therapy.
In the current study, veterans with combat-related PTSD were randomly assigned to receive
d-cycloserine, alprazolam, or placebo 30 minutes before each of five sessions of virtual reality exposure. We hypothesized that treatment outcomes in the patients receiving
d-cycloserine would be superior to those for the placebo group, whereas patients assigned to alprazolam would have an outcome inferior to that with placebo. To examine biomarkers of treatment effect, we collected data on cortisol and startle response. Prior work has demonstrated that the beneficial effects of
d-cycloserine occur when sufficient extinction learning has occurred (
10,
24,
25). In this study, extinction learning across exposure sessions was explored as a conditional effect of treatment response. Extinction learning was defined in the present study as the average decrease in peak ratings of subjective discomfort across exposure sessions.
Method
This double-blind, placebo-controlled study consisted of a baseline screening assessment, six treatment visits, and follow-up assessments at 3, 6, and 12 months posttreatment conducted by blind independent evaluators. The participants were randomly assigned in a 1:1:1 ratio to the three treatment conditions: virtual reality exposure plus 50 mg of d-cycloserine, virtual reality plus 0.25 mg of alprazolam, or virtual reality plus pill placebo. The compounding pharmacy randomly assigned patients to the medications in blocks of 30. The study staff were blind to medication condition. The institutional review boards of Emory University and the Atlanta VA Medical Center approved this study.
Participants
The study participants were 156 medically stable Iraq and/or Afghanistan veterans between 22 and 55 years old who met the DSM-IV criteria for PTSD due to military trauma, which was verified through the participant’s discharge papers. The exclusion criteria included a lifetime history of psychosis, bipolar disorder, current suicidal risk, current alcohol or drug dependence, pregnancy, and current use of medications that could confound the data (glucocorticoids, benzodiazepines, chronically used opioids). Mild traumatic brain injury was permitted. The patients were required to have discontinued taking long-acting benzodiazepines for 1 month and short-acting benzodiazepines for 2 weeks before screening. Participants taking other psychotropic medications must have been taking stable doses for at least 2 weeks before beginning the study and were required to maintain a stable dose throughout the study. As-needed pain medication was prohibited on study treatment days. Participants received $50.00 after each assessment visit and $15.00 travel reimbursement per treatment session. After complete description of the study to the subjects, written informed consent was obtained.
Assessments
At the baseline screening visit, a master’s-level clinician administered the Clinician-Administered PTSD Scale (CAPS) (
26) to assess PTSD diagnosis status, using the most traumatic incident identified by the patient. The Mini International Neuropsychiatric Interview (MINI) (
27) was administered to evaluate other axis I disorders. The participants completed several self-report measures, including the PTSD Symptom Scale (
28). All assessment interviews were videotaped to assess interrater reliability. Ten percent of the MINI and CAPS interviews were randomly selected to monitor the reliability of the interview process. All assessments were performed when the participants were free of study medication.
At each assessment, the participants were exposed to standardized 2-minute virtual reality scenes. Startle responses were elicited by 40-ms, 106-dB white noise bursts during each scene, as well as in the presence of blank blue squares, at a variable 15–45-second interstimulus interval. The responses were measured by using electromyography of the orbicularis oculi muscle contraction. Salivary cortisol samples were collected immediately before, immediately after, and 15 minutes after scene presentation. The samples were immediately frozen and batch-processed by using a chemiluminescent immunoassay. All samples were run in duplicate, and three levels of quality control were processed in every assay. The detection limit for the salivary assay was 0.1 nmol/L. The interassay and the intra-assay coefficients of variations were under 10%.
Treatment
All participants were seen individually for one 90-minute introductory session that included information gathering, treatment planning, and an explanation of the treatment rationale. This was followed by five weekly 90-minute sessions of virtual reality exposure delivered by doctoral-level clinicians. Each participant arrived 30 minutes before the virtual reality session, was given questionnaires to complete, and took a single pill under the supervision of study personnel. During the virtual reality sessions, participants were encouraged to expose themselves to their most traumatic memories, following guidelines for standard exposure therapy (
4). The therapist viewed the virtual environments on a video monitor and attempted to match stimuli that the patient described. The therapist encouraged continued exposure (30 to 45 minutes) until anxiety decreased. The participant’s anxiety level was assessed every 5 minutes through the use of a subjective rating of discomfort (0=no anxiety, 100=maximum anxiety). Exposure was followed by 15–20 minutes of processing of the experience, integrating material from the exposure, and making new associations explicit. Other than the virtual reality exposure, the only differences from standard exposure therapy were that no homework was assigned, as the design dictated exposure only in conjunction with the study medication, that the participant’s eyes were open to view the virtual reality scenes, and that only six sessions were administered.
