The Affordable Care Act authorized $1.5 billion over 5 years for the Maternal, Infant, and Early Childhood Home Visiting Program, legislated on March 23, 2010. Funding is prioritized for state-level dissemination of evidence-based home-visiting programs to support the health and development of at-risk children, with 3% set aside for tribal communities (
1).
Several gaps in the evidence base for home-visiting programs threaten the potential public health impact of the Maternal, Infant, and Early Childhood Home Visiting Program (
2). First, current home-visiting programs have not been evaluated in low-resource special populations in the United States, including American Indian, new immigrant, and military families (
2,
3)—populations that can be difficult to recruit and retain (
3). Second, no home-visiting program currently endorsed by the Maternal, Infant, and Early Childhood Home Visiting Program (
3,
4) has been designed to target or shown reductions in both maternal drug use and mental health problems known to negatively affect children’s early development (
5–
8) and disproportionately affect mothers in at-risk settings. Third, current home-visiting interventions have not systematically measured intervention impact on children’s emotional and behavior outcomes across early childhood (0 to 3 years) that are known to predict better developmental trajectories across the life course (
9,
10). Identification of early benefit is critical, given the short grant cycle of the Maternal, Infant, and Early Childhood Home Visiting Program and the need for early markers to indicate positive return on investment. Fourth, the most rigorously evaluated home-visiting programs do not lend themselves to replication in at-risk communities. For example, some interventions require nurse home visitors (
11), despite the shortage of nurses in low-resource, culturally diverse communities. Further, reports on home-visiting trials have not included methods or outcomes of intervention fidelity (
2). Ensuring intervention fidelity is critical to scaling efforts. Finally, trials that have depended on assessments that employ high-cost professionals or technologies (i.e., direct or videotaped observational assessments) or extended periods of follow-up to identify benefit are often not feasible within disadvantaged populations, such as those targeted by the Maternal, Infant, and Early Childhood Home Visiting Program.
To address these gaps, the Family Spirit intervention (
12–
14) is to our knowledge the first in the home-visiting literature to be designed to address behavioral health disparities of the poorest and most underserved population in the United States (
15–
17), American Indians, and to be evaluated by using state-of-the-science measures of intervention fidelity and early childhood emotional and behavioral development. The intervention targeted American Indian adolescents—who have the highest rates of teen pregnancy, substance use, suicide, and dropping out of school of any racial or ethnic group in the country. Because of a shortage of nurses and the community preference for indigenous home visitors (
14), bilingual paraprofessional home visitors from the participating communities were employed and trained to intervention mastery. The existing literature suggests paraprofessional home visitors have influenced some specific outcomes, such as birth outcomes, but have not achieved the broad-based effects on maternal and child health and behavior outcomes that nurse home visitors have (
18,
19). Similarly, a Cochrane report examining global evidence for paraprofessional-delivered interventions concluded that while paraprofessionals were effective in specific domains, i.e., immunization uptake and health promotion to prevent acute respiratory infection and malaria, there was yet insufficient evidence to promote paraprofessional practice or policy in other behavioral or mental health domains (
20).
The Family Spirit intervention has been evaluated in two shorter, smaller trials with positive maternal outcomes at 6 and 12 months and positive child outcomes at 12 months (
12,
13). The aims of this trial were to evaluate the intervention’s effects on parental competence (parenting knowledge, locus of control, stress, and behaviors) and maternal behavioral problems that impede effective parenting through early childhood (0 to 36 months postpartum). Secondary aims were to evaluate intervention effects on early childhood emotional and behavioral outcomes. This trial’s 12-month outcomes were published previously (
14). Here we report results through the final study period, to 36 months postpartum.
Method
Study Design
A multisite, randomized (1:1), parallel-group trial was conducted to assess the efficacy of the Family Spirit intervention for parenting and for maternal and child emotional and behavioral outcomes from 32 weeks gestation to 36 months postpartum. Participants were randomly assigned to receive either the Family Spirit intervention plus optimized standard care or optimized standard care alone. Detailed study methods have been published previously (
14). Relevant tribal, Indian Health Service, and Johns Hopkins University research review boards approved the trial. An independent data safety and monitoring board maintained oversight of participant safety.
