Antisocial personality is a common problem that is debilitating for the individual and disruptive for others. People with antisocial personality manifest two sets of problems. First, they persistently engage in antisocial behavior, including physical aggression, lying, rule-breaking, and crime. Second, they display pervasive antisocial character traits across three domains: emotional coldness, with callous-unemotional indifference to the distress of others; impulsiveness, including irresponsibility and irritability; and interpersonal problems, including manipulativeness and an inability to form enduring relationships (
1). More severe cases meet criteria for antisocial personality disorder, which affects 3%–5% of adults (
2). Such individuals pose a major problem to society, frequently committing violent and criminal acts (
3). By age 28, the most antisocial 3%–5% of children cost society 10 times more than comparison subjects (
4), estimated at an extra $2.6–$4.4 million (
5). Underpinning the phenomenology, brain scanning studies show reduced gray matter volume in areas implicated in empathic processing and moral reasoning (Brodmann’s areas 10, 20/38) (
6). Antisocial personality is notoriously difficult to treat; the only published intervention trial found cognitive-behavioral therapy to be ineffective (
7). Because of the severe impairment, high social cost, and untreatability of established antisocial personality in adulthood, examining the feasibility of prevention is a public health priority.
Antisocial personality is increasingly seen as a lifespan developmental disorder with its origins in childhood (
1–
3), and the presence of conduct disorder in childhood is a prerequisite to diagnosis of the disorder. Community surveys find that around 10% of children with antisocial behavior will develop antisocial personality disorder in adulthood (
2), and the proportion rises to over a third in clinic-referred cases (
8); a higher proportion develop less extreme forms. Many authoritative bodies advocate early intervention. For example, the Institute of Medicine (
9) has called for early intervention studies for antisocial personality and other mental disorders, and the U.S. Surgeon General’s report on youth violence (
10) recommended rigorous evaluation of prevention programs. The U.K. National Institute for Health and Clinical Excellence (NICE) recommends parent training in childhood to prevent the development of antisocial personality disorder (
2). However, to date there is scant evidence to support these recommendations; to our knowledge, this study is the first to address the issue.
Antisocial personality is a condition that is well suited for early intervention. First, the antisocial behavior component is reliably identifiable early in childhood (
11). Second, although the majority of antisocial children do not end up with antisocial personality disorder, there is nonetheless strong continuity of antisocial outcomes to adulthood. For example, a representative longitudinal survey that identified the most antisocial 5% of children at age 7 found, at age 28, an 11-fold greater incidence of violent offending relative to comparison subjects (35% compared with 3%), a fourfold greater incidence of heavy drug use (20% compared with 5%), and a ninefold greater incidence of leaving school with no qualifications (52% compared with 6%) (
12). Third, antisocial personality is amenable, at least in the short term, to early intervention. Meta-analyses confirm that parent training programs (which typically last 10–12 weeks and teach skills for promoting a positive relationship alongside calm discipline) are a successful intervention for childhood disruptive behavioral disorders that may presage antisocial personality, but few studies have follow-up data beyond 1–3 years (
13,
14). A notable exception was the Fast Track trial, a model selective prevention program that started with antisocial 7-year-olds and provided parent training and other interventions over several years. However, follow-up into adulthood showed no overall effects, although subgroup analysis found improvements for the most antisocial children (
15).
The second component of antisocial personality, antisocial character traits, is apparent and stable by adolescence, when such traits reliably predict progression to adult antisocial personality (
16,
17). Empirical trials confirm that parenting interventions may be effective for younger children with antisocial character traits (
18), but no studies have yet shown any intervention to be effective in preventing antisocial personality in the longer term. A follow-up to adulthood of a school intervention using behavioral feedback from classmates found no overall effects on the emergence of antisocial personality, although there were possible improvements for a more severe subgroup (
19).
In the present study, we examined the long-term effects into adolescence of early parent training on the two elements of antisocial personality—antisocial behavior and antisocial character traits. If treatment gains from an earlier intervention persist to adolescence, then there is reason to believe that they will endure into adulthood, since persistent antisocial behavior seldom increases or emerges after adolescence. The proximal target of the intervention, parenting, was measured using expressed emotion, quality of supervision, and directly observed interaction style. We also measured the adolescents' reading achievement, an important independent predictor of long-term antisocial and social adjustment outcomes that may also be improved by parenting interventions (
20).