Apparatus
During the virtual reality sessions, the participant wore an eMagin Z800 head-mounted display (eMagin Corp., Bellevue, Wash.) that included separate screens for each eye, integrated head tracking, and stereo earphones. The participant was presented with a computer-generated view of a virtual Iraq or Afghanistan environment that changed in a natural way with head and body motion. A handheld controller allowed the participant to navigate within the environment at his or her own pace, in a simulation of either 1) driving a Humvee down a desert highway alone or in a convoy or 2) navigating on foot through Iraq-like city scenes. Trigger stimulus options were of four types: auditory, visual, olfactory, and tactile. The auditory stimuli included weapons fire, explosions, incoming mortars, helicopter flyovers, prayer calls, and radio. The visual stimuli included night vision, smoke, explosions, civilians, and burned vehicles. The olfactory stimuli were burning rubber, diesel fuel, weapons fire, and Middle Eastern spices. The tactile stimuli included vibrations and were delivered through a raised platform with a subwoofer driven by an audio amplifier. The therapist delivered trigger stimuli through a network linked to the virtual reality personal computer.
Statistical Analyses
A piecewise mixed-effect model was used to test the hypotheses that 1) d-cycloserine would produce outcomes superior to those with placebo and 2) alprazolam would not be superior to placebo. Piecewise models were used to estimate separate slopes for distinct time periods, such as active treatment and follow-up. The model included an intercept representing the posttreatment assessment, a slope representing the magnitude of change from baseline to posttreatment, a slope representing the magnitude of change from posttreatment to 12-month follow-up, and dummy-coded variables for d-cycloserine and alprazolam that assessed the specified hypotheses with α=0.025. Terms for interactions between the dummy-coded variables and the slopes assessed differences in change during treatment and follow-up. Rates of PTSD diagnoses, based on the CAPS, were compared at posttreatment and at the 3-, 6-, and 12-month follow-ups by means of chi-square tests. Outcomes were analyzed on the basis of the intent-to-treat group of all randomly assigned participants.
An exploratory analysis was conducted to examine extinction learning, which was calculated as the difference between peak subjective distress ratings in successive sessions. The mean of these differences was used as an index of average extinction learning across treatment. This mean was included as a fixed effect predicting posttreatment scores, as an interaction with the dummy-coded contrasts to assess the interactive effect of extinction learning on outcomes across the conditions. When the effect was significant, 95% confidence intervals (CIs) were constructed to identify the level of extinction learning in which a significant difference between the conditions was detected at α=0.05 (
29).
Repeated-measures analysis of variance (ANOVA) was used to analyze the effects of the virtual reality scenes on cortisol levels across time. Within-subject variables included sample (before, after, and 15 minutes after virtual reality) and time (baseline, posttreatment, and 6-month follow-up). Effects of treatment condition (d-cycloserine, alprazolam, and placebo) were examined as a between-groups variable. The same analysis was repeated with startle response used as the dependent variable. The time and group variables were the same as in the preceding analysis, but the virtual reality included two levels (virtual reality scene, blue square) and an additional variable was included for block (two blocks were presented).
Results
In all, 156 participants were randomly assigned to
d-cycloserine (N=53), alprazolam (N=50), and placebo (N=53). The flow of participants through the study is depicted in Supplemental Figure 1, which appears in the
data supplement accompanying the online version of this article. There were no significant differences in dropout rate across conditions at posttreatment (χ
2=3.36, df=2, p=0.19) or at the 3-month (χ
2=3.63, df=2, p=0.16), 6-month (χ
2=2.75, df=2, p=0.25), or 12-month (χ
2=1.11, df=2, p=0.57) follow-up. Dropouts did not significantly differ from completers on baseline demographic characteristics or symptom variables. Little’s test suggested that the missing cases met the assumption for missing completely at random (χ
2=124.89, df=127, p=0.54). There were no meaningful between-group differences at baseline (
Table 1). A randomly selected subset of diagnostic interviews (N=47) were reviewed by a master’s-level clinician to calculate the interrater reliability, and the agreement for the primary diagnosis across assessments was 100%.
