Kraepelin’s articulation of two major forms of psychosis—dementia praecox and manic-depressive insanity—in the 5th and 6th editions of his textbook (
1,
2), published in 1896 and 1899, represented a foundational event for modern psychiatry. Differences in course and outcome comprised the critical basis for Kraepelin’s position. The goal of this essay is to trace historically the origin of Kraepelin’s diagnostic approach. This takes us back to two earlier figures in German psychiatry, Karl Kahlbaum (1828–1899) and his protégé Ewald Hecker (1843–1909) (
3), and their writings from the early 1860s through the 1890s (
4). Kraepelin acknowledged the influence of both men on his clinical methodology (
5,
6). Kahlbaum’s work in particular has been singled out as the “first modern clinical classification” (
7), and the years leading up to the publication of Kraepelin’s influential textbook have been described as “Kahlbaum’s Era” (
8). Healy has recently suggested that contemporary psychiatry is more indebted to Kahlbaum than to Kraepelin and hence our neo-Kraepelinian era is, in fact, a neo-Kahlbaumian one (
9).
The essential position of Kahlbaum and Hecker was that the psychiatric diagnoses of mid-19th century German psychiatry were nothing but “symptom complexes.” As Kahlbaum wrote,
… the various forms in which mental illness has been known since antiquity, and is still known today, cannot be considered as different species in their own right but only as symptom-clusters which can appear in the course of different disorders. (
10, p. 236)
Hecker restates this position forcibly:
…the commonly accepted names for psychiatric illnesses, i.e., melancholia, mania, insanity, confusion and dementia are completely unsuitable and insufficient, because these names do not designate true disease forms but temporary conditions. (
11, pp. 349–350)
Kahlbaum had been the first to reach this conclusion after a comprehensive analysis of past nosologies in his seminal monograph of 1863 on the classification of psychiatric diseases (
12). The sheer number of nosologies led him not only to chide psychiatrists for their relentless addiction to novel diagnostic systems, but also to differentiate between 1) strictly symptom-oriented classifications that allowed for numerous, but often hopelessly contradictory, forms and 2) classifications that grouped symptoms into symptom complexes. None of the bygone “splitters” or “lumpers” who had developed such classifications had, however, succeeded in laying a “stable, scientific foundation” (
12, p. 139) for psychiatry. And when it came to actually diagnosing their patients, Kahlbaum argued that psychiatry’s many “rationalistic,” “non-empirical,” or “armchair” classifications had left physicians in the lurch. In fact, Kahlbaum’s look back at earlier nosologies was a story of psychiatrists often blinded by their own “rationalistic” preconceptions and in need of empirical evidence to overcome those biases.
Kahlbaum and Hecker repeatedly drew on parallels from general medicine in making their nosologic position clear. Kahlbaum noted that the earlier psychiatric symptom complexes were analogous to “dropsy,” which was “a syndrome common to a number of [disease] conditions” (
13, p. 175). Hecker wrote that if these psychiatric syndromes were “transferred to somatic medicine, they would correspond to a classification of headache, chest pain, abdominal pain, etc.” (
11, p. 350). In a later passage, Hecker described “cough” as being analogous to the psychiatric classifications of mania and melancholia (
11, p. 352).
The problem with the use of these symptom complexes, they argued, was that, because of their great heterogeneity, they prevented physicians from gaining useful insights into etiology, prognosis, and treatment. Each case became its own study. Generalizations to provide clinically useful information were impossible. Turning again to general medicine, Hecker noted the critical difference between the clinician who diagnosed a headache—providing little helpful information—and one who diagnosed a headache due to typhoid fever, where the diagnosis now carried important information about prognosis and treatment. In addition to relying on examples from general medicine, Kahlbaum and Hecker also utilized their clinical observations (
14), pointing to the proven clinical “fact” that melancholy and mania had quite variable outcomes and could end in either cure or dementia.