A key feature of this study is the analysis of two different types of treatment trials. We examined whether long-term intervention effects were comparable in an indicated sample of clinic-referred children and a selective sample of high-risk community (non-clinic referred) children. An indicated approach is simpler to administer, as there are fewer children with severe problems, they are easier to identify, and their parents are usually prepared to engage in treatment; however, the problems may already be too entrenched to treat. In contrast, a selective approach targets milder cases, but because problems are less established, whole populations have to be screened and fewer cases will go on to develop serious problems (
21); also, parents may be less willing to engage in treatment. There has long been debate in the prevention literature about the relative merits of each approach; some have argued that resources should be shifted from intervention with established disorders to selective early intervention (
22). Discovering whether there are differences in the long-term effectiveness of the two approaches may help guide strategies for large-scale prevention and public health improvement.
Our aims in this study were 1) to discover whether a high-quality parent training program (the Incredible Years program) (
23) given to parents of children 3–7 years old would have persisting effects into adolescence on oppositional defiant disorder symptoms and antisocial personality character traits (the two primary outcome measures) and on adolescent antisocial behavior, adolescent reading ability, and quality of the parent-child relationship (the three secondary outcome measures); and 2) to examine whether the long-term effects of early intervention would be greater with an indicated or a selective prevention strategy.
Method
Design
This study is a follow-up after 4–10 years (mean=7 years) of two high-quality randomized controlled trials that met criteria to be included in stringent meta-analyses (
14). The follow-up (called the Study of Parents’ and Adolescents’ Experiences; the protocol is available at
http://www.kcl.ac.uk/iop/depts/cap/research/napr/our-research-projects/space.aspx) was approved by the research ethics committee of King's College London, and written informed consent was obtained from parents and adolescents.
Indicated Early Intervention Study
Participants.
A total of 120 children 3–7 years old who were referred to child mental health clinics by family doctors because of antisocial behavior were enrolled in a pragmatic controlled trial (
24). Their mean antisocial behavior severity was above the 97th percentile (
Table 1). They were initially allocated to parent training groups (N=73), waiting list (N=37), or usual management (N=10). After 6 months, families in the waiting list group were randomly allocated to parent training (N=21) or usual management (N=16); thus, overall, 94 families were allocated to parent training and 26 to usual management (see Figures S1 and S2 in the
data supplement that accompanies the online edition of this article). Families allocated to parent training showed a large reduction in child antisocial behavior after treatment compared with controls (effect size=1.1 standard deviations), and the improvement was maintained at 18-month follow-up (
25).
Parenting intervention.
The Incredible Years basic videotape program, which has a strong evidence base (
23), was offered to groups of parents of six to eight children over 13–16 weeks. The program covers play; praise and rewards; limit setting; and handling misbehavior. In each session, videotaped scenes of parents and children together are shown, depicting “right” and “wrong” ways of handling children. Parents are supported while they practice alternative ways of managing their children, and homework is assigned. Parents attended a mean of nine sessions, 74% of those offered. Therapists held regular jobs in their local service; they received training over 3 months and accreditation from the program developer. During the study, they brought videotapes of treatment sessions to weekly supervision to ensure adherence to the manual.
Control intervention.
The control condition was individualized treatment in child mental health clinics by trained mental health staff. Typically the parent and child were seen together and separately; parents received supportive psychotherapy, and children received help in understanding why they might feel angry or frustrated and in exploring strategies to change this. Families attended a mean of six sessions, 63% of those offered. Five children in this arm were treated with methylphenidate; none of the children in the parenting group arm received psychotropic medication.
Follow-up.
Data for these analyses were collected 5.6–10.5 years after the intervention was completed (mean=7.8 years, SD=1.1), when the children were between 9.4 and 17.2 years old (mean=13.2 years, SD=1.8).
Selective High-Risk Early Intervention Study
Participants.