Efficacy Comparisons
Across all conditions there was a significant effect over the course of the trial for scores on the CAPS (b=−12.19, CI: −16.04 to −8.33, p<0.001; d=1.56) and on the self-rated PTSD Symptom Scale (b=−4.68, CI: −6.56 to −2.80, p<0.001; d=1.16) (
Table 2). The effect for the CAPS was maintained over 12 months (b=−1.19, CI: −1.86 to −0.53, p<0.001), but this was not the case for the PTSD Symptom Scale (b=−0.22, CI: −0.54 to 0.11, p=0.20).
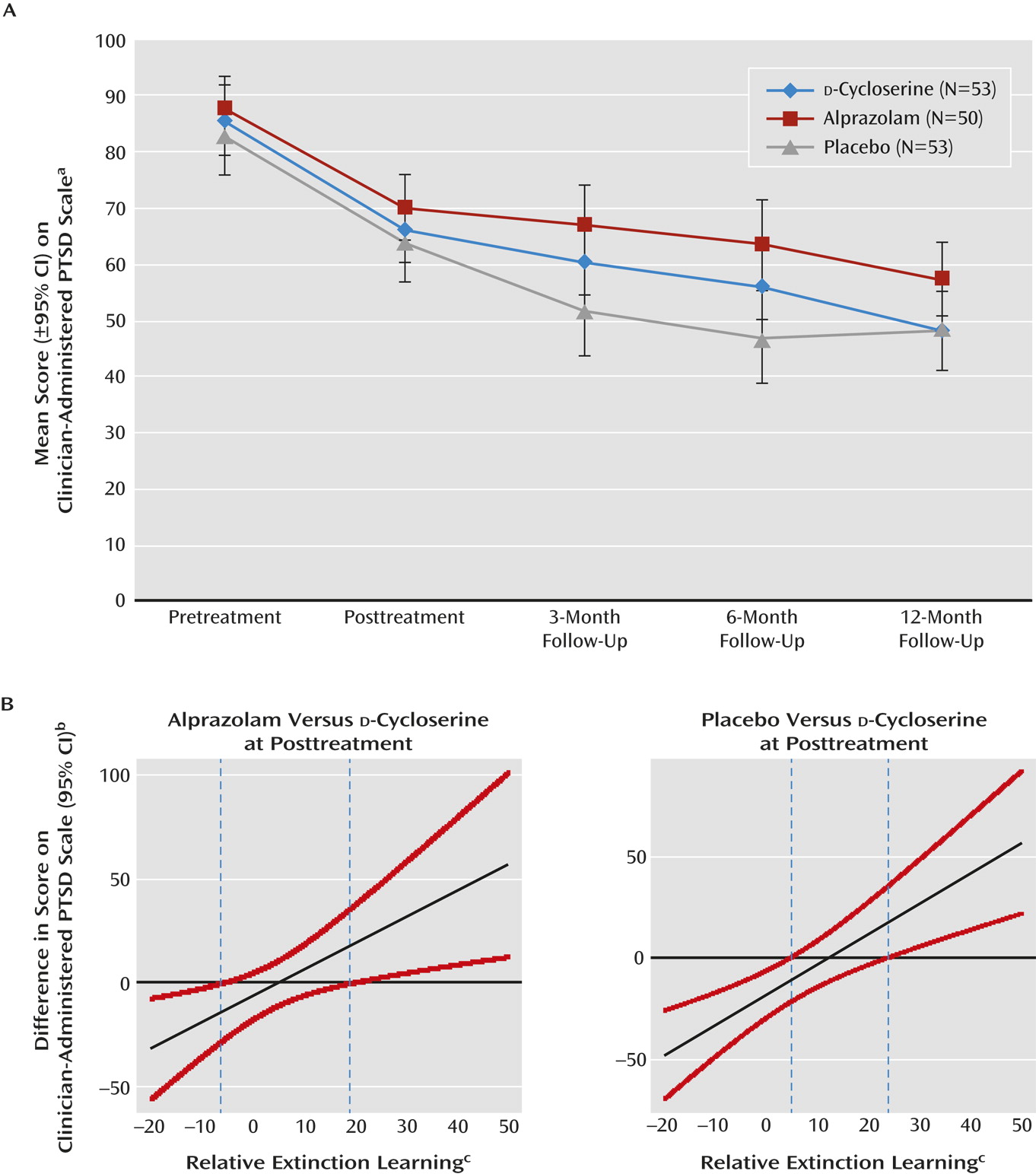
Analyses of posttreatment differences were made according to a priori planned contrasts (
Figure 1A). There was not a significant difference between
d-cycloserine and placebo at posttreatment on the CAPS (b=4.46, CI: −1.40 to 10.33, p=0.14) or the PTSD Symptom Scale (b=4.76, CI: −0.39 to 9.92, p=0.07). The interaction between change from pretreatment to posttreatment and condition was not significant in the analysis of the
d-cycloserine and placebo conditions, for either the CAPS (b=4.46, CI: −4.68 to 14.39, p=0.32) or the PTSD Symptom Scale (b=3.00, CI: −1.66 to 7.66, p=0.21), which suggests that the change from baseline to posttreatment did not differ between
d-cycloserine and placebo. The interaction between 12-month score and condition was also not significant in the comparison of
d-cycloserine and placebo for either the CAPS (b=−0.56, CI: −2.24 to 1.12, p=0.52) or PTSD Symptom Scale (b=−0.23, CI: −1.06 to 0.59, p=0.59).