If Kahlbaum was dissatisfied with the confusion that plagued traditional psychiatric terminology, he was equally discontented with the findings of pathological anatomy. Mockingly, he took his neuropathological colleagues to task for suggesting that the largely unsatisfactory and confusing results of psychiatric autopsies were simply attributable to ignorance about cerebral anatomy or to the fact that they simply had not “cut up and rummaged around in enough psychiatric corpses” (
12, p. 60). The only tangible result of postmortem studies was that none of the existing nosologies could be correlated with necroscopic evidence in anything more than the most general way. These failings were, however, not largely attributable to pathoanatomic methods, but were due rather to the inadequate “descriptions and demarcations of diseases” with which neuropathologists had to work (
12, p. 173).
Skepticism about pathoanatomic research was no less forcefully expressed by Hecker. In his programmatic 1871 article on clinical psychiatry, he noted that the promise of neuropathology, particularly as articulated by earlier major figures such as Wilhelm Griesinger (1817–1868) in his dictum that mental illness was brain disease, had not yet yielded much fruit. Hecker wrote that
… the subtle anatomy and physiology of the brain are still in a dismal state and … the pathological anatomy of the psychoses up to now has offered us extremely few hard facts. (
11, p. 351)
Hecker saw no need to wait for pathological anatomy and even argued that doing so represented a kind of “passive resistance” that involved clinging to old nomenclature simply because pathological anatomy had not delivered on its promises yet (
15, p. 211). Kahlbaum and Hecker wanted to break this resistance and make the formation of clinical forms the immediate and pressing goal of a clinically oriented psychiatric research program.
Rather than calling for larger and more refined postmortem studies, Hecker laid the failure of this approach back on the inadequacies of psychiatric nosology. He argued against the then-dominant view that the way forward for diagnosis was through advances in brain-based research and that once the etiology had been discovered through neuropathology, this would lead to a definitive resolution of the diagnostic questions. Rather, Hecker turned this position on its head, arguing that psychiatric neuropathology would advance only once it had moved beyond traditional “diagnoses” that were, in fact, mere symptom complexes. With evident exasperation, he wrote,
No wonder we find in “mania” at times this and at times that change …. in the brain. Would it be any different if we were to trace the anatomo-pathological substrate of “abdominal pain”? (
11, p. 351)
Here again, using examples drawn from general medicine, Hecker countered the argument that etiologic research had to precede good psychiatric diagnoses. Many of what he tellingly termed the “empirically based disease forms” of his day (his examples included Graves’ disease and typhoid fever, the bacterial cause of which was not discovered until 1880) had unknown etiology. Psychiatry, he argued, was putting the cart before the horse by jumping enthusiastically into etiologic research before the development of true clinical syndromes. Turning to general medicine, he noted that
Long before the changes of the organs could be demonstrated with the knife in hand [pathology], certain disease forms were propounded according to empirical, clinical observation…. Why, then, in psychiatry do we want to wait until we have found an anatomo-pathological basis instead of nominating … disease forms on the basis of detailed and precise clinical observation? (
11, pp. 351–352)
In support of this key point, Hecker appealed to Rudolf Virchow (1821–1902)—a leading light of late 19th century scientific German medicine. In defending the practice in general medicine of first defining empirical disease forms and then searching for their etiology, Virchow wrote,
… I believe that there exists in every other natural science the same method of initially assigning certain things to an empirical group and giving it a name while reserving the search after the true origin... for a later time. (
15, p. 210;
16, p. 39)
So what was this method of “detailed and empirical clinical observation” that Hecker advocated and how could it be applied to psychiatric illness?
He began by stating what it was not. It did not involve using a “predefined classification principle.” Nor did it derive different forms of mental illness from the presence or absence of a single symptom. This was the classical deductive approach used in early botany and zoology, where classification proceeded by key divisions based on single characteristics, such as tree versus shrub, flowers versus no flowers, warm- versus cold-blooded, etc. (
17). Hecker and Kahlbaum argued that the major psychiatric syndromes of their day relied on a similarly simplistic a priori distinction. That is, the formula was something like “excited/grandiose + insane = mania” and “retarded/morose + insane = melancholia.” In this fashion, earlier nosologists had developed certain “rules” governing symptom aggregation and selection. But what they lacked, and what Kahlbaum and Hecker sought to add, was a “rule of the course” that would be used to break up symptom complexes and constitute new and specific disease entities (
12, p. 152).
