Pediatric-Onset and Adult-Onset Separation Anxiety Disorder Across Countries in the World Mental Health Survey
Abstract
Objective:
Method:
Results:
Conclusions:
Method
Samples
Measures
Overview.
Diagnostic assessment.
Sociodemographic variables.
Functional Impairment.
Childhood family adversities.
Traumatic events.
Analysis Procedures
Results
Prevalence
| Country and Country Income | Lifetime Prevalence | 12-Month Prevalence | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | Total | Male | Female | Sample Size (N) | ||||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | Male | Female | |
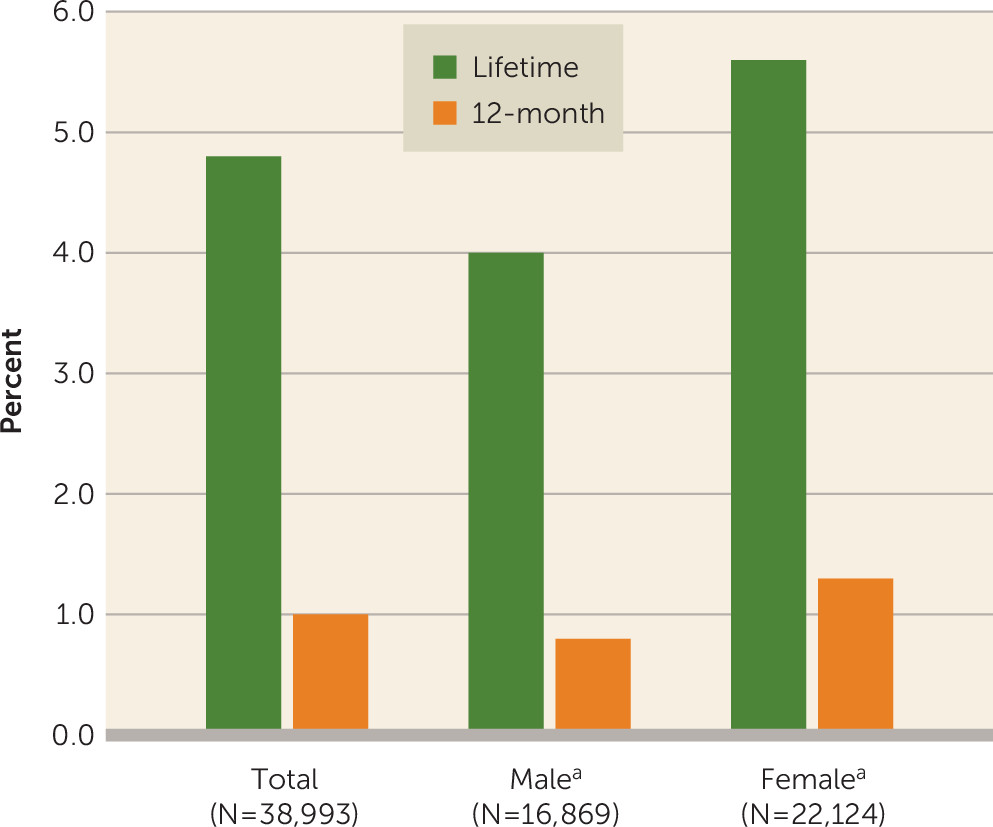
| All countries | 4.8 | 0.1 | 4.0 | 0.2 | 5.6* | 0.2 | 1.0 | 0.1 | 0.8 | 0.1 | 1.3* | 0.1 | 16,869 | 22,124 |
| Low-/lower-middle income | 5.5 | 0.4 | 4.5 | 0.4 | 6.4* | 0.5 | 1.3 | 0.2 | 0.9 | 0.2 | 1.7 | 0.4 | 2,622 | 3,472 |
| Colombia | 9.8 | 0.8 | 8.1 | 1.1 | 11.3* | 1.2 | 2.7 | 0.5 | 1.9 | 0.5 | 3.3 | 0.9 | 885 | 1,496 |
| Nigeria | 0.2 | 0.1 | 0.2 | 0.1 | 0.2 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 614 | 675 |
| People’s Republic of China-Beijing/Shanghai | 1.3 | 0.5 | 0.7 | 0.4 | 2.1 | 1.0 | 0.2 | 0.1 | 0.0 | 0.0 | 0.4 | 0.2 | 326 | 297 |
| Peru | 6.1 | 0.7 | 5.6 | 0.8 | 6.6 | 0.9 | 1.2 | 0.2 | 0.9 | 0.2 | 1.4 | 0.3 | 797 | 1,004 |
| Upper-middle income | 4.7 | 0.2 | 4.0 | 0.3 | 5.3* | 0.3 | 1.2 | 0.1 | 1.0 | 0.2 | 1.4 | 0.2 | 5,334 | 7,271 |
| Brazil | 7.7 | 0.4 | 6.7 | 0.6 | 8.6* | 0.6 | 2.0 | 0.3 | 1.7 | 0.4 | 2.3 | 0.3 | 2,187 | 2,850 |