There was a significant difference between the alprazolam and placebo conditions at posttreatment on the CAPS (b=7.88, CI: 2.28 to 13.48, p=0.006) but not on the PTSD Symptom Scale (b=2.61, CI: −2.23 to 7.45, p=0.29). The interaction of posttreatment change and condition was not significant in the comparison of alprazolam and placebo for either the CAPS (b=3.57, CI: −5.70 to 12.84, p=0.45) or the PTSD Symptom Scale (b=1.93, CI: −2.61 to 6.48, p=0.41). The interaction of 12-month score and condition was also nonsignificant in the comparison of alprazolam and placebo for the CAPS (b=0.07, CI: −1.51 to 1.65, p=0.94) and the PTSD Symptom Scale (b=0.04, CI: −0.74 to 0.82, p=0.92). Finally, a significantly greater proportion of participants in the alprazolam condition met full PTSD criteria relative to the proportion of participants in the placebo condition at 3 months (χ
2=7.11, df=1, p=0.008) (
Table 3). This difference was not observed at other time points.
Conditions of Treatment Response
Extinction learning.
There was a significant interaction between learning (
30,
31) and treatment condition that suggested the association between extinction learning and posttreatment scores on the CAPS (b=−2.19, CI: −3.44 to −0.94, p=0.001) and PTSD Symptom Scale (b=−0.82, CI: −1.19 to −0.45, p=0.001) were associated with extinction learning for the
d-cycloserine condition only. The association between extinction learning and outcomes was not significant for the placebo condition (CAPS: b=0.59, CI: −0.04 to 1.22, p=0.07; PTSD Symptom Scale: b=0.11, CI: −0.08 to 0.32, p=0.26) or the alprazolam condition (CAPS: b=−0.17, CI: −0.97 to 0.62, p=0.67; PTSD Symptom Scale: b=−0.04, CI: −0.42 to 0.35, p=0.85). These findings suggest that extinction learning was associated with posttreatment scores for the
d-cycloserine condition but not for the placebo and alprazolam conditions. To further clarify this interaction, 95% confidence bands were calculated for the difference in posttreatment scores on the CAPS between the
d-cycloserine condition and the other conditions (
Figure 1B). Relative to the posttreatment outcomes for patients in the alprazolam and placebo groups, outcomes were better for patients in the
d-cycloserine condition whose extinction learning scores were higher by 18.99 (alprazolam) and 23.94 (placebo). Patients in the
d-cycloserine group had worse outcomes when their extinction learning scores were 6.29 points less than those in the alprazolam group or 4.78 points less than those in the placebo group.
Biomarkers.
