Report of the treasurer
Bruce Schwartz, M.D.
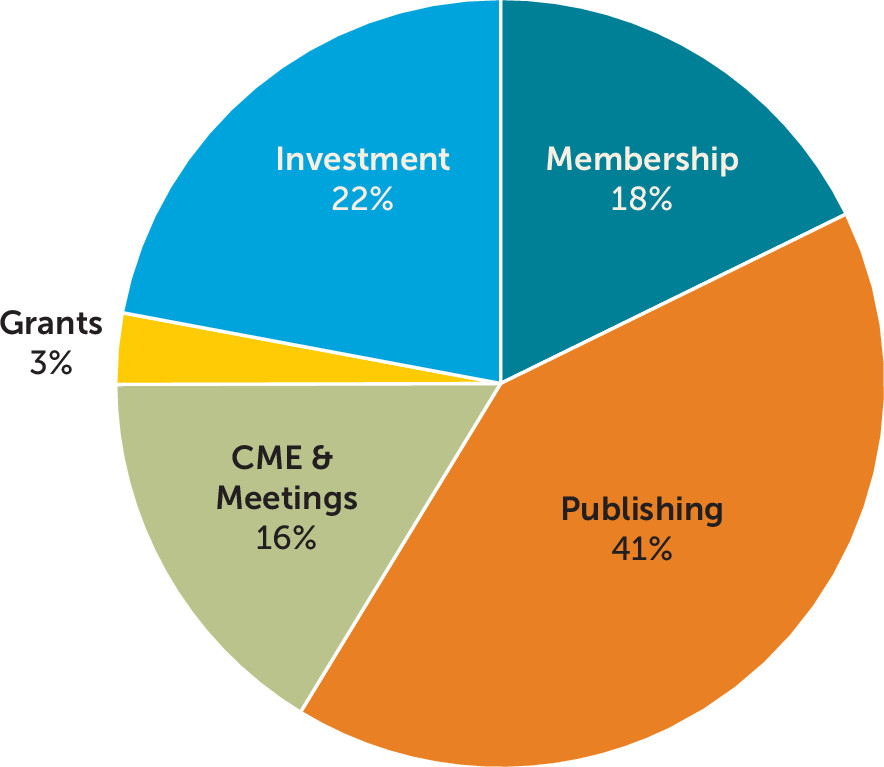
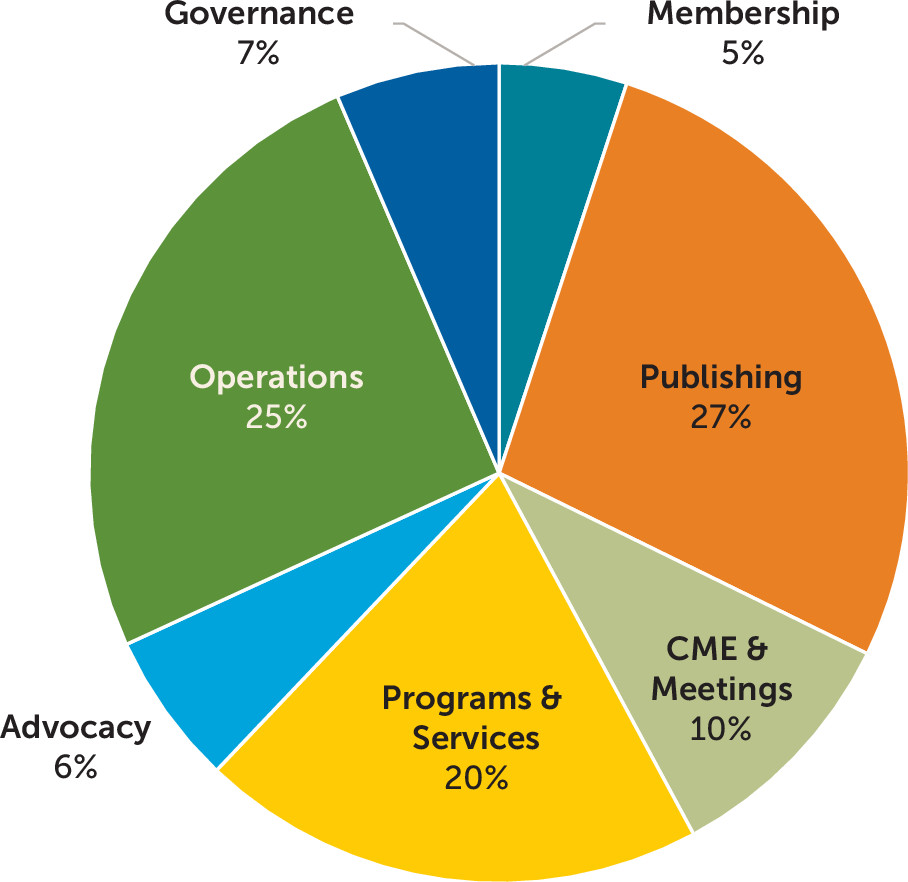
For the year ended December 31, 2017, unaudited net income was $10.5 million, based on $60.5 million in revenue and $50.0 million in expenses (see
Figures 1 and
2). Net income was $4.0 million higher than in 2016 and $11.2 million higher than the ($.7) million deficit that was budgeted. In 2016, net income was $6.5 million, based on $56.5 million in revenue and $49.7 million in expenses.