Participants
Eligible participants were expectant American Indian teens (ages 12–19 years at conception) at no more than 32 weeks gestation from four southwestern reservation communities. Prospective participants were excluded if they were currently participating in other mental or behavioral research or if life circumstances precluded full participation in the intervention protocol, such as severe mental illness or legal status that required high-intensity residential care. Participants were recruited from Indian Health Service clinics, Women, Infants, and Children nutrition programs, and schools and by word of mouth. Potential participants were screened for inclusion and were given a complete description of the study. Research staff obtained assent and parent or guardian consent from participants younger than 18 years and consent from participants who were 18 or older.
The study sites were rural reservation communities with populations of 15,000–25,000, including the White Mountain Apache and San Carlos Apache Reservations in eastern Arizona and the Tuba City and Fort Defiance communities on the Navajo Reservation in northern Arizona.
Interventions
The Family Spirit Intervention was developed over a decade through community-based participatory research (
12). The intervention content included 43 structured lessons and followed a culturally congruent format (
14). Positive parenting lessons were focused on reducing behaviors (i.e., poor monitoring; coercive interactions; harsh, unresponsive, or rejecting parenting; and abuse/neglect) associated with early childhood behavior problems, including externalizing, internalizing, and dysregulation problems (
21–
23). Additional content addressed maternal behavior and mental health problems that impede positive parenting, including substance use and externalizing and internalizing behaviors (
13). The Family Spirit interventionists, referred to as family health educators (or educators), were required to have a minimum of a high school diploma or GED, at least 2 years of additional job-related education or work experience, and the ability to speak their Native language and English. They delivered lessons one-on-one in the participants’ homes, using highly illustrated tabletop flip charts. Each home visit was designed to last no more than 1 hour, and it included a warm-up conversation, lesson content, a question-and-answer period, and summary handouts. Visits occurred weekly through the third trimester of pregnancy, biweekly until 4 months postpartum, monthly between 4 and 12 months postpartum, and bimonthly between 12 and 36 months postpartum (
14).
Several strategies were implemented to maintain intervention fidelity: 1) educators had to score at least 80% on Family Spirit content quizzes before administering lessons, 2) study coordinators, who did not deliver the intervention, reviewed the educators’ session summary forms for visit duration, lessons completed, and other issues addressed, 3) study coordinators rated a random 20% of audio-recorded lessons for quality and adherence to intervention protocol, and 4) study coordinators conducted in-person quarterly ratings of home visits for protocol adherence.
Optimized standard care consisted of transportation to recommended prenatal and well-baby clinic visits, pamphlets about child care and community resources, and referrals to local services. It also addressed access barriers to health care for young mothers and children, and it overcame concerns that home-visiting programs have operated in parallel, not in partnership, with pediatric care (
24). Family health liaisons conducted the optimized standard care and were not trained in the Family Spirit intervention, to avoid contamination of the control condition.
Outcomes
Intervention impact was assessed in three domains: 1) parental competence, 2) maternal emotional and behavioral outcomes, and 3) children’s emotional and behavioral outcomes at nine time points: approximately 28 to 32 weeks gestation (baseline), 36 weeks gestation, and 2, 6, 12, 18, 24, 30, and 36 months postpartum. Study assessments were selected for their wide use, strong psychometric properties, cross-cultural validity, and low cost and feasibility for implementation and dissemination in low-resource communities. Assessments are described below with accompanying Cronbach’s alpha scores averaged across all time points.
Parental competence.
Parenting knowledge was assessed by using a 30-item maternal self-report we created to measure knowledge gains (mean alpha=0.58; baseline, 12, 24, and 36 months). Parenting locus of control was measured with a 27-item maternal self-report of three domains: parent self-efficacy, parent control, and child control (mean alpha=0.84; 2, 6, 12, 18, 24, 30, 36 months) (
25). Parenting-related stress was measured by means of the Parenting Stress Index–Short Form, a 36-item maternal self-report instrument (mean alpha=0.94; 24 and 36 months) (
26).