| Bulgaria | 1.4 | 0.4 | 1.5 | 0.8 | 1.2 | 0.3 | 0.4 | 0.3 | 0.6 | 0.5 | 0.2 | 0.1 | 951 | 1,282 |
| Lebanon | 6.9 | 1.3 | 4.9 | 1.5 | 9.0 | 1.8 | 1.9 | 0.5 | 1.1 | 0.5 | 2.7 | 0.8 | 251 | 365 |
| Mexico | 4.5 | 0.4 | 3.7 | 0.8 | 5.2 | 0.5 | 0.9 | 0.2 | 0.7 | 0.2 | 1.1 | 0.2 | 853 | 1,509 |
| Romania | 0.9 | 0.3 | 0.9 | 0.4 | 0.9 | 0.3 | 0.3 | 0.1 | 0.2 | 0.1 | 0.3 | 0.2 | 1,092 | 1,265 |
| High-income | 4.7 | 0.2 | 3.7 | 0.2 | 5.6* | 0.3 | 0.9 | 0.1 | 0.7 | 0.1 | 1.0 | 0.1 | 8,913 | 11,381 |
| Belgium | 1.4 | 0.3 | 0.7 | 0.3 | 2.1* | 0.4 | 0.1 | 0.1 | 0.0 | 0.0 | 0.3 | 0.2 | 599 | 591 |
| France | 3.5 | 0.5 | 3.1 | 0.7 | 3.9 | 1.0 | 0.9 | 0.3 | 0.4 | 0.2 | 1.4 | 0.7 | 692 | 772 |
| Germany | 2.0 | 0.4 | 1.5 | 0.4 | 2.6 | 0.6 | 0.4 | 0.2 | 0.5 | 0.3 | 0.4 | 0.3 | 806 | 912 |
| Italy | 1.5 | 0.4 | 0.6 | 0.3 | 2.3* | 0.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.1 | 1,171 | 1,209 |
| The Netherlands | 3.0 | 0.6 | 2.0 | 0.8 | 4.0 | 1.1 | 0.6 | 0.3 | 0.5 | 0.3 | 0.7 | 0.6 | 472 | 637 |
| Northern Ireland | 5.1 | 0.5 | 5.1 | 0.8 | 5.2 | 0.6 | 0.4 | 0.1 | 0.5 | 0.2 | 0.4 | 0.1 | 822 | 1,164 |
| Portugal | 6.4 | 0.8 | 5.7 | 1.5 | 7.2 | 0.7 | 1.2 | 0.3 | 0.8 | 0.4 | 1.5 | 0.4 | 759 | 1,301 |
| Spain | 1.2 | 0.3 | 1.1 | 0.4 | 1.4 | 0.4 | 0.3 | 0.1 | 0.1 | 0.1 | 0.4 | 0.2 | 1,210 | 1,485 |
| United States | 9.2 | 0.4 | 7.4 | 0.5 | 10.8* | 0.6 | 1.9 | 0.2 | 1.7 | 0.3 | 2.1 | 0.2 | 2,382 | 3,310 |
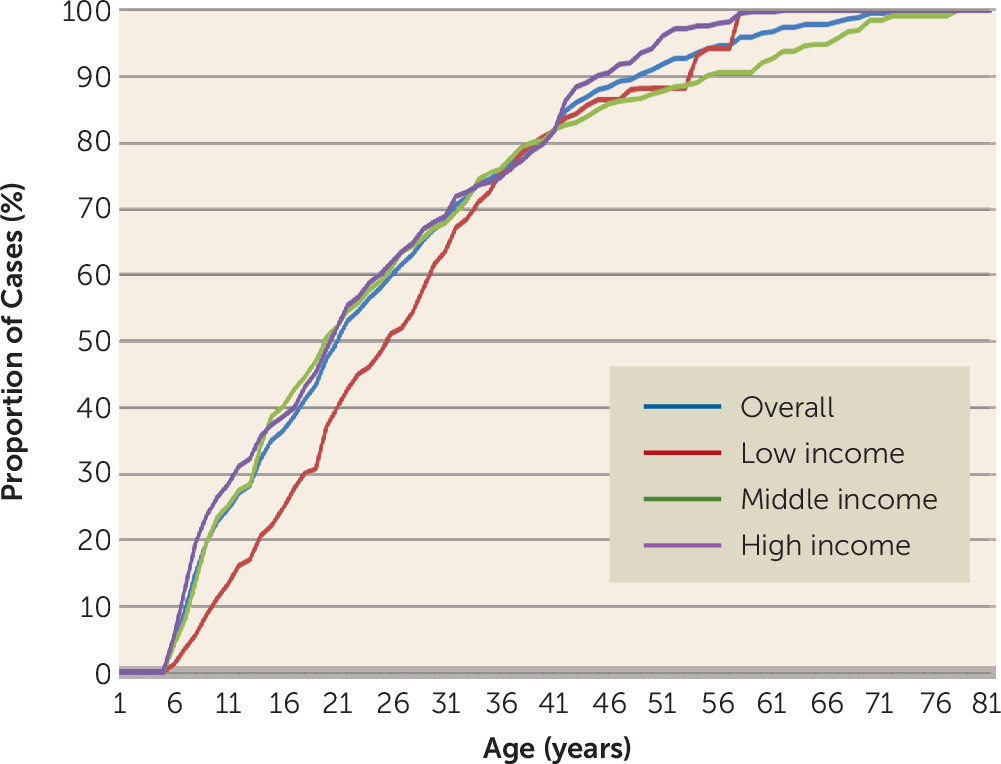
Age at Onset
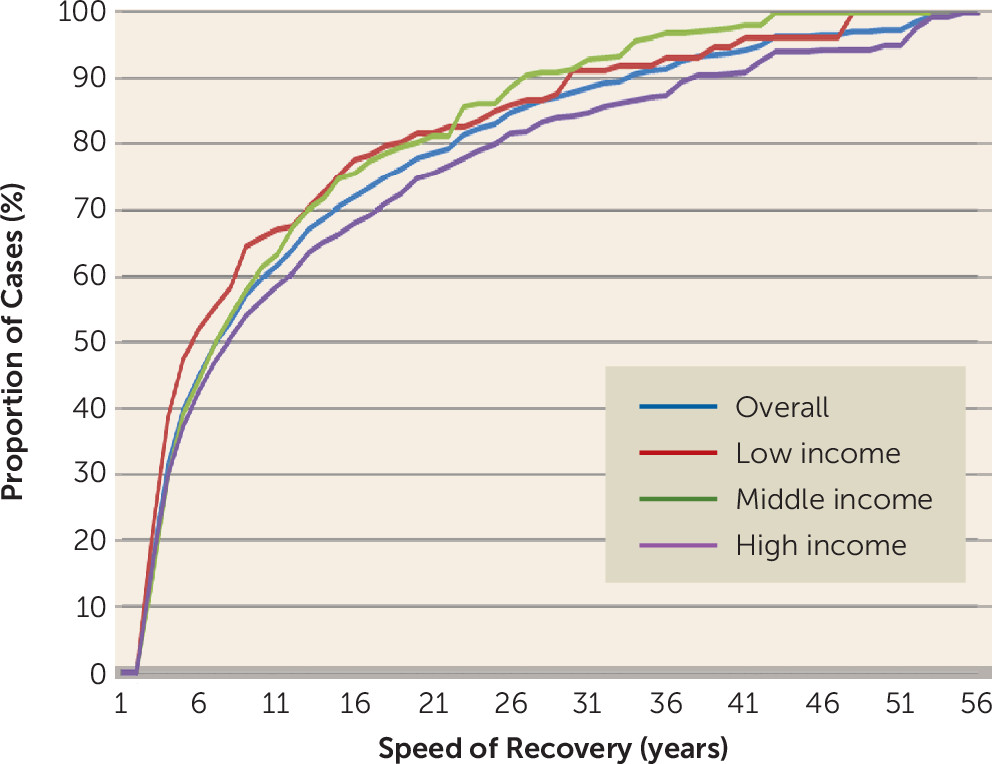
Persistence