All children were screened in reception and year one classes (the equivalent of prekindergarten and kindergarten) from eight schools in a deprived area of London (
20). Teachers and parents of 684 children 4–6 years old completed the conduct problems scale of the Strengths and Difficulties Questionnaire (
26) and a checklist of the DSM-IV oppositional defiant disorder items. Parent and teacher scores were summed. A total of 279 children (41%) met the cutoff, which was defined as a score ≥5 on the Strengths and Difficulties Questionnaire or having ≥10 DSM symptoms; of these, 109 took part in the randomized trial. Their mean antisocial behavior severity was above the 82nd percentile (
Table 1). Families allocated to parent training showed a moderate reduction in child antisocial behavior after treatment compared with controls (effect size=0.6 standard deviations).
Parenting intervention.
This was the Incredible Years basic videotape program, supplemented by sessions on how to read with the child, since poor literacy independently contributes to antisocial outcomes, and attendance at a group that includes education on how to improve child reading has been found to help engage parents (
19). Families attended a mean of 15 sessions, 55% of those offered. Many therapists were from the clinical trial; training and supervision procedures were the same.
Control intervention.
Control parents were offered a telephone helpline manned by the same staff, advising them on how to access regular services. Seven families contacted the helpline, and one attended a local clinic and received counseling. No child in either trial arm received psychotropic medication.
Follow-up.
Data for these analyses were collected 4.2–7.7 years after the intervention was completed (mean=5.8 years, SD=0.83), when the children were between 9.2 and 13.1 years old (mean=11.0 years, SD=0.90).
Pre- and Postintervention Childhood Measures
Participant characteristics were assessed by an interview that covered family structure and income, housing type, ethnicity, and parental education. Child antisocial behavior was assessed using the Parent Account of Child Symptoms (
27), a standard investigator-based interview. Further information on procedures and measures is provided in the online
data supplement.
Measures at Adolescent Follow-Up
Oppositional symptoms and diagnosis were assessed at follow-up using the Child and Adolescent Psychiatric Assessment (
28), a semistructured diagnostic interview with parents. Antisocial personality traits were assessed from parent reports on the Antisocial Process Screening Device (
29). Antisocial behavior was assessed using the conduct problems scale of the Strengths and Difficulties Questionnaire for parents and teachers (
23) and the Self-Report Delinquency instrument (
30). Reading was assessed using the Weschler Objective Reading Dimensions age-standardized score (
31), an investigator-administered reading assessment. Parent-child relationship quality was assessed by expressed emotion using the Five-Minute Speech Sample (
32), supervision through the Child and Adolescent Psychiatric Assessment interview (
28), and interaction quality through direct observation of 20 minutes of parent-adolescent interaction (
33).
Data Analysis
The power to detect a difference of 0.6 standard deviations at follow-up was 80% in the clinical trial and 89% in the community trial (p<0.05). Analyses tested the long-term effects of treatment on the primary and secondary outcome measures, using an intention-to-treat approach. The variables included in the prediction model on an a priori basis were preintervention antisocial behavior severity, sex, age, and group (treatment or control). Significant treatment differences between the trials were then examined as a statistical interaction between treatment exposure and trial type (indicated or selective). In supplementary analyses, multiple imputation (with 20 data sets) was used to account for potential biases associated with missing data. All analyses were based on generalized estimating equations to account for the nested structure of the data, based on maximum likelihood.
Results
Table 1 summarizes the family demographic and child behavior data in the initial trials and at follow-up. There were no initial within-sample differences by treatment group. However, between-sample differences were notable: on average, the indicated sample had more severe preintervention antisocial behavior (F=62.84, df=1, 228, p<0.001), more often lived in public housing (F=4.85, df=1, 225, p<0.05), were less often from an ethnic minority group (χ
2=4.24, df=1, p<0.05), were older (F=4.76, df=1, 224, p<0.05), and attended a higher percentage of treatment sessions offered (F=14.40, df=1, 144, p<0.01).