The home environment was also assessed, with the Home Observational Measure of the Environment (HOME), a 37-item observational measure completed by an independent evaluator. Separate ratings were made for parental behavior, parent-child interaction, and home environment; the maternal acceptance subscale was omitted owing to concerns regarding cultural appropriateness (mean alpha=0.73; 6, 12, 18, 24, 30, 36 months) (
27).
Maternal emotional and behavioral functioning.
The Center for Epidemiological Studies—Depression scale (CES-D) is a 20-item self-report and was used to assess maternal depressive symptoms (mean alpha=0.84; baseline, 36 weeks gestation, 2, 6, 12, 18, 24, 30, 36 months) (
28). The Achenbach System of Empirically Based Assessments youth self-report is a 112-item scale, and it was used to evaluate externalizing problems (opposition/defiance, rule breaking, and social problems), internalizing problems (anxious/depressed/withdrawn, thought problems), and total problems (mean alpha=0.90; baseline, 6, 12, 18, 24, 30, 36 months) (
29).
The drug use subscale of the Voices for Indian Teens, a culturally specific self-report instrument, was used to measure the quantity and frequency of alcohol and drug use (mean alpha=0.73; baseline, 2, 6, 12, 18, 24, 30, 36 months) (
30).
Children’s emotional and behavioral outcome.
The Infant-Toddler Social and Emotional Assessment is a 126-item parental report. It measures children’s externalizing behaviors (activity/impulsivity, defiance/aggression), internalizing behaviors (distress/anxiety, inhibition/withdrawal), dysregulation (of sleeping, eating, emotions, sensory experiences), and competence (in attention, compliance, imitation/play, motivation, empathy) (externalizing behaviors, mean alpha=0.84; internalizing behaviors, mean alpha=0.80; dysregulation, mean alpha=0.89; competence, mean alpha=0.89; 12, 18, 24, 30, 36 months). These outcomes are presented both as means and as proportions of participants whose scores were clinically “of concern,” i.e., ≤10th percentile (
31).
Sample Size
The primary outcome for determining sample size and power was the HOME (
27). With 322 participants and an assumption of 25% attrition, alpha=0.05, within-family correlation of r=0.5, and assessment completion rate of four out of the six time points when the HOME was to be administered, the study had 90% power to detect a meaningful public health effect size of 0.33 (
32).
Randomization and Blinding
The data manager created the randomization sequence by using Stata 9.0 (StataCorp, College Station, Tex., 2005). Participants were stratified by site, age (12–15 and 16–19 years), and parity (0 and ≥1) and randomized with a 1:1 allocation in blocks of four into two study arms: Family Spirit plus optimized standard care or optimized standard care alone. After enrollment, the paraprofessional family health liaisons telephoned the study coordinator to receive each participant’s randomization status. Neither the liaisons, who implemented the optimized standard care condition and self-report assessments, nor the family health educators, who implemented the Family Spirit intervention, were blind to randomization status. Independent evaluators, who administered the Infant-Toddler Social and Emotional Assessment and the HOME, were blind to randomization status.
Statistical Methods
Repeated-measures analyses of covariance (ANCOVAs) were employed to test for hypothesized intervention effects (differences between the intervention and control groups in means for continuous outcomes and in odds ratios for dichotomous outcomes) across the postpartum assessment period (i.e., the main effect of intervention condition in the ANCOVA model). In addition, effect sizes were computed for continuous outcomes; effect sizes were calculated as the estimated group mean difference divided by the square root of the residual covariance estimate. All postpartum assessment points for a given outcome were included in the analysis.
Assessments gathered between 28 and 32 weeks gestation represented baseline values. For the CES-D, the baseline value was the average of scores from the first two time points (i.e., <32 weeks and approximately 36 weeks gestation) to generate a more accurate estimate of depressive symptoms during pregnancy. If the outcome measure was collected at baseline, its value was included in the analysis as a covariate. Other covariates included the mother’s age, the sex and age of the child (in months) at the time of assessment (for child outcomes) to adjust for differences between nominal and actual assessment points, and three variables to control for nonequivalence (0.05<p<0.1) between study groups at baseline: maternal depressive symptoms during pregnancy, lifetime cigarette use, and alcohol or illegal drug use during pregnancy. The inclusion of relevant covariates also serves to increase statistical power for hypothesis tests by reducing unexplained (error) variance in the models. Factors in the ANCOVA models included study condition, site, and assessment wave.