Expressing their mission in general terms, this method required that psychiatrists “keep an eye on the whole course of the illness when observing patients” (
11, p. 352). Hecker then advocated, with a bit more precision, taking broad syndromes and, on the basis of such careful observation, splitting them up into more specific disease forms.
He used the example of infectious diseases, where “clinical disease forms” such as typhoid and cholera were separated out from the “symptom constellation” of “fever.” How was this separation accomplished? He focused initially on time course. It was rarely the occurrence of fever alone that was definitive diagnostically. Rather it was “its course, its sequential rise and fall and its exchange with fever-free time” (
11, p. 354). Of additional importance were the associated symptoms and signs, such as specific kinds of rash or diarrhea.
Hecker’s case was strengthened by the existence of a uniquely psychiatric example of his proposed method for the delineation of specific disease forms. He wrote,
The only real disease form which has gained entry into psychiatry provides the best evidence for this [proposed process]: … progressive paralysis of the insane [aka general paresis of the insane (GPI)]. (
11, p. 353)
What differentiated GPI from other less specific psychiatric syndromes was both “a peculiar and special course” and a set of relatively unique symptoms and signs. He wrote,
It is not the single symptoms of grandiose delusion of the paralysis which allow us to propound this disease form, but the grouping of these symptoms into a clinical picture and the peculiar course which the disease runs as a whole. (
11, p. 353)
It is hard to exaggerate the importance of this example of GPI in the conceptual framework that Kahlbaum and Hecker developed. We will now turn to how they applied the lessons of GPI (i.e., a distinct course accompanied by characteristic clinical features) to the articulation of what they would claim as three distinct “true diseases”: hebephrenia, catatonia, and cyclic insanity.
Hebephrenia
While first proposed by Kahlbaum, the concept of hebephrenia was fully articulated by Hecker in his famous 1871 article (
18). In describing hebephrenia, Hecker drew on the example of GPI. Hecker wrote that a key distinctive feature of the course of GPI, as noted originally by Westphal, was the “early onset of a quickly advancing dementing process among the psychiatric signs of the paresis.” He went on to write,