| Disorder | Temporally Primary Separation Anxiety Disorder Predicting Subsequent Onset and Persistence of Other Disorders | Temporally Primary Other Disorders Predicting Subsequent Onset and Persistence of Separation Anxiety Disorder | ||||||
|---|---|---|---|---|---|---|---|---|
| Onseta | Persistenceb | Onsetc | Persistenced | |||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Internalizing | ||||||||
| Major depressive disorder | 1.4* | 1.3–1.6 | 1.3* | 1.1–1.7 | 1.7* | 1.4–2.0 | 1.4 | 0.9–2.1 |
| Bipolar disorder | 1.8* | 1.4–2.3 | 1.3 | 0.8–2.2 | 1.9* | 1.4–2.4 | 1.6 | 0.9–2.7 |
| Panic disorder without agoraphobia | 1.3* | 1.0–1.7 | 1.0 | 0.6–1.8 | 1.8* | 1.4–2.2 | 1.4 | 0.8–2.5 |
| Generalized anxiety disorder | 1.5* | 1.2–1.9 | 1.4 | 1.0–1.9 | 1.1 | 0.8–1.6 | 0.9 | 0.5–1.6 |
| Posttraumatic stress disorder | 1.6* | 1.3–2.1 | 1.8* | 1.2–2.6 | 0.9 | 0.7–1.2 | 0.9 | 0.5–1.6 |
| Social phobia | 1.6* | 1.2–2.0 | 1.2 | 0.8–1.7 | 1.4* | 1.2–1.7 | 1.3 | 0.9–2.0 |
| Specific phobia | 1.7* | 1.2–2.2 | 1.3 | 0.7–2.5 | 2.1* | 1.8–2.4 | 1.0 | 0.7–1.4 |
| Agoraphobia with or without panic | 1.2 | 0.9–1.6 | 2.6* | 1.4–4.7 | 1.3 | 0.9–1.8 | 1.1 | 0.6–1.9 |
| Externalizing | ||||||||
| Attention deficit hyperactivity disorder | 2.8* | 1.6–4.6 | 0.8 | 0.4–1.9 | 1.1 | 0.8–1.5 | 1.2 | 0.7–2.0 |
| Oppositional defiant disorder | 1.6* | 1.1–2.6 | 1.0 | 0.4–2.3 | 1.7* | 1.3–2.2 | 1.4 | 0.8–2.4 |
| Conduct disorder | 1.4* | 1.0–1.8 | 0.7 | 0.3–1.4 | 1.4* | 1.1–1.9 | 0.8 | 0.4–1.6 |
| Intermittent explosive disorder | 1.3 | 1.0–1.7 | 0.7 | 0.5–1.2 | 1.3* | 1.0–1.7 | 0.8 | 0.5–1.4 |