Analyses were intent-to-treat; all randomly assigned participants were included. Analyses of continuous outcomes were conducted by using SAS PROC MIXED; SAS PROC GLIMMIX was used for dichotomous outcomes. The covariance structure specified for the repeated-measures analysis was banded Toeplitz (
33,
34)—three bands for continuous outcomes and two bands for dichotomous outcomes (to facilitate model convergence) and for the Parental Stress Index, which included only two postpartum assessments. The banded Toeplitz structure was selected to parsimoniously model the cross-wave covariation expected in the repeated measures. Consistent with current recommendations (
35,
36), missing data were addressed through the application of maximum likelihood estimation (restricted maximum likelihood for continuous outcomes and restricted pseudo likelihood for dichotomous outcomes). In addition, ANCOVA models were employed to examine potential differential attrition associated with baseline outcome and covariate measures.
Results
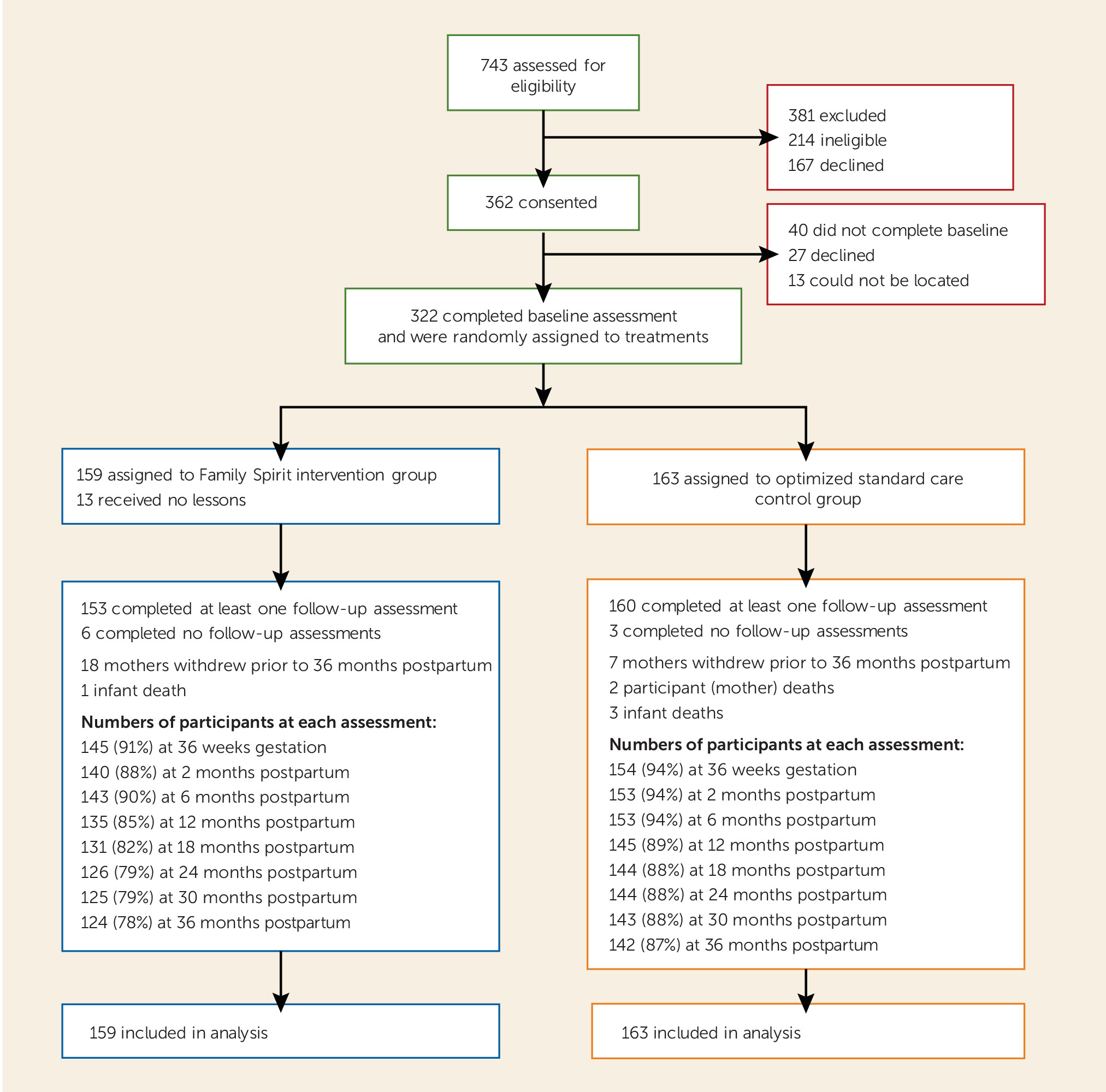
Of 743 women assessed for eligibility, 381 were excluded (214 were ineligible and 167 declined to participate) and 362 consented to participation. Of these, 322 completed baseline assessments and were randomly assigned between 2006 and 2008 (
Figure 1). Within the intervention group, 13 received no Family Spirit lessons. Two mothers (both in the control group) and four infants (intervention, N=1; control, N=3) died during the trial. Twenty-five mothers (intervention, N=18; control, N=7) withdrew during the study period. Wave-specific participation rates for postpartum assessments ranged from 92% at 6 months postpartum (N=296; intervention, N=143; control, N=153) to 83% at 36 months postpartum (N=266; intervention, N=124; control, N=142).
Baseline Characteristics
As shown in
Table 1, the participants were on average 18.1 years old and were predominantly primiparous, unmarried, and residentially unstable. They had a high lifetime rate of substance use, and one-third had a high level of depressive symptoms. The two treatment groups were similar at baseline, with the exception of three variables that were more common in the intervention group (0.05>p≤0.1): maternal depressive symptoms, use of alcohol during pregnancy, and lifetime cigarette use.