At follow-up, 93 members of the indicated sample (78%) were successfully assessed, as were 90 members of the high-risk sample (83%). Dropout was not significantly associated with any preintervention variable. Preliminary analyses indicated that socioeconomic indicators (ethnicity, maternal education, housing type), follow-up interval, and percentage of sessions attended did not reliably predict adolescent or parenting outcomes, so they were dropped from the main analyses.
Long-Term Effects in the Indicated Sample
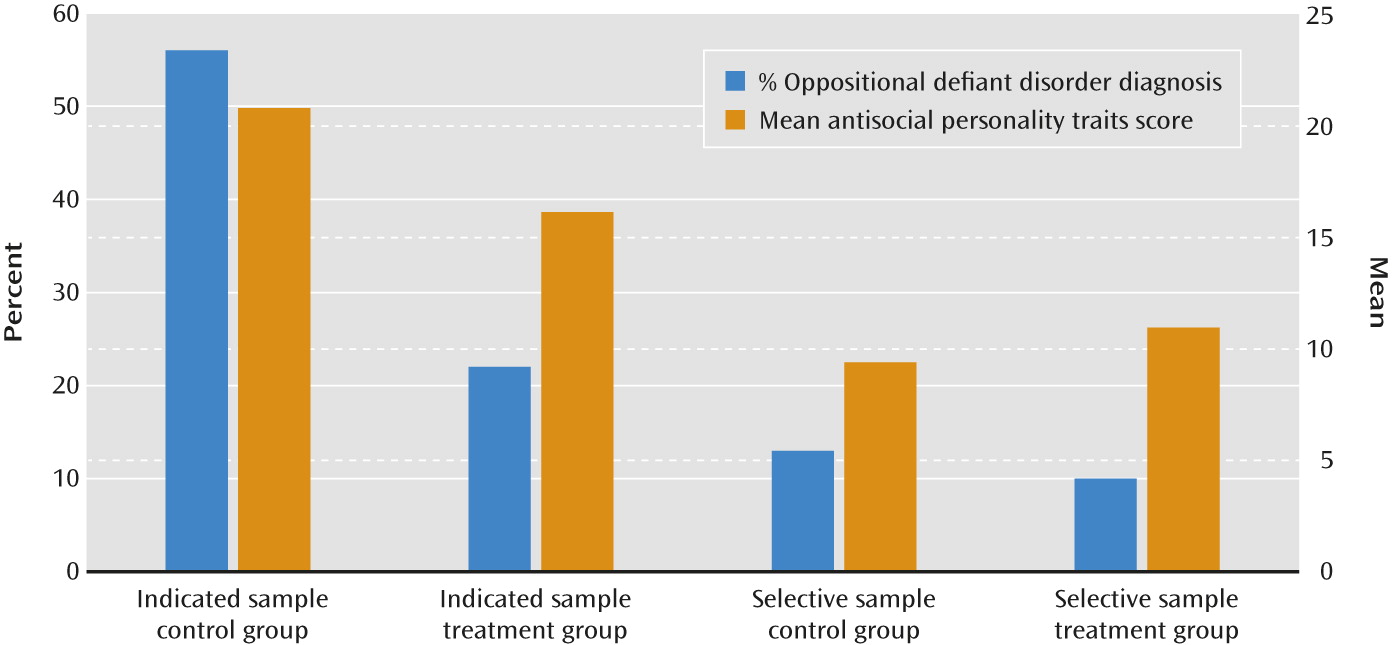
Treatment in early childhood was associated at follow-up in adolescence with improvement in both oppositional defiant symptoms and antisocial personality traits. Secondary outcomes also improved, with less parent-reported antisocial behavior, better reading (Tables 1 and 2), and improved parenting on two out of three measures (Table 3; see also Table S1 in the online data supplement). Effect sizes were medium to large: 0.91 for oppositional defiant symptoms, 0.70 for antisocial personality traits, and 0.42 for standardized reading achievement. Diagnosis rates of oppositional defiant disorder were considerably reduced (B=–1.61, SE=0.63; odds ratio=0.20, 95% CI=0.06, 0.69, p=0.01) (
Figure 1). Analyses using multiple imputation for missing values yielded similar results (see Table S2 in the
data supplement).