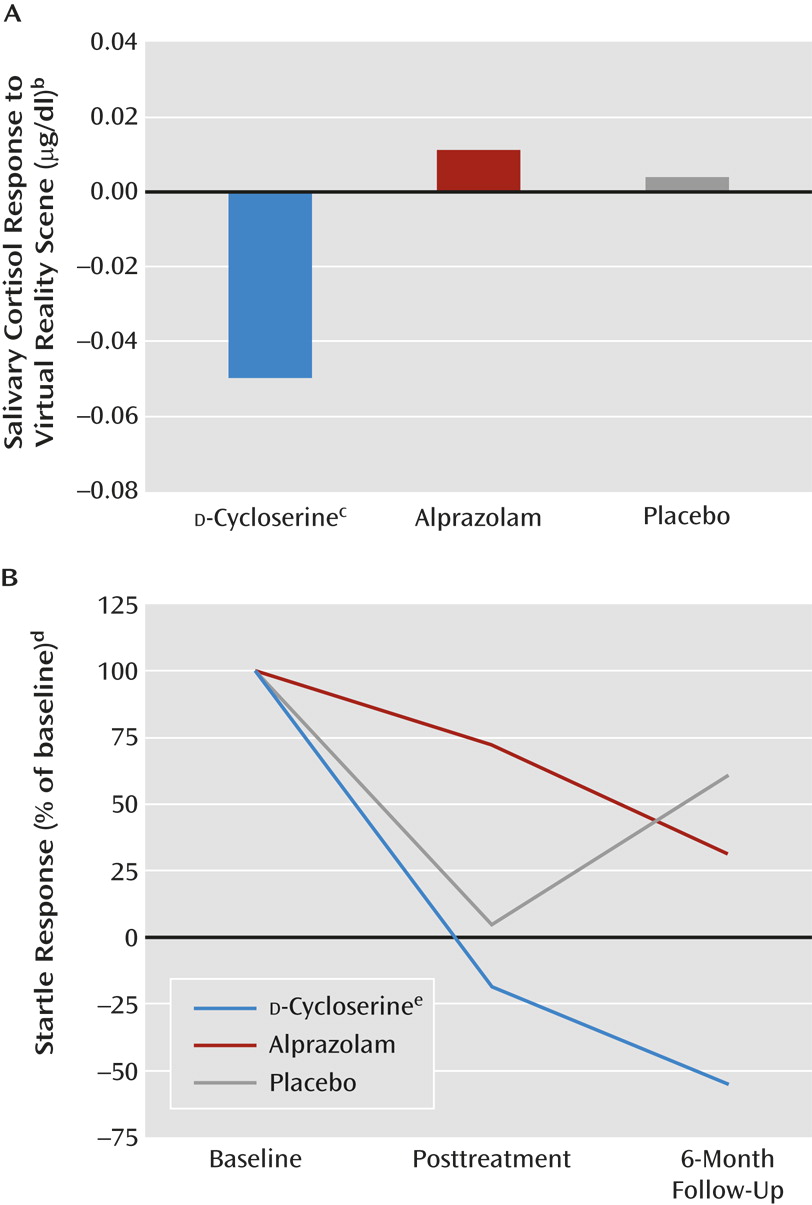
Cortisol data were available for 104 individuals at baseline and for 39 individuals at all three time points when data were collected (baseline, posttreatment, and 6-month follow-up). Cortisol levels preceding the virtual reality exposure did not differ between conditions (p=0.59). A repeated-measures ANOVA of cortisol levels revealed a significant interaction of time and sample (before, after, or 15 minutes after virtual reality) (F=2.43, df=4, 152, p=0.05). The cortisol response to virtual reality exposure at the end of treatment is shown in
Figure 2A. A repeated-measures ANOVA of change in cortisol level from before to 15 minutes after virtual reality revealed a significant time-by-condition interaction (F=2.58, df=4, 72, p<0.05), with the change score decreasing more in the
d-cycloserine group after treatment than in the alprazolam and placebo groups (p<0.05 in both comparisons).
Data on startle response were available for 117 patients at baseline and 32 patients at all three time points. A repeated-measures ANOVA indicated a significant four-way interaction of time, virtual reality, block, and condition (F=2.74, df=4, 58, p<0.05). Follow-up analyses within each treatment condition showed that treatment had a significant effect on the startle response during the virtual reality scenes only in the
d-cycloserine group (F=6.24, df=2, 12, p=0.01). After correction for group differences in startle response at baseline, the
d-cycloserine group again showed a significant percentage change from baseline with time (F=51.65, df=2, 12, p<0.001), while the other groups did not (
Figure 2B).
Discussion
To our knowledge, this is the first randomized controlled clinical trial of treatment for veterans with PTSD that has used virtual reality exposure combined with d-cycloserine, alprazolam, or placebo. The most significant findings with potential clinical implications include the following: 1) six sessions (five with virtual reality exposure) were associated with significant improvement in PTSD symptoms at posttreatment that was maintained at follow-up, although there was no control for the virtual reality exposure; 2) the primary hypothesis of d-cycloserine enhancement was not supported overall, but d-cycloserine enhanced PTSD symptom outcomes in patients with more between-session learning; 3) alprazolam use during treatment was associated with diminished efficacy of exposure therapy, with more severe posttreatment symptoms and higher rates of PTSD diagnosis at the 3-month follow-up relative to placebo; and 4) two neurobiological biomarkers, salivary cortisol level and startle response, were sensitive to treatment gains and indicated differential treatment response favoring d-cycloserine. The effects of d-cycloserine augmentation of virtual reality exposure in this group of veterans with PTSD are inconclusive. The primary hypothesis of overall differences in scores on the CAPS was not supported, but d-cycloserine demonstrated benefits on secondary measures (cortisol and startle) in exploratory analyses.