| Substance abuse with or without dependence | 1.0 | 0.8–1.2 | 1.3 | 0.9–1.8 | 1.4* | 1.0–1.9 | 0.8 | 0.5–1.5 |
| Substance dependence with abuse | 1.0 | 0.8–1.4 | 1.3 | 0.8–2.1 | 1.0 | 0.7–1.4 | 1.0 | 0.4–2.2 |
Comorbidity
Other Predictors of Separation Anxiety Disorder Onset and Persistence
| Variable | Total Sample | Childhood (Age 13) | Adolescence (Ages 13–17) | Early Adulthood (Ages 18–29) | Later Adulthood (Ages ≥30) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Sex | ||||||||||
| Female | 1.3* | 1.2–1.5 | 1.4* | 1.1–1.7 | 1.1 | 0.8–1.5 | 1.4* | 1.1–1.9 | 1.1 | 0.7–1.7 |
| Male (reference) | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| Educationb | ||||||||||
| Student | 1.2 | 1.0–1.6 | – | – | – | – | 1.0 | 0.6–1.5 | ||
| Low | 1.5* | 1.2–2.0 | – | – | – | – | 1.4 | 1.0–2.2 | 2.0* | 1.3–3.2 |
| Low-average | 1.6* | 1.2–2.0 | – | – | – | – | 1.4 | 1.0–2.0 | 2.0* | 1.2–3.3 |
| High-average | 1.7* | 1.3–2.1 | 1.4 | 1.0–1.9 | 1.8* | 1.2–2.7 | ||||
| High (reference) | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| Marital Statusc | ||||||||||
| Never married | 1.1 | 0.9–1.4 | – | – | – | – | 0.9 | 0.7–1.1 | 1.2 | 0.8–1.8 |
| Previously married | 1.3 | 0.9–1.8 | – | – | – | – | 1.6* | 1.1–2.3 | 1.7* | 1.1–2.5 |
| Currently married (reference) | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| Number of maladaptive family functioning childhood adversitiesd, e | ||||||||||
| 1 | 1.7* | 1.4–2.0 | 1.7* | 1.3–2.2 | 1.2 | 0.8–1.8 | 1.6* | 1.2–2.1 | 2.1* | 1.2–3.7 |
| 2 | 2.0* | 1.6–2.4 | 2.3* | 1.7–3.1 | 1.4 | 0.8–2.4 | 1.7* | 1.2–2.3 | 2.0* | 1.1–3.4 |