Most of the increased net income is attributable to higher investment income. The budget anticipated earning $3.0 million of investment earnings that would be used to fund the operating budget; whereas in 2017 the reserve portfolio returned $13.3 million, a 15.3% return. During 2016, the portfolio earned $7.1 million, a 9.4% return.
Revenue-producing activities, which are those business lines that generate a positive return and fund the Association’s programs and operations, include membership programs, publishing activities, and medical education and meetings. These activities provided $24.5 million in revenue after expenses. This amount was $.7 million lower than in 2016. The reduced revenue is attributable to lower print advertising revenue and lower membership dues revenue, offset by higher revenue from the medical education and meetings. The number of members continues to rise; however, the number of members moving into the reduced dues or dues exempt categories continues to rise as well, resulting in $.4 million less in revenue. 2017 also saw a significant decline in print advertising for Psychiatric News and the American Journal of Psychiatry. Publishing expenses were reduced to partially offset the revenue loss; however, the net revenue declined by $.9 million from 2016. The 2017 annual meeting was held in San Diego and saw increases in attendance and the number of exhibitors and sponsors.
Expenses for Programs and Services, which includes federal advocacy, policy development, research, diversity, and communications, was $.6 million higher than in 2016. The higher costs are due to the filling of vacant positions in the areas of research, education, diversity, and policy.
Expenses for the APA mental health registry, PsychPRO, increased by $.7 million over 2016 as the registry transitioned from development into operational.
APA’s financial position remained strong, with net assets of $98.1 million, cash of $8.6 million and investments of $98.2 million.
Report of the Ceo and Medical Director
Saul Levin, M.D., M.P.A.
I am pleased to present the CEO and Medical Director’s report for the APA President’s year May 2017–May 2018, which outlines the Administration’s actions, activities, and accomplishments in the past year according to the APA’s strategic initiatives.
In March, the inaugural APA Board of Trustees meeting took place at APA’s new headquarters at 800 Maine Ave. SW, Washington, DC, along with the Grand Opening with DC Mayor Muriel Bowser and the APA Foundation Board of Directors meeting. The APA Board passed an action thanking Dr. Frank Brown for his work and leadership at the APA and as the Chair of the Building Committee and Dr. David Fassler for his guidance starting as the APA Treasurer and then on investment oversight that set the opportunity for the APA Building.
The APA Administration continues to implement the APA’s strategic initiative objectives voted by the Board of Trustees within the organization’s core areas as follows:
Advancing Psychiatry
Children’s Health Insurance Program (CHIP): Congress passed a 6-year reauthorization of CHIP in January. The $14 billion program provides health insurance to nearly nine million children and adolescents from low-income families who do not qualify for their state’s Medicaid program. It also provides access to quality evidence-based mental health care services for the estimated 850,000 CHIP beneficiaries experiencing serious behavioral or emotional disorders.
APA Administration collaborated with district branches to engage members via a member-wide grassroots effort. As a result, council members and APA’s advocates sent over 1,400 letters to their respective federal lawmakers and governors, additional phone calls to congressional offices, or urged action through social media.