Attrition was higher in the intervention group than in the control group. Attrition in both conditions primarily occurred before 12 months, followed by relatively stable participation through 36 months. Analyses of differential attrition showed significant effects for two variables. Women in the intervention group who reported no substance use during pregnancy were more likely to drop out, and participants in the control group who reported never using cigarettes were more likely to remain in the study. Attrition did not favor the intervention group.
Intervention Fidelity
Three-quarters (74.2%) of the participants in the intervention group completed more than 50% of the Family Spirit lessons by 12 months postpartum, and 69.8% and 66.7% did so at 24 and 36 months postpartum, respectively. Intervention lessons were completed as planned for 85% of the visits. The average time for lesson visits was 52 minutes.
Parenting Outcomes
As shown in
Table 2, across the study period the mothers in the intervention group had significantly more parenting knowledge and parental locus of control. The difference was not significant at p<0.05 for parenting stress or observations of the home environment.
Maternal Outcomes
As shown in
Table 3, across the study period the mothers in the intervention group had significantly lower scores for depression and externalizing problems. No between-group differences were seen in the score for internalizing problems or the total score on the Achenbach youth self-report measure. Mothers in the intervention group had lower use in the past month of marijuana and illicit drugs (
Table 3). No between-group differences were observed for alcohol use.
Child Outcomes
As shown in
Table 4, children in the intervention group had lower scores for externalizing problems, internalizing problems, and dysregulation from 12 to 36 months. Fewer children in the intervention group scored in the “of concern” range (≤10th percentile) for externalizing and internalizing problems (
Table 4).
Discussion
This study demonstrated the effectiveness of a paraprofessional-delivered home-visiting intervention for American Indian teen mothers’ parenting, externalizing problems, depression, and substance use and for their children’s early emotional and behavioral outcomes from infancy through 36 months postpartum. Findings from previous trials were replicated and extended (
12–
14). Despite an active control group that connected participants to recommended prenatal and pediatric care, effect sizes were similar in magnitude to those of community-based interventions with recognized public health impact (see reference
32).