Kahlbaum was the first to point out … that this markedly striking feature is part of another disease, which has not much else in common with paresis: namely hebephrenia. (
18, p. 93)
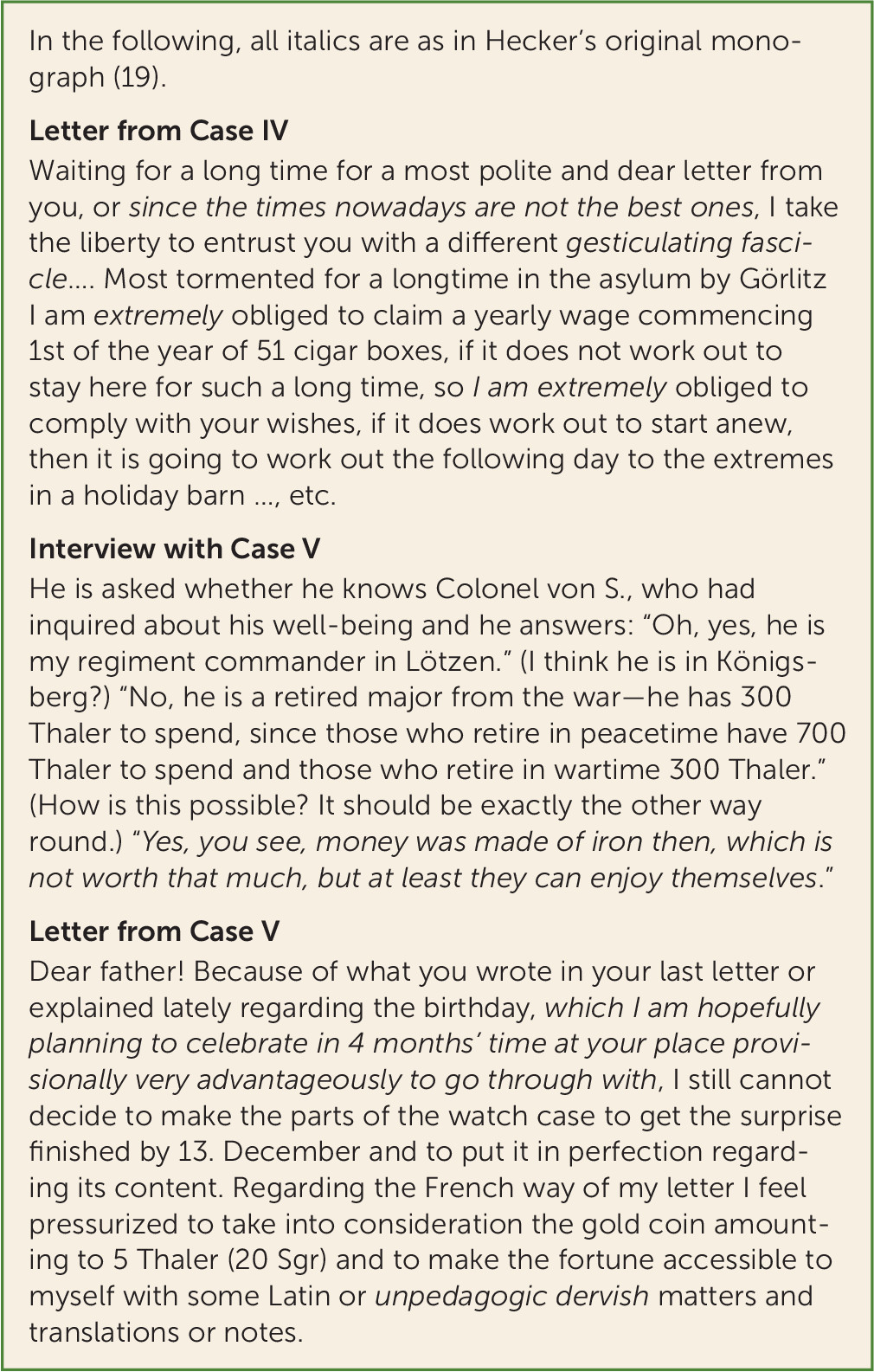
Hebephrenia stood out, Hecker went on to argue, “due to its typical course and range of specific symptoms” (
18, p. 93), the same language he used for describing the kinds of features that made GPI so clearly a distinct diagnostic entity. In particular, Hecker repeatedly commented on the characteristic thought disorder that occurred in hebephrenia and was sufficiently distinctive that “very often one can make the diagnosis just from the hebephrenic’s letters” (
18, p. 99). In particular, he noted that they often were “almost entirely consisting of shallow, meaningless phrases” (
19, p. 235). Several quotes from the speech and letters of Hecker’s cases are presented in
Figure 1.
Hecker’s use of these letters is important for reasons that relate specifically to his aim of tracking the early development of hebephrenia in his patients. The letters were so important that Hecker’s clinical case material was confined to patients in whose files such letters existed. He valued the letters—citing them verbatim and liberally—for the “objective” and “unbiased” preclinical evidence that they yielded. Because of hebephrenia’s rapid progression to dementia, alienists had usually seen only the later stages of the illness, after the “actual illness” had run its course and the patients had already arrived “mentally crippled” in the asylum (
20, p. 396). Patient letters opened a window onto the course of hebephrenia.
Hecker’s and Kahlbaum’s understanding of hebephrenia was facilitated by the fact that, unlike most alienists, they were well placed to study psychiatric disorders in adolescents. Their asylum in Görlitz was a private sanatorium that served a wealthy, international clientele and that had acquired a reputation as an institution specializing in the treatment of young patients (
21). As a part of the asylum’s therapeutic regime, Kahlbaum developed a
pädagogicum to enable “specialized medical observation and treatment” for a large and rapidly growing number of young patients. The
pädagogicum employed a special staff of teachers who were “embedded organically and methodologically” into daily asylum life and who, through “patient, methodical, pedagogical influence,” aimed to correct their young patients’ “failed up-bringing” (
12, p. 6;
22;
23).