| 3 | 2.3* | 1.8–2.8 | 2.6* | 1.8–3.7 | 2.1* | 1.3–3.4 | 1.7* | 1.2–2.5 | 2.0* | 1.1–3.4 |
| 4 | 2.8* | 2.0–4.0 | 3.0* | 1.9–5.0 | 1.7 | 0.8–3.6 | 3.3* | 1.6–6.8 | 1.9* | 1.0–3.8 |
| ≥5 | 2.8* | 2.1–3.6 | 3.7* | 2.3–6.0 | 1.0 | 0.4–2.5 | 2.5* | 1.3–4.6 | 3.7* | 1.5–9.1 |
| None (reference) | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| Number of other childhood adversitiesf | ||||||||||
| 1 | 1.3* | 1.1–1.5 | 1.5* | 1.2–1.9 | 1.3 | 0.9–1.9 | 1.0 | 0.8–1.3 | 1.1 | 0.7–1.5 |
| 2 | 1.2 | 1.0–1.5 | 1.7* | 1.2–2.3 | 1.2 | 0.7–2.1 | 0.8 | 0.6–1.2 | 1.0 | 0.6–1.7 |
| ≥3 | 1.8* | 1.3–2.4 | 2.8* | 1.6–4.9 | 1.4 | 0.6–3.6 | 1.3 | 0.7–2.3 | 0.5 | 0.2–1.5 |
| None (Reference) | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – | 1.0 | – |
| Lifetime traumag | ||||||||||
| War | 1.1 | 0.9–1.3 | 1.6* | 1.0–2.5 | 1.4 | 0.7–2.5 | 0.9 | 0.6–1.3 | 1.0 | 0.6–1.5 |
| Violence | 1.1 | 0.9–1.2 | 2.0* | 1.2–3.3 | 0.8 | 0.5–1.2 | 1.2 | 0.9–1.5 | 0.8 | 0.5–1.1 |
| Sexual violence | 1.6* | 1.3–1.9 | 2.8 | 0.6–12.3 | 3.0* | 1.5–5.8 | 1.6* | 1.2–2.1 | 1.5* | 1.0–2.1 |
| Accident | 1.4* | 1.1–1.6 | 1.1 | 0.7–1.7 | 1.8* | 1.2–2.6 | 1.3* | 1.0–1.7 | 1.5* | 1.0–2.3 |
| Family death | 1.4* | 1.2–1.6 | 1.7* | 1.1–2.5 | 1.3 | 0.8–2.0 | 1.3* | 1.0–1.6 | 1.6* | 1.2–2.3 |
| Network events | 1.3* | 1.1–1.6 | 1.6 | 0.9–2.9 | 1.5* | 1.0–2.2 | 1.3* | 1.0–1.7 | 1.1 | 0.8–1.5 |
| Other | 1.5* | 1.2–1.9 | 1.9* | 1.1–3.3 | 1.7* | 1.0–3.00 | 1.2 | 0.8–1.8 | 2.0* | 1.3–3.3 |
Role Impairment of 12-Month Separation Anxiety Disorder