Opioid epidemic funding measures: APA continues to advocate for sustained funding for infrastructure-related programs and efforts, including education, provider training, and general resources to address the crisis. Congress passed the Omnibus spending bill for fiscal year 2018 that included $3.6 billion in funding to fight the opioid epidemic. A total of $1 billion is dedicated to state opioid response grants under the Substance Abuse and Mental Health Services Administration (SAMHSA) as authorized under the Cures Act. In addition, Congress appropriated $500 million to the National Institutes of Health for a new initiative to research opioid addiction, development of opioid alternatives, pain management, and addiction treatment. APA administration will continue to engage Congress and the Committee of Jurisdiction on the opioid issue.
Veterans’ health care legislation: APA continues to see legislation adopting a variety of approaches to enhancing primary and mental health care services for veterans. Senator Dean Heller (N.V.), along with Senators John Cornyn (Tex.) and Marco Rubio (Fla.), introduced S. 2548, the Veteran Urgent Access to Mental Healthcare Act. The legislation would require the Department of Veterans Affairs (VA) to provide veterans released from the military with an “other-than-honorable” discharge with access to mental health assessments and treatment. The legislation mandates a VA study to evaluate the effect of combat experience on veterans’ mental health. APA supported the proposed legislation.
Congress prioritizes the provision of quality care for veterans under the current administration. The FY2018 Omnibus provided $81.5 billion in discretionary funding for VA programs, an increase of $7.1 billion above the FY2017 level. The measure aligns funding with the Administration’s priorities providing $782 million for a new VA-Department of Defense (DoD) compatible electronic health record system to ensure an accurate, seamless transition of care for service members transitioning under the VA. The measure also appropriates $68.8 billion to VA medical care, providing continuation and expansion of health care services to approximately seven million veterans and their families. Additionally, I serve as a member of the Special Medical Advisory Group that advises on matters related to clinical care, research, training, and planning on shared issues facing the VA.
Ligature risks: As a function of implementing their “Zero Suicide” campaign, supported by CMS, the Joint Commission (TJC) surveyors increased scrutiny for risks of ligature, suicide, and other self-harm, determining that many facilities are not sufficiently mitigating those risks. The surveyors lacked standard guidelines for these reviews and mandated costly, inconsistent standards. APA met with CMS to voice concerns regarding lack of standardization with the new surveyors and unintended consequences such as facility closures, bed reductions, or other cuts in mental health services. At the request of CMS, APA surveyed our membership regarding these changes and potential affects to the facilities and are finding that some facilities may decrease the number of beds or other services as a result of the fines associated with citations given. APA continues to advocate for more standard guidelines for the reviews and alternative solutions to ensure that no facilities close, reduce beds, or decrease other mental health services.
MACRA 2018 Rule: CMS issued the final rule for the second year of the Quality Payment Program. Below are some highlights of that rule:
1) The low-volume threshold: The low-volume threshold increases in 2018 to 200 Part B patients or $90,000 Part B allowable charges per year (from 100 patients or $30,000, for 2017). Together with exclusions for the first year of Medicare participation and participating in “advanced” alternative payment models, this will exempt about 60% of the 1.5 million clinicians providing Part B services. The 600,000 clinicians who are still subject to the Merit-Based Incentive Payment System (MIPS) reporting and adjustments include about 11,500 psychiatrists.
2) Virtual groups: Individual clinicians and small practices that exceed the low-volume threshold could apply by December 31, 2017, to report as a virtual group for 2018.
3) Small practices: Practices of up to 15 clinicians may:
• Apply for a hardship exception from the MIPS ACI category, which would increase the weight of their score in the quality category to 75%;
• Receive some points for partial reporting of MIPS quality measures;
• Report fewer improvement activities and still receive full credit; and
• Earn five bonus points on their final MIPS score.
4) MIPS Quality category: This category accounts for 50% of the MIPS composite score for 2018. To earn points in this category requires reporting at least six quality measures. Those reporting fewer measures may avoid penalties if no other measures are available that are relevant to their practice and/or patients. (Please see the Research section for additional MIPS information tied with APA’s Mental Health Registry, PsychPRO.)
5) The MIPS Advancing Care Information category: This category accounts for 25% of the MIPS composite score. Hospital-based clinicians may apply for a hardship exception from this category. The weight of their quality score will increase, to account for 75% of their MIPS composite score. Bonus points are given for using the 2015 (versus 2014) edition of certified electronic health record technology and reporting to public health agency or clinical data registries.
APA Payment Reform Toolkit: APA added to the APA Payment Reform Toolkit to help psychiatrists avoid future penalties under Medicare’s new MIPS. The APA guide, “Take Action Now to Avoid Medicare Penalties,” offers step-by-step instructions to help psychiatrists navigate the new MIPS policies.
