You Seldom Get a Second Chance With a Gunshot: Lethality of Suicidal Acts
How Early is Too Late?
References
Information & Authors
Information
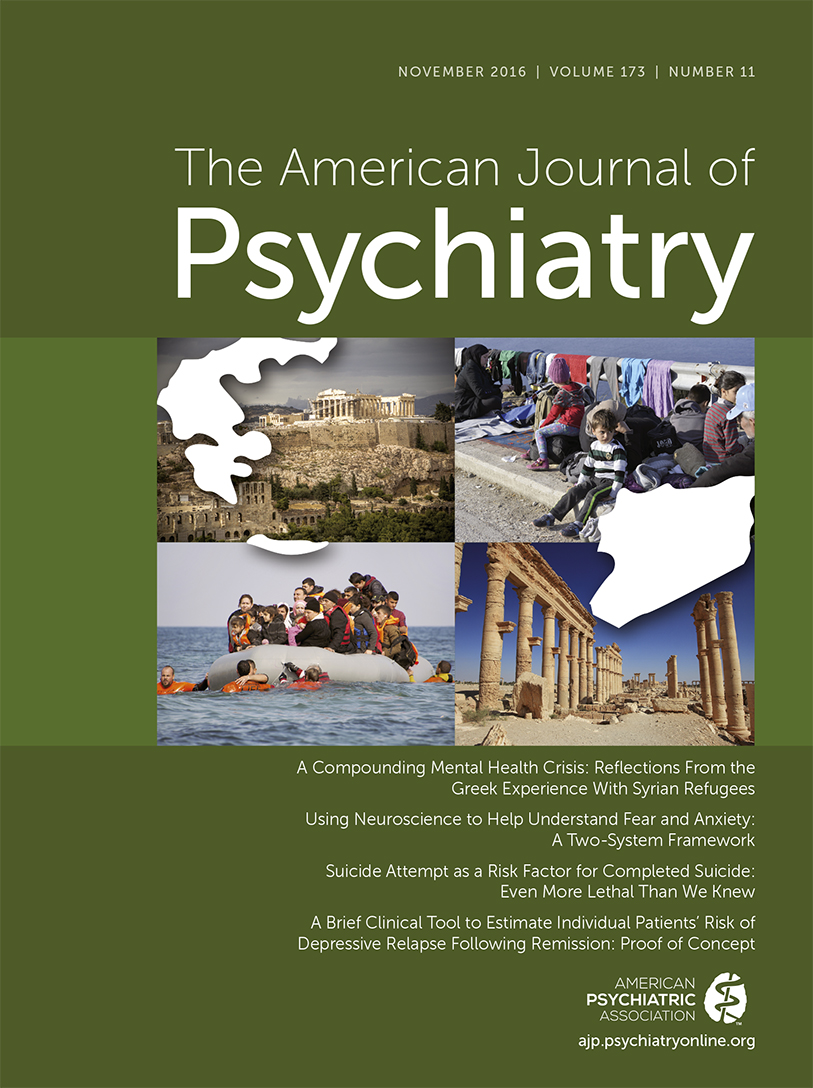
Published In
History
Keywords
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.