| Country Income and Age at Onset | Total | With Comorbidity | Without Comorbidity | |||
|---|---|---|---|---|---|---|
| % | SE | % | SE | % | SE | |
| Total sample | ||||||
| 4–12 years old | 33.9 | 5.2 | 37.3 | 5.9 | 8.5 | 8.2 |
| 13–17 years old | 42.2 | 7.5 | 46.5 | 8.5 | 23.7 | 10.8 |
| 18–29 years old | 35.7 | 4.3 | 45.3 | 5.3 | 16.7 | 5.3 |
| ≥30 years old | 31.7 | 5.8 | 40.4 | 7.3 | 21.2 | 8.9 |
| Total | 35.3 | 2.5 | 42.4 | 2.9 | 18.3 | 4.3 |
| Low-/lower-middle income countries | ||||||
| 4–12 years old | 24.0 | 12.2 | 24.7 | 12.7 | 0.0 | 0.0 |
| 13–17 years old | 14.5 | 7.9 | 13.0 | 8.7 | 19.4 | 18.8 |
| 18–29 years old | 19.8 | 5.8 | 32.2 | 8.5 | 8.5 | 5.7 |
| ≥30 years old | 9.0 | 5.4 | 19.5 | 10.5 | 0.0 | 0.0 |
| Total | 17.6 | 4.1 | 25.3 | 6.0 | 6.9 | 3.8 |
| Upper-middle income countries | ||||||
| 4–12 years old | 38.4 | 10.6 | 38.5 | 11.3 | 36.8 | 26.3 |
| 13–17 years old | 30.6 | 10.7 | 27.8 | 13.1 | 39.3 | 17.0 |
| 18–29 years old | 44.6 | 8.0 | 47.9 | 10.5 | 35.0 | 12.2 |
| ≥30 years old | 35.4 | 9.1 | 46.8 | 10.5 | 26.0 | 13.9 |
| Total | 38.2 | 4.1 | 41.6 | 4.4 | 30.6 | 8.9 |
| High-income countries | ||||||
| 4–12 years old | 33.6 | 6.1 | 40.5 | 7.0 | 0.0 | 0.0 |
| 13–17 years old | 62.3 | 10.5 | 71.1 | 9.2 | 0.0 | 0.0 |
| 18–29 years old | 39.8 | 6.4 | 49.1 | 7.6 | 14.7 | 7.7 |
| ≥30 years old | 38.1 | 10.4 | 41.6 | 12.5 | 28.9 | 16.9 |
| Total | 41.4 | 3.8 | 49.3 | 4.3 | 14.2 | 5.7 |
Discussion
Acknowledgments
References
Information & Authors
Information
Published In
History
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).