These results suggest that virtual reality exposure therapy attenuated cortisol and startle responses to a trauma-relevant scene. Reduced cortisol reactivity after 12 months of paroxetine treatment of PTSD has been observed previously (
21); the current study expanded this finding to a placebo-controlled randomized trial and demonstrated the effect after 6 weeks of treatment. Patients who received
d-cycloserine had greater posttreatment reductions in cortisol and startle responses than did either the alprazolam or placebo group. Although
d-cycloserine has shown enhanced extinction of fear-potentiated startle in animal studies (
8), this is the first study we are aware of showing effects of
d-cycloserine on fear-potentiated startle in PTSD patients.
As a potential targeted pharmacological agent for the augmentation of extinction learning, which is believed to underlie exposure-based psychotherapy,
d-cycloserine was initially shown to enhance extinction of conditioned fear in rodent models (
8). This finding was rapidly replicated in a number of additional animal studies, which showed that
d-cycloserine enhances the consolidation phase of fear extinction, increases the rate of between-session extinction learning, and reduces fear reinstatement (
32). These promising preclinical studies were translated across a number of exposure therapy paradigms in humans with clinical anxiety disorders (
9–
13). Despite these promising findings, studies examining fear extinction in healthy humans by using skin conductance response indicated no
d-cycloserine enhancement of extinction training or recall (
33,
34). However, as in the rodent studies,
d-cycloserine was found to significantly reduce reinstatement of fear after extinction (
34), demonstrating potential long-term benefits of extinction learning. Given the role of
d-cycloserine in learning, it may have contributed to more long-lasting extinction of responses to the virtual reality scenes (as seen in
Figure 2B).
Therefore, we believe that the reduced reactivity to trauma-related cues following treatment was likely due to treatment-related learning effects (i.e., extinction) and that
d-cycloserine enhanced these learning effects. Additionally, our data showing that extinction learning was associated with posttreatment scores for the
d-cycloserine condition, but not for the other conditions, is consistent with the increasing evidence that
d-cycloserine’s clinical effect may be best observed through enhancing consolidation of extinction gains made between sessions (
10,
14,
24,
25,
35) and preventing return of symptoms after treatment. Together these effects may represent the NMDA-dependent augmentation of relatively weak components of extinction learning, which may be difficult to identify in the patients’ clinical ratings in the context of the robust effects of exposure therapy.
Strengths of the current study include the novel treatments offered, the combination of treatments, and the use of biomarkers. Use of virtual reality exposure has been advocated for this cohort of veterans because this generation is familiar with video games and finds virtual reality exposure therapy more acceptable than talk therapy and because virtual reality is very evocative and may assist emotional engagement in exposure therapy (
30). Improvements in only six sessions in this study were comparable to results from other studies in veterans that administered more sessions of prolonged exposure (
31). We believe that the comparison of
d-cycloserine and alprazolam with placebo is novel. The study was well controlled, with objective measures at every assessment point, including long-term assessment by blinded independent assessors.
Weaknesses of the current study include the high dropout rate. It should be noted that 31 participants dropped out before the first treatment session. Many of these participants came to be assessed after completing the PTSD 101 course at the local VA hospital. Seeking treatment is encouraged after the course. Many of these individuals may have attended the baseline assessment to be compliant and for monetary reimbursement. Although disheartening, the dropout rate is similar to rates in other studies with veterans and active duty personnel (
31). There were also differences in how the data were analyzed between the clinical measures and the biological measures (cortisol, startle) that were necessitated by differences in data type.
In conclusion, we observed an apparent response to a brief course of virtual reality exposure in this cohort of veterans, although there was no treatment control for the virtual reality exposure. As previously thought (
17), we should be cautious in the use of benzodiazepines in patients with PTSD; in this study they seemed to have attenuated overall response in the long term. The
d-cycloserine results are less conclusive: there was a clear drug effect favoring
d-cycloserine on salivary cortisol and startle biomarkers and a more complicated advantage in clinical symptoms among participants who experienced good extinction learning between sessions. There may be a subtype of participants for whom
d-cycloserine will enhance learning during exposure therapy.