Kraepelin’s university clinic had no
pädagogicum. Whereas Kahlbaum and Hecker had used hebephrenia’s course to establish it as a distinct nosological entity, Kraepelin believed that they had found only a specific subtype of mild dementia characteristic of younger, upper-class patients. Drawing on the work of his student Leon Daraszkiewicz (
24), Kraepelin therefore admitted more severe forms of hebephrenia that terminated in severe dementia and were less influenced by external factors (
6,
25).
The influence on Kraepelin of Hecker’s work on hebephrenia can be clearly illustrated by this short quote from Kraepelin’s first systematic description of dementia praecox in the 4th edition of his textbook:
The first precise, and in many ways exemplary, description of certain forms of dementia praecox was given by Hecker in 1871. (
26, p. 442)
Indeed, Kraepelin explicitly emphasized the deep affinity between Hecker’s hebephrenia and dementia praecox. At the same time, however, he believed that Hecker’s category was too narrowly focused on pubescence and needed to be expanded to include Daraszkiewicz’s findings. It was precisely to accommodate this expanded understanding of hebephrenia that Kraepelin proposed the term “dementia praecox” (
27, p. 1016), a term used previously by German and French psychiatrists, such as Heinrich Schüle and Bénédict Morel (
28–
30).
Catatonia
Kahlbaum began his famous 1874 monograph on catatonia (
31) by commenting on the role of “organic signs” in the diagnosis of psychiatric syndromes—were they nonspecific or specific and therefore of critical diagnostic importance? He answered this question by giving a brief history of the then-current thinking about the etiology of GPI:
At first, the paralytic component was regarded merely as a complication … but it gradually became clear that the psychiatric disorders involved were present more specifically in association with the pathognomonic paralytic phenomena typical only of this disease and that there was a close connection between the progress of the psychic phenomena and the somatic components. (
31, p. 7)
He then began his description of what he called catatonia and its close relationship with the “striking” cataleptic states and “waxen” flexibility. He wrote,
These interesting somatic features are as unique in the diagnosis of this particular illness as are the somatic components of general paralysis of the insane. (
31, p. 9)
But it was not only the presence of characteristic clinical symptoms that made catatonia resemble GPI:
In some aspects, such as the clinical course marked by the passage through various phases of distinct mental states and the significant association with muscular disorders, the one is analogous to the other. (
31, p. 9)
Later in the monograph, he again focused on course and its ability to help define diseases from more heterogeneous symptom complexes. After describing the rich clinical symptoms seen in his catatonic cases, he wrote,
If one observes, however, how these combinations repeat themselves frequently and how, when they do appear, the combination occurs in a certain sequence which recurs again and again in different patients, the conclusion must be drawn that all these occurrences have a common etiology and only represent progressive transformations with the same basic process. (
31, pp. 26-27)
He summarized his views as follows:
In this newly defined group of disorders, similar to the general paresis of the insane (GPI) … clinical changes in the locomotor apparatus form the main and typical features of the disease; in addition, each disease (GPI and this disease) exhibits manifold patterns of symptoms. (
31, p. 27)
Kraepelin’s uptake of Kahlbaum’s views on catatonia was slow. In 1879, five years after publication of
Catatonia, alienists in the Munich asylum where Kraepelin worked had yet to diagnose a single case of the disorder (
6). Furthermore, Kraepelin’s early mentors and colleagues thought little of Kahlbaum’s work (
6,
32,
33). And more than a decade later, in 1890, Kraepelin still openly resisted Kahlbaum’s interpretation of catatonic symptoms, hoping to demonstrate that they were characteristic of a specific, volitional disorder as opposed to Kahlbaum’s view of catatonia as a motility psychosis (
6,
34). Nevertheless, Kraepelin ultimately adopted and popularized Kahlbaum’s concept of catatonia in his textbook, partially in the 4th edition of 1893 and completely by the 5th edition of 1896 (
35).