CONNECT for Health Act: APA supported telemedicine provisions in the CHRONIC Act that passed as part of the most recent budget legislation. The legislation facilitated Medicare Advantage to incorporate telehealth coverage in its policies beginning in 2020.
Puerto Rico Relief: Hurricane Maria left destruction in its wake for more than three million residents of Puerto Rico. This humanitarian crisis was met with the territory’s looming health care crisis. Puerto Rico’s health care system was, and still is, being pushed to its limits in the aftermath of Hurricane Maria as hospitals and clinics grapple with crippling losses of essentials, including access to medications and dialysis machines.
APA sent a letter to Congressional leadership urging for immediate resources and financial aid. The President has since provided relief and deployed resources to be used in an efficient and effective capacity to support those Americans affected by the disaster and with backing from the APA Foundation, APA members and staff donated more than $30,000 to the relief effort.
Assistant Secretary for Mental Health and Substance Use: The Senate confirmed the nomination of Elinore McCance-Katz, M.D., Ph.D., for Assistant Secretary for Mental Health and Substance Use. The confirmation of Dr. McCance-Katz, a long-time APA member, is especially of importance in bringing psychiatric leadership to this crucial new position at SAMHSA created in the 21st Century Cures Act. The Assistant Secretary is charged with overseeing SAMHSA and coordinating mental health and substance use programs and research across all federal agencies. APA endorsed Dr. McCance-Katz and galvanized support behind the nomination.
Mental Health Parity: Parity compliance and enforcement efforts continue to focus on several priority areas of federal and state parity regulatory efforts. APA is working with APA district branches on parity compliance and enforcement efforts. We are also working with the Department of Health and Human Services (HHS) and the Department of Labor to develop the parity guidance and action plan requirements codified in Section 13001 of the Cures Act, including model audit and disclosure practices.
Medicare: Over the course of spring and summer 2017, APA submitted formal comments in response to several Medicare proposed rules for 2018:
•
Quality payment program: APA successfully advocated for improvements to MIPS that exclude many psychiatrists from MIPS reporting and penalties and help others to earn a bonus. Starting in 2018, only psychiatrists with over 200 Part B patients and over $90,000 in annual charges must do MIPS reporting to avoid a future payment decrease. Small practices that do MIPS reporting gained several advantages, including a virtual group reporting option, a hardship exception from the Advancing Care Information (EHR) category, and bonus points on their final score.
•
Medicare Physician Fee Schedule: CMS finalized several proposals APA supported in the 2018 Medicare Physician Fee Schedule, including extending coverage for collaborative care services to federally qualified health centers and rural health centers and increasing the payments to those providing collaborative care services.
•
Quality measurement: APA noted that the current quality programs do not include enough quality measures that are “meaningful, appropriate, or applicable” to psychiatric patient care. The proposed rules in this past cycle have included quality measures that the APA was not able to support for inclusion into the respective quality reporting programs because detailed information about these measures was not provided. APA comments requested that more information be shared so that we could provide additional feedback on their proposed additions to these programs.
Health Information Portability and Accountability Act (HIPAA) and Health information technology (HIT): Due to member questions received through the Helpline, APA developed a primer for membership on HIPAA and HIT to help members keep patient information private and secure.
Recruitment into psychosomatic medicine specialty: In collaboration with the Council on Psychosomatic Medicine, a
video to help recruit medical students into psychosomatic medicine was finalized and is available on the APA website.
Updated dementia measure set: The American Journal of Psychiatry and Neurology, the journal of the American Academy of Neurology (AAN), simultaneously published the Executive Summary of the jointly owned and managed “Dementia Management Measure Set Update.” This measure set was developed under a partnership between the APA and AAN to provide meaningful quality measures to psychiatrists and other health care providers who treat this vulnerable patient population.
Regulatory relief: APA participates in the American Medical Association (AMA) Workgroup on Regulatory Relief with other medical specialty societies. The workgroup has developed a set of priority areas for discussion and advocacy with the new Administration, especially the new leadership of HHS. The APA administration participated in a meeting at HHS to discuss how to relieve physicians’ burdens.