Compared with diagnostic interview and parent-reported questionnaires, the effects for teacher-reported conduct problems or adolescent self-reports of delinquent behavior at school or of substance misuse were weaker and nonsignificant (although a borderline significant effect on self-reported antisocial behavior was observed; see Table S1 in the
data supplement).
Long-Term Effects in the Selective High-Risk Sample
There were no significant long-term treatment effects on any adolescent or parenting outcome measure (Tables 1–3). Difference in Treatment Effects by Sample Type
The findings suggest stronger effects in the indicated compared with the selective high-risk sample. This was tested formally by rerunning the generalized estimating equations adding sample type (clinic, community) and sample-by-treatment interaction. The sample-by-treatment interaction was significant for each adolescent and parenting outcome listed in
Tables 2 and
3, with the intervention being significantly more effective for the indicated sample, including with imputed data (see Table S3 in the
data supplement). Supplementary analyses indicated that the study effect was not explained by initial severity of child antisocial behavior or demographic differences between the samples (see the
data supplement).
Discussion
In this study, we examined whether parent training for antisocial behavior in young children had persisting beneficial effects by preventing the development of antisocial personality in adolescence. In the sample with cases where treatment was clinically indicated, we observed improvements at long-term follow-up in both facets of antisocial personality, namely, antisocial behavior (with a large reduction in the odds of having oppositional defiant disorder) and antisocial character traits. Additionally, participants’ reading ability was substantially improved on a standardized assessment, and the parents expressed greater emotional warmth and supervised their adolescents more closely, although effects were not found in directly observed parenting behavior. Teacher report and adolescent self-report did not show significant differences. These findings are encouraging, as they suggest that important aspects of the life trajectories and adjustment of these individuals were improved by a comparatively modest intervention occurring in early childhood, despite notably poor early disturbance and risk exposure.
In contrast, in the sample of children with high levels of risk selectively recruited from the community, we found no sustained improvements from parent training on antisocial behavior, character traits, or reading ability; nor were persisting effects detected in the parent-child relationship. The difference in findings between the two studies was statistically significant. Further analyses showed that the difference was not reliably explained by child or family characteristics.
Strengths of both studies included the use of multimethod, multi-informant measures with high-quality, investigator-rated semistructured interviews for the primary outcome measures, and teacher report, adolescent report, independent testing, and direct observation of parent-adolescent relationship quality for the secondary outcome measures. Both studies had good retention rates (78% and 83%), especially considering the mean interval of 7 years between intervention and follow-up assessment and the difficulty tracing and engaging disadvantaged families with antisocial children. Families were included whether or not they had engaged in the intervention, an intention-to-treat analysis strategy. A proven parenting program was delivered to a high standard with good short-term outcomes, making it more likely that if there were long-term effects, they would be detected. The populations were representative of real-life conditions, as recommended by CONSORT criteria for pragmatic trials (
34). Thus, in the indicated sample, participants were routine referrals, and intervention staff were employed by local services; in the selective high-risk sample, the initial screen covered 99% of the population, and 65% of parents approached took part. Adding to validity, the intervention and research teams were independent of the program developer, which is important, as positive trial results from commercial developers have not always been replicated by others (
35).
The study had some limitations. The clinic sample had relatively small numbers in the control arm, making it prone to type II (false-negative) errors, although it nonetheless had adequate statistical power. Both trials only enrolled children whose parents were prepared to engage in treatment, so the findings may not be applicable to families who are reluctant to engage.
A further issue is whether the gains observed in the indicated sample might be due to parental bias. This does not seem likely, however, for several reasons. First, the research staff conducting clinical interviews were blind to treatment condition and quite separate from the intervention staff. Moreover, several years had elapsed, so it is unlikely that parents would have wished to please the research team. Second, the primary outcome measure was assessed with a semistructured interview, in which the investigator takes considerable trouble to elicit detailed examples and then makes the ratings independently of the informant. Semistructured interviews are the cornerstone of psychiatry and are widely used as the main outcome measure in treatment trials because they are less prone to biases than questionnaire methods. Their validity has been widely established, and they predict numerous poor outcomes (
36,
37). Third, other measures that were independent of parental bias—ratings of expressed emotion and psychometric testing of youths—showed a significant difference between intervention and control groups. Finally, in the selective high-risk sample, no difference was found between intervention and control groups using the same interview and interviewers; any methodological bias toward favoring treatment would be expected to affect both trials.