Like Kahlbaum and Hecker, Kraepelin also focused on the disorder’s course and outcome in isolating its characteristic symptoms. But his observations yielded a fundamentally different clinical picture of catatonia. Whereas Kahlbaum’s catatonia was a so-called “total” mental disorder that progressed from mania and melancholy through insanity to dementia, Kraepelin dispensed with this sequence and posited a much more negative outcome. And whereas Kahlbaum described catatonia as a motor-neural disorder and distinguished it from GPI chiefly on the basis of its cataleptic symptoms, Kraepelin pointed to patients’ waxy flexibility in placing greater emphasis on a volitional rather than a neuropathological etiology. (Crucially, it was the poor outcome of catatonia that brought him to associate it with dementia praecox. In his years of clinical experience, Kraepelin claimed to have never encountered a case with obviously catatonic symptoms that did not culminate in dementia. Furthermore, the “frequency of catatonic signs” in more typical cases of dementia praecox strongly suggested that both were manifestations of the same morbid process [
26, p. 454].)
Cyclic Insanity
We can also learn about how Kahlbaum and Hecker used information about course and symptoms to move toward empirical disease forms by analyzing Kahlbaum’s discussion of
cyklisches Irresein, or “cyclic insanity,” published in 1882 (
36). The fundamental contrast he made was between the occurrence of the symptoms of mania and melancholia in cyclic insanity versus in what he called “typical insanity.” According to his definition, cyclic or circular insanity was
a form of illness, in the course of which melancholia and mania, two apparently contrasting states, are observed to follow each other. This succession repeats quite often and more or less regularly with intervening intervals of true or at least apparent mental health. (
36, p. 83)
Typical insanity, by contrast, was the name he gave to a unitary psychosis as articulated by Wilhelm Griesinger and Heinrich Neumann. As understood at this time, the basic idea was that there was only one true form of insanity and all the individual major syndromes were just transitory manifestations of that one disorder. Focusing initially on mania, Kahlbaum noted that the course was quite different from that seen in cyclic insanity:
In typical insanity, the manic phase after having reached a peak without remission can change into a kind of insanity with confusion that may eventually reach a stage of idiocy or so-called terminal dementia. (
36, p. 84)
He noted this apparent discrepancy in the course and outcome of these affective syndromes as follows:
It is often found that the course of typical insanity, once the peak of mania or rage has passed, leads to weakness and eventually to complete decline of mental power. In comparison to this course, it is remarkable that there are also many cases of illness in which melancholia and mania can be very intense, yet end in remission without mental decline. (
36, p. 84)
Kahlbaum then asked the key question “Are the melancholia and mania in cyclic insanity to be considered the same as the melancholia and mania in typical insanity?” (
36, p. 84). He noted the general similarity of the clinical forms but then made the trenchant observation that “a closer look at their detailed features reveals substantial differences.” Note that he began by articulating differences in the course of these syndromes, but now he was moving to the second criterion that he wanted to use in shifting from symptom complexes to empirical disease forms, that is, to differences in symptoms and signs.
He began with melancholia. In typical insanity, the initial melancholic phase was often of a “vague character” and represented “the sultriness before the thunderstorm” (
36, p. 84) of the emerging psychosis. By contrast, in the melancholia of cyclic insanity, the mood symptoms were much more distinct, often accompanied by self-accusations, and closely resembled the full melancholic syndrome seen “in disorders in which only melancholia occurs” (what we would now call unipolar major depression).
Kahlbaum then noted that “the difference in mania between cyclic and typical insanity is even sharper” (
36, p. 84). To follow his argument, we need to note that Kahlbaum proposed a version of faculty psychology that divided the mind into three major functions: feeling, intellect, and volition. In typical insanity, the manic syndrome was not restricted to the domain of feeling, but it “quickly reaches such a degree and extent that all the major mental functions are disturbed” (
36, p. 84)—that is, both intellect and volition—and becomes a “pervasive derangement.” By contrast, in the mania of cyclic insanity, the disturbance was restricted only to the domain of feeling. They
have an irrepressible cheerfulness, without real delusions, but only exaggerations of self-esteem and of other emotions. Such patients can explain everything they say and do in an understandable and even seemingly reasonable way. (
36, p. 84)
Using mania in a way that is unfamiliar to us (as an agitated, grandiose psychosis affecting all aspects of mental functioning—mood, intellect, and volition), Kahlbaum summarized his conclusion as follows:
The stage of exaltation in the cyclic insanity group is not an actual mania involving exaltation of all mental functions, only of the emotions. In contrast, in typical insanity leading to terminal idiocy, the exaltation is a true mania. (
36, p. 87)
So we began with the two classical symptom complexes of mania and melancholia. Kahlbaum then argued that they could occur in two different disease courses—as part of typical insanity and cyclic insanity. He then observed the associated difference in course with the former often leading to deterioration and the latter to multiple recurrences but without dementia. Then he focused in on the clinical symptoms, noting, on closer observation, a number of important differences. And finally, in keeping with his taxonomic agenda, Kahlbaum named these two forms “vesania typica circularis” and “cyclothymia.”