Supporting Research
APA Mental Health Registry (PsychPRO): PsychPRO prepared participants to meet MIPS reporting requirements within the 2017 CMS program reporting period. A total of 607 providers (in 245 practices) have signed agreements to join the registry, and 262 providers (in 44 practices) have been onboarded in terms of EHR integration, complete data mapping and refinement, and the ability to review their quality measures on their dashboards. To date, we have de-identified information in PsychPRO from over 72,000 patients, resulting in 329,000 clinical encounters.
PsychPRO was again successful in becoming certified as a 2018 Qualified Clinical Data Registry (QCDR), receiving approval from CMS this January. PsychPRO’s designation as a QCDR allows it to continue being used to develop and test new quality measures that better reflect the value of mental health care delivered in a variety of settings. For more information about the registry, please visit
www.psychiatry.org/psychiatrists/registry.
Research Colloquium for Junior Investigators: Four post-Research Colloquium webinars for the 2017 cohort have been completed, with a total of 33 (67.3%) junior investigators in attendance.
A total of 70 applications were received for the 2018 Research Colloquium, a 22% increase from the previous year. The 70 applications included 12 from international fellows from Argentina (1), Belgium (1), Brazil (1), France (2), Mexico (1), the Netherlands (1), Nigeria (2), Peru (2), and Switzerland (1). Applications were reviewed by the research track leads, and acceptance letters were sent to 52 junior psychiatrist investigators. The Society of Biological Psychiatry and the American College of Neuropsychopharmacology continue to collaborate with the APA/APA Foundation on this year’s Colloquium.
Proposals for Changes to DSM-5: Five proposals for minor changes to DSM received approval for public comment from the Subcommittee on Minor Changes and the DSM-5 Steering Committee. These proposals were posted for public comments for a 1-month period from November 22, 2017, to December 22, 2017. The public comments were summarized and shared with the Subcommittee on Minor Changes for additional deliberation. The comments were largely supportive of the proposals; therefore, both the Subcommittee on Minor Changes and the DSM-5 Steering Committee made a final determination to recommend approval of the proposals as submitted.
Education
Workgroup of Physician Well-Being and Burnout: This workgroup, chaired by Richard Summers, M.D., meets monthly by phone and met in person at the APA Annual Meeting. The workgroup launched a website (
https://psychiatry.org/wellbeing) that includes an online self-assessment tool and well-being resources. The workgroup continues to add new content to the website, including resources, short and informative video testimonials from psychiatrists, news articles, and other educational tools.
American Board of Psychiatry and Neurology (ABPN) Maintenance of Certification (MOC) Part 3 Pilot: ABPN plans to pilot an alternative pathway for the MOC-3 10-year exam. This pilot is currently under development and will launch in January 2019. All diplomates who are currently participating in MOC, are due to recertify in 2019, 2020, or 2021, and who are in good standing will be eligible to participate. All eligible diplomates received an e-mail from ABPN in December 2017 with details of the program and were contacted again on March 22, 2018, with formal instructions on how to enroll in the program. Enrollment closed May 1, 2018.
The pilot program will use journal-based self-assessment as an alternative to the 10-year exam. Over the course of 3 years, diplomates will be required to read 30 articles chosen from a broad library of approved articles. After each article, a diplomate will complete a short online quiz. If they answer 4 of 5 questions correctly, they will have successfully completed one article. Child psychiatrists who are recertifying during that time and also meet the same conditions will also be able to participate but would not be permitted to double-count articles. No other subspecialties will be included in the pilot, although ABPN has stated that if the pilot goes well, they will expand this program to other subspecialties as quickly as possible.
Substance abuse education: The APA continues to engage learners each month through its SAMHSA-funded Provider’s Clinical Support System for Medication-Assisted Treatment (PCSS-MAT) webinar series. APA submitted approximately 12 online education resources to be included in a nationwide campaign led by the AMA to increase clinician knowledge regarding the opioid epidemic. The APA’s role has expanded within the PCSS-MAT program to include providing technical assistance to a primary care practice in Pennsylvania as they seek to implement MAT in their clinic. An updated version of the buprenorphine training program launched in January 2018 and is available for free to resident-fellow members. Additionally, APA will be joining the State Technical Assistance Team Education and Support Coalition as part of a SAMHSA-funded grant to AAAP. APA will provide 32 learning collaboratives over the next 2 years as part of this grant.
Year-end summary from the Office of Continuing Medical Education (CME): In 2017, the Office of CME issued 350,000+ CME credit/hours of education from across its live, online, journal, and district-branch CME programs. Over 34,200 users received education or claimed credit through the APA’s learning management system.