The gains in the indicated group are plausible and are consistent with the mechanism of action of the intervention. Personality traits are likely to be more malleable in younger children, when the ability to feel empathy is still developing (
38) and brain development shows more plasticity (
39); more supportive parenting is associated with increased brain growth in areas related to emotion processing (
40). Change toward more empathetic responding requires repeated experience of more sensitive primary caring relationships, which may be internalized and underlie positive behavior (
41); persisting differences in parental expressed warmth were observed in the treated group. Regarding youth antisocial behavior, in keeping with social learning theory (
42), change was seen in the domain where the parents could directly influence the contingencies around the adolescent (i.e., at home), but not where they had less influence (in the community and at school). That may account for why no evidence in teacher-reported antisocial behavior was found, a finding confirmed in meta-analyses of short-term effects of parenting interventions (
14). The improvement in reading was not directly targeted in the intervention delivered to the clinic sample, but this effect is compatible with recent studies showing that parent training can lead to reading improvements (
20) and that there is a close link between antisocial behavior and reading problems in development (
20).
In contrast, the failure of the selective sampling strategy to have enduring effects despite good gains in the short term in childhood was disappointing. The lack of a long-term difference may be due, first, to the size of the initial short-term treatment effect, which was half as large as that observed in the clinic sample (0.6 compared with 1.1 standard deviations). Second, parents may not have felt so motivated to continue to work on their child’s behavior, since it was less problematic at the outset and since they were not seeking treatment when recruited. This explanation is supported by their attending a lower percentage of offered sessions than did the clinic group (although the total number was greater, since more were offered). Third, unlike the children in clinic control group, who remained seriously antisocial, those in the community control group showed regression to the population mean (ending on the 60th percentile), a phenomenon commonly seen in community-wide surveys. The level of antisocial behavior within individuals in the general population naturally waxes and wanes, so that choosing a high cutoff may select individuals at a high point in their cycle, which is likely to be followed by a reduction over time.
This study has important implications for patient care. For children at high risk of poor outcomes, high-quality parent training programs should be offered not only because they ameliorate disruptive behavior in the short term, but also because they may prevent later personality problems and associated impairment. As the children become adolescents, parents could be offered booster courses to address new developmental challenges and improve behavior in the community—for example, by monitoring the whereabouts of their child when out of the house, negotiating rules about alcohol, and enforcing sanctions for misbehavior; programs addressing these issues are effective (
14). To improve later antisocial behavior at school, teacher classroom management programs could be introduced, since they have a growing evidence base (
43).
The study also carries implications for public health policy. The findings provide the first evidence that parent training for young children with clinical-level antisocial behavior may reduce the poor outcomes and high cost of later antisocial personality, thus supporting the recommendations of NICE and other bodies concerned by the “epidemic” of youth violence (
2,
7,
39). Whether parent training should be recommended as a selective long-term prevention policy for children with milder problems is less clear. The findings here are broadly in keeping with the two post hoc analyses described in the introduction (
15,
19), which found that early intervention effects may not be enduring for less symptomatic and at-risk children. Thus, the selective Fast Track trial (
15) found no overall long-term effects, but the most severe cases initially did seem to improve.
Nonetheless, the short-term gains in the selective high-risk sample described here were substantial; the lack of a significant persisting effect in this case does not necessarily imply that selective early intervention should be abandoned. In physical medicine, many drugs have effects lasting only for a short time—for example, in asthma or diabetes treatment—but are nonetheless considered effective. In other areas of mental health, such as depression, relapse prevention treatment following initial treatment has proven effective; this approach may be applicable to child antisocial behavior and personality, where a “dental care model” could be applied, in which children have regular checkups, with further intervention as appropriate. Further research is needed to replicate the findings, test the effectiveness of later booster interventions, and examine whether benefits persist into adulthood.