In the 6th edition of his textbook, published in 1899, Kraepelin claimed that he had found no clinical evidence to support Kahlbaum’s distinction between “vesania typica circularis” and “cyclothymia” (
37, vol. 2, pp. 416–417). Kraepelin arrived at this conclusion not least because he was no longer beholden to Kahlbaum’s ‘typical insanity’ and the notion of unitary psychosis that underpinned it. But he also drew on his own clinical observations, citing cases involving severe manic episodes that did not result in cognitive deterioration. As Kraepelin’s category of manic-depressive illness developed, however, it was clearly not the all-encompassing “total” disorder of Kahlbaum’s typical insanity that culminated in dementia but, instead, much closer to his cyclical affective disorder. Critically, he adopted Kahlbaum’s key concept that patients with manic-depressive insanity did not develop dementia even in the setting of chronic symptoms. This was clearly expressed in the final edition of his textbook:
… the attacks of manic-depressive insanity with the delimitation attempted here never lead to profound dementia, not even when they continue through life almost without interruption. Usually all morbid manifestations completely disappear; but where that is exceptionally not the case, only a rather slight, peculiar weakness develops. (
38, p. 3)
Interestingly, Kraepelin expanded Kahlbaum’s concept of cyclothymia to include cases with single manic or depressive episodes. That, however, is another story.
Conclusions
The influential nosology for major psychiatric disorders developed by Kraepelin in the 1890s and still of substantial importance to our field did not arise de novo. Rather, Kraepelin’s work was strongly influenced by and indeed largely based on concepts developed in the preceding decades by Kahlbaum and Hecker. The field has been slow to recognize this interdependence, in large part because neither Kahlbaum nor Hecker was widely known in their own day. Neither had university appointments (a critical mark of professional status at this time), and both spent almost all of their careers in private asylums. This dependence of Kraepelin on his predecessors is well captured in a key early review of his work by the then rising star of American psychiatry, Adolf Meyer. He wrote,
A very stirring turn in psychiatry has come lately from Kraepelin, who took a stand foreshadowed by Kahlbaum, but never demonstrated with such consistency before. With the fifth edition of his textbook, the time had come to break away from the resigned symptomatic attitude [as] the pride of the clinician demanded disease entities. (
39, p. 651)
Kahlbaum, Hecker, and Kraepelin shared a commitment to a clinical research agenda for psychiatry in which the first and foremost task was to utilize the methods of clinical assessment and follow-up to help define disease forms. The conceptual framework for this approach was laid down by Kahlbaum and Hecker, and it was further developed by Kraepelin. Indeed, a major focus of Kraepelin’s clinical research career involved developing more fully the nosologic paradigm proposed by his older colleagues (
4). Working in high-prestige academic centers with a large flow of patients and sufficient staff to assist him, and using his famous system of “patient cards” (
Zählkarten) (
40,
41), Kraepelin was able to expand considerably the clinical program of research along the lines first articulated by Kahlbaum and Hecker (
4).
It is important to emphasize that, in the decades around 1900, Kraepelin was not working in isolation. Major psychiatric nosologies were proposed by his approximate contemporaries, including Kraft-Ebbing (
42,
43) and especially the neuropsychiatrist Carl Wernicke (
44–
47). While Wernicke’s work led to an alternative diagnostic tradition within German psychiatry, represented by Karl Kleist and Karl Leonhard (
48), its contemporary influence on psychiatric nosology has been minor compared with Kraepelin’s.