Comments to the Accreditation Council for Graduate Medical Education (ACGME): The APA submitted comments to the ACGME on the importance of diversity in residency training as part of the ACGME’s revision of its Institutional Requirements policies.
The Medical Mind Podcast: This podcast channel features a number of 10- to 15-minute audio episodes focusing on innovation in mental health care. The podcast channel was started within the Division of Education as part of the SAMHSA-funded PCSS-MAT grant, with the goal of providing a more narrative exploration of substance use disorders and innovative approaches to treatment. Episodes can be found online at
https://www.psychiatry.org/psychiatrists/education/podcasts/the-medical-mind-podcast or in the Apple “Podcasts” App by searching The Medical Mind.
Joint Sponsorship Program for CME: In 2016, the APA’s Board of Trustees approved an expansion of the Joint Sponsorship CME program. APA is currently using the expanded program to support our affiliated groups. APA has seen increased participation by district branches in this program, numerous applications for affiliate groups, and new outside groups such as the New York City Department of Health and Mental Hygiene.
Course of the month promotion: In 2015, APA began a free CME opportunity for all APA members. A new, monthly online course was promoted to members, which they would be able to complete for Category 1 CME credits. To date, there have been more than 6,500 individual course registrations.
Diversity
2018 APA/APAF Fellowship application cycle: The 2018 APA/APAF Fellowship application cycle ended with 212 application submissions. The number of submissions increased 23% from the previous cycle. Two of the five states that have never had an awardee were represented (Oklahoma and North Dakota). Ten applications were from the nation’s three psychiatry residency programs at Historically Black Colleges and Universities (HBCUs). The Division of Diversity and Health Equity (DDHE) is further evaluating application data and overseeing the award selection process. In addition, we are continuing to reach out to district branches and state associations to help connect fellows to become more involved in leadership at the district branch level. Discussions will also be held at the Annual Meeting with district branch presidents and executive directors to further work on including new fellows and post-fellows into leadership.
SAMHSA Minority Fellowship Programs grant renewal: DDHE submitted an application to renew funding of the SAMHSA-funded Minority Fellowship Programs (MFP) for years 2018 through 2023. APA expects to be notified of the status of the application in the summer of 2018.
APA Response to the DHHS Draft Strategic Plan for FY 2018–2022: DDHE collaborated with APA’s Policy, Programs, and Partnerships (PPP) and the Caucus of Lesbian, Gay, Bisexual, Transgender, and Questioning/Queer Psychiatrists to develop a response to the FY 2018–2022 Strategic Plan of DHHS. The strategic plan did not contain strategies to address disparities of minority populations, including LGBTQ.
In the response letter to DHHS’s Acting Administrator, APA stated the following:
[T]o reduce the cost of health care and achieve our goals of creating a healthier nation, the needs of specific populations must be examined and effectively addressed. We urge you to reconsider this omission in the draft DHHS Strategic Plan and include strategies to focus on better access to health services and improved outcomes for minority populations, including LGBTQ, in the final version of the DHHS Strategic Plan for 2018–2022.
Climate change and disaster mental health: CME module: The module was developed as a follow-up to the APA Community Mental Health Disparities Program on “Climate Change and Mental Health” that occurred at the 2016 IPS meeting in Washington, DC. The purpose of the module is to increase awareness about climate change and its impact on mental health, especially in vulnerable populations.
Conversations on diversity: DDHE sponsored its fifth session of Conversations on Diversity at IPS in New Orleans on October 21, 2017. The session included small breakout groups of APA leadership and members from various cultural backgrounds who strategized ways to increase diversity and inclusion within the organization and reduce mental health disparities among underserved patient populations.
Psychiatry residency programs at HBCUs: DDHE visited three of the four psychiatry residency programs at HBCUs throughout the months of October and November. The purpose of the visits was to inform psychiatry residents at HBCUs about APA and funding opportunities through APA/APAF Fellowship programs. The effort also supports an aspect of APA’s fourth strategic initiative: supporting and increasing diversity within APA.
APA/APAF medical student grants: The purpose of APA/APAF medical student grants is to reduce mental health disparities by providing experiential learning to medical students interested in serving underserved and minority communities. The travel grant allows for medical students to witness organized psychiatry at work and learn more about the field.