Strengths
This study makes several important contributions to gaps (
2–
4) in the current home-visiting field and to the preventive care and public health literature more generally: 1) the intervention was effective in reducing maternal and child behavior health disparities in the most disadvantaged and hard-to-reach and -retain U.S. subgroup (
2,
15,
16); 2) assessment measures identified short-term (12-month) and longer-term (up to 36 month) maternal and child behavioral outcomes and included measures of intervention fidelity—both lacking from previous home-visiting trials; and 3) the trial demonstrated the effectiveness of community-based paraprofessionals as behavioral interventionists—a finding that is increasingly critical for populations with a shortage of nurses or professional health care providers and persistent behavioral and mental health disparities.
The intervention’s dual focus on competent parenting and mothers’ behavioral and mental health risks that impede competent parenting is likely critical to the success of home-visiting programs in communities that suffer intergenerational behavioral health disparities. To this point, relative to mothers in the control group, mothers receiving the Family Spirit intervention had better parenting knowledge and self-efficacy, while showing fewer externalizing problems and less depression and substance use—maternal behaviors that have been linked to negative parenting practices that predict child behavior problems over the life course (
5–
8). Meanwhile, children in the intervention group benefited in three developmental domains (externalizing, internalizing, and dysregulation problems) that predict better behavior outcomes in later childhood and adolescence (
9,
10); also, a smaller proportion of children in the intervention group scored in the “of concern” range for externalizing and internalizing problems. Moreover, these maternal and child effects were apparent despite baseline group differences, notably maternal depression, that might be expected to reduce response to intervention efforts. Of public health importance for the participating communities, children in the control condition—in spite of receiving optimized pediatric care—had considerably more “of concern” levels of externalizing (23.8%), internalizing (14.6%), and dysregulation (14.6%) problems than the normative sample for these measures (<10%) (
31). Given the known risks of early childhood externalizing, internalizing, and dysregulation behaviors for later childhood substance abuse, educational attainment, and obesity (
9,
10,
37), this research has implications for reductions in health, education, and mental health problems across the life course. In light of the increasing global burden of behavior-related noncommunicable disease, efforts to scale interventions of the Family Spirit type in high-risk communities deserve the attention of scientists and policymakers alike. Further, according to prior evidence regarding return on investment from nurse home-visiting programs relative to health care and welfare cost savings (
38,
39), paraprofessional home visitors, who are more affordable than nurses, could lower health and human service costs, build the capacity of the local work force, and better match consumer preferences for culturally competent providers in high-risk settings.
Home Environment
This study did not find differences in ratings from home observations. Other home-visiting studies have not identified differences until 2 to 4 years postpartum (
11,
40). Our lack of findings may be related to a lag in this indicator, the fact that the mothers were highly mobile and unable to establish a stable home environment for their children, or the lack of cultural congruity in several items of the measure, described previously (
13,
41).
Limitations
The trial had several potential limitations, including concerns regarding generalizability, response bias with self-report measures, and the large number of study outcomes. In terms of generalizability, the intervention was designed to address the poorest, most at-risk communities in the country. All sites shared substantial behavioral health and sociodemographic disparities similar to or exceeding those of other at-risk communities in the United States and worldwide, but they were diverse in language, culture, and exposure to dominant society norms.
Self- and parent-report measures of maternal and child behavior outcomes from 0 to 3 years postpartum facilitated detection of early intervention benefit and allowed for paraprofessional administration. However, response bias is a concern for maternal self- and parent-report measures. Some of the mothers’ self-report scores (i.e., on the Achenbach youth self report) were better than or comparable to those for U.S. all-race samples (
29) despite the mothers’ early pregnancy, drug use, and challenging living conditions. On the other hand, mothers in both groups reported high rates of depression and substance use, sensitive indicators for under-age respondents, and high rates of “of concern” scores for their infants and toddlers. Other types of assessments, such as biological samples (e.g., cotinine or urine samples) or videotaped and coded observational measures, were not culturally acceptable or financially feasible in this trial. Low-cost, sensitive standardized self-reports can facilitate dissemination and real-time effectiveness monitoring as home-visiting programs are implemented at scale in community settings.
Finally, because of the large number of dependent variables, the likelihood that some significant findings could be due to chance was increased. However, the majority of outcomes showed significant differences, were consistent with the study’s theoretical model and hypotheses (
14), and replicated and extended findings from previous Family Spirit evaluations (
12,
13,
41).