The nearly world-wide acceptance of Kraepelin’s nosologic system arose from a range of factors, including his prominent status in the field of psychiatry, the broadly recognized quality and subsequent wide influence of his textbook, and the ability of this new paradigm to convey a sense of excitement and scientific promise compared with the existing syndromal typologies, which were seen as old and increasingly scientifically sterile (
49). These three men also shared a deep skepticism for the “brain-based” neuropathological paradigm of psychiatric research dominant in most European academic centers during the latter half of the 19th century. However, this skepticism never prevented Kraepelin, as a professor in both Heidelberg and Munich, from recruiting and supporting the research of leading neuropathologists, including Franz Nissl, Alois Alzheimer, and Korbinian Brodmann (
50,
51).
During the critical period from about 1860 to 1900, Kahlbaum, Hecker, and Kraepelin were together responsible for a paradigm shift in the conceptualization of psychiatric diagnosis. They moved from the symptom-based syndromes popular since the late 18th century (mania, melancholia, dementia, etc.) and from the eclectic range of 19th-century armchair nosologies to what we might call proto-disease entities. In this effort, they were strongly influenced by parallel developments in general medicine, especially the rise of bacterial theories of disease (
52) in which different disorders often had distinct symptoms and illness courses. Even more important, their thinking was shaped by the increasing understanding and delineation of the syndrome of GPI. This disorder, with its distinctive course and characteristic symptoms that were increasingly clearly delineated over this time period (its etiology was not definitively demonstrated until 1913 [
53]), was paradigmatic for these three clinical researchers, shaping their approach to the other psychiatric syndromes then populating Europe’s asylums. Put simply, their hope was that—as GPI was shown to have distinct symptoms, a particular course, and eventually a unique etiology—a similar progression of medical understanding would evolve for the other major psychiatric syndromes.
This paradigm shift was, however, built on a promise that has not yet been fulfilled. GPI has proven to be the exception and not the rule among the major psychiatric syndromes. We still do not know whether this “Kahlbaum-Hecker-Kraepelin paradigm”—defining disorders on the basis of distinctive symptoms and course—will produce psychiatric syndromes that are sufficiently homogeneous to yield up their etiologic secrets. Indeed, Kraepelin’s nosology met with vigorous opposition by some psychiatric contemporaries (
30,
50,
54). He was particularly criticized for his
idiosyncratic use of prognosis as a key to diagnosis…. [noting that] the criterion was logically weak since the course of any illness also depended upon fortuitous conditions, such as the severity of the lesion and host resistance, neither of which could be considered as ‘essential’ aspects of the disease. (
4, p. 818)
Our task here is not to prognosticate the future of this paradigm so central to the history of our discipline but to suggest that understanding its historical origins will help us now and in the future to evaluate its strengths and limitations.
A final question is whether the sole focus of the Kahlbaum-Hecker-Kraepelin paradigm on clinical research methods restricted the subsequent trajectory of psychiatric nosology. Each of these three clinicians reacted skeptically to the premature claims in late 19th-century Germany that brain science, then largely neuropathology, would soon be capable of solving the problems of psychiatric nosology. Their colleague and competitor Carl Wernicke attempted to develop a psychiatric nosology founded in brain function (
44–
47), but that effort proved premature and bore limited scientific fruit. Would a more inclusive nosologic vision that included both biological and clinical methods have led to more rapid progress in psychiatric nosology?
Such historical counterfactuals (“What would have happened if…?”) are problematic to evaluate given the inherent unpredictability of historical processes. Our view of the recent history of biological psychiatry suggests a nuanced response. Certainly, on their own, the robust claims from biologically oriented researchers that psychiatric nosology could be based on simple neurochemical processes (
55,
56) or major Mendelian-like genes (
57–
59) have proven incorrect. Indeed, reviews as recent as DSM-5 have concluded that the best-replicated findings of biological psychiatry were too nonspecific to be of diagnostic utility (
60). What was potentially lost, then, was not a single major biological breakthrough that would illuminate an entire nosologic area, like the discovery of the
Treponema. Rather, what may have been missing was an iterative process in which the mutual strengths of the available fallible clinical and biological tools interacted synergistically on nosologic problems. With the increasingly powerful biological tools now available to our field, it may be time to revisit the question of whether and how biological measures can be usefully integrated into clinical approaches to psychiatric nosology like those pioneered by Kahlbaum, Hecker, and Kraepelin.