Cultural Competence and Inclusive Excellence Summit II: APA collaborated with General Motors and the Ohio State University Wexner Medical Center to sponsor the Cultural Competence and Inclusive Excellence Summit II at APA headquarters on September 25–26, 2017.
Other Member Updates
The American Journal of Psychiatry (AJP): Ned Kalin, M.D., has been selected to be the next Editor of AJP. Dr. Kalin is among the most accomplished biological psychiatrists in the field. His research combines molecular, preclinical animal models, and human functional imaging studies to elucidate the mechanisms underlying the pathophysiology of anxiety and affective disorders. His planned approach for the Journal is to integrate the clinical aspects of the field with an accessible understanding of the translational behavioral science and neuroscience underlying key clinical issues. Dr. Kalin’s tenure officially begins January 1, 2019. We thank Dr. Robert Freedman for his 13 years of dedicated service and for taking AJP to new heights and readership.
The American Journal of Psychotherapy: APA Publishing’s newly acquired psychotherapy journal welcomed Holly Swartz, M.D., as its Editor. Dr. Swartz is recognized internationally for her research focusing on optimizing psychosocial treatments for mood disorders. Her vision for the Journal is to address topics across treatment modalities, age groups, genders, races and ethnicities, and diagnoses and serve the international community by curating a vibrant, pluralistic, dialogue about psychotherapy that ultimately will inform clinical care. The Journal successfully relaunched on April 30th with a robust website that included the entire back catalog (back to 1947, heretofore unavailable) as well as new original content.
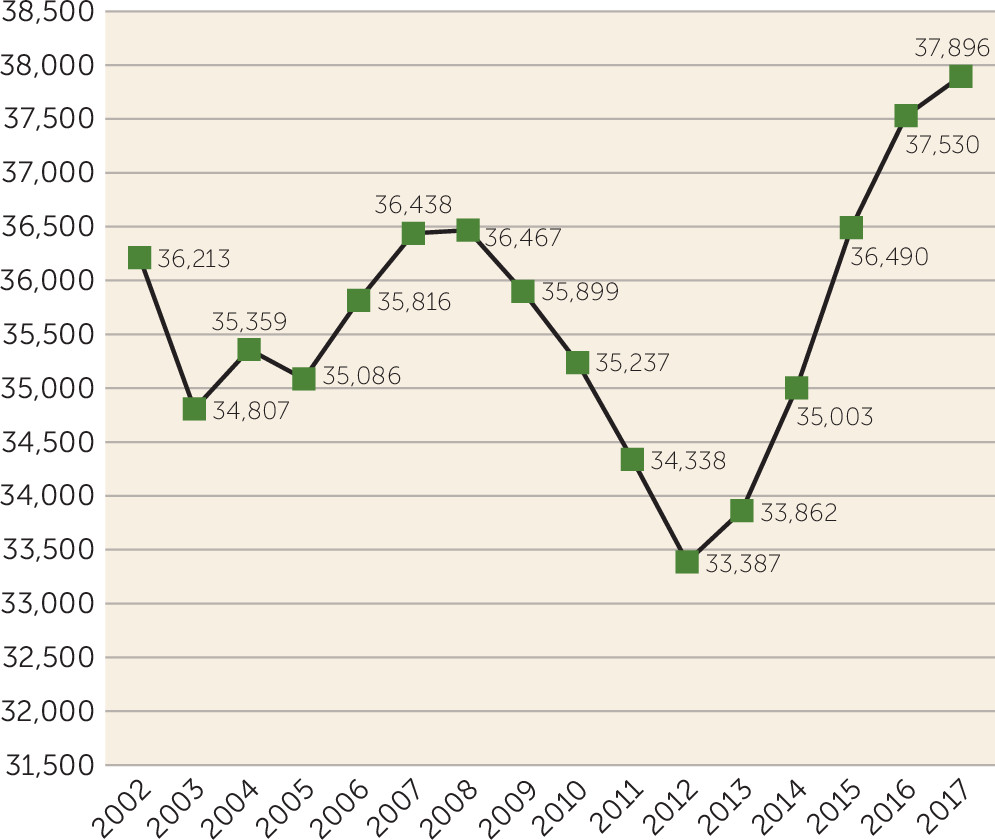
Membership Trending Upward: At the end of 2017, total membership stood at 37,896, which is the highest level in 15 years. Highlights of this trend are shown in
Figure 5.
I look forward to our continued discussions and another year of the APA growing and enhancing our position in the mental health/health care field.
Report of the SPEAKER-ELECT
James R. (Bob) Batterson, M.D.
It has been an honor to serve as your Speaker-Elect this past year. Theresa Miskimen—the Speaker—and I have been pleased to see the activity of the Assembly, with a total of 40 action papers in the two Assemblies in our term. Discussions have been brisk between meetings on current topics, including the Goldwater Rule, parity, marijuana legalization, and improving access to care. The Assembly moved quickly to deal with CMS ligature rules that were released just weeks before the November Assembly. MOC was another issue, where votes were taken as new business due to need for immediate action by our Association.
Actions of the Assembly have been moving through the councils and components of the APA. The Joint Reference Committee (JRC) has been monitoring this movement and receives updates from councils. Action papers over the past year have driven a healthy amount of discussion in the councils and set agendas for related projects. There are also policies that come out of these papers that return to the Assembly and the Board of Trustees for approval.
One highlight for me was when the Assembly approved a paper at the May 2017 Assembly on “Health Care as a Human Right.” This paper was sent to the Council on Psychiatry and Law by the JRC in June 2017 and after review was sent back to the JRC in October, and then to the Board which approved it at the December 2017 meeting. Within 7 months, the idea of a member at a district branch inspired the Assembly, and a significant statement was made by our Association. This is an example of how the Assembly can work. Most papers that have passed the Assembly have taken longer to become policy, as there is more nuance to them and work to do before they are ready for Board approval.
Assembly members gave back to the APA by supporting the APA Foundation and the APAPAC. Last fall, the Assembly held a special fundraiser for the APA Foundation’s efforts for hurricane relief in the Gulf states and Puerto Rico. We raised over $8,000 in the 90-minute event. The total funds donated by members at the Assembly meeting were record-breaking for the Foundation. The APAPAC also raises sizable donations from Assembly members each time we meet.
I have participated in two meetings that I wish to highlight relating to the Assembly:
•
APA-ABPN discussion: This meeting occurs yearly with a few APA leaders, along with Larry Faulkner and a few members of his board. We hosted the meeting this year at the new APA headquarters. Dr. Everett, our President (May 2017–May 2018), made a wonderful presentation on current APA efforts in Burnout, and Dr. Gorrindo, Director of Education at the APA, reported on educational opportunities within the APA that will meet various MOC requirements. Assembly actions about costs and barriers to meeting the requirements were discussed as well.
◦
An important new initiative of the ABPN is the Pilot Project on Self-Assessment with articles that would allow diplomates to not only receive self-assessment CME but also forego the 10-year exam. Participants would have to review 30 articles and answer four out of five questions correctly to be able to forego the exam, and there would be 40 articles from which to choose. This is a significant change for the ABPN. With this project, they will be offering the opportunity for diplomates to choose to learn about and be examined on areas they feel are important to them.
◦
We have ongoing dialogue about fees. They affect our early-career members especially hard, as this is when they take their exams.
•
The Scope of Practice Summit at the American Medical Association: Held in March 2018: This group was formed by a resolution of the House of Delegates, and the APA was a founding member. Representatives of many medical professional organizations and some state associations were present. This 1-day meeting brought to light the many battles that are being fought regarding scope of practice. It was impressive to see how many different professions are pushing in various states to be able to practice medicine or to expand on their current privileges. The issues that face our own profession are not unique. Strategies to successfully challenge these efforts were discussed, and, as could be expected, sometimes obvious arguments about safety do not always work. While I cannot divulge details of strategy that were discussed, below are some objectives that our APA is encouraging:
◦
All APA members should reach out to members of their state legislatures early and often; remind them who you are and make yourself available as their “go-to person” for any mental health issue for which they need more information.
◦
Access to care is one of the most common arguments made for expanding scope of practice. New innovations, including telehealth and collaborative care, are not only better answers to the access problem than expanding scope but innovations such as these are the future of psychiatry.
◦
Working toward systems of care that emphasize the strength of various health professions with opportunities for all to have a pathway to success may decrease scope battles in the future.
This has been a very busy year for me as your Speaker-Elect, with two Assemblies, two additional Assembly Executive Committee meetings, three Joint Reference Committee meetings, and four Board meetings all within this past year. I also had the pleasure of visiting several area meetings. I look forward to my year as your Speaker and will work to build on the work of Drs. Miskimen, Anzia, and Martin and many others before them.