Clinicians, patients, and families are well aware of the pressing need for more effective treatments for depression, and this issue of the Journal is focused on new developments in the treatment of major depressive disorder. That major depression is a worldwide public health problem cannot be overstated. It continues to be a leading source of suffering, disability, and cost. Not only do we need treatments with improved efficacy, a low side-effect burden, and a more rapid onset of action, it is imperative that we also develop the ability to predict individual differences in response to different medications and treatment modalities.
The papers in this issue encompass clinically relevant themes that include: the phenomenology of depression and predictors of treatment response, ketamine maintenance therapy for treatment-resistant depression, a translational animal study focused on ketamine’s mechanism of action, and a study challenging earlier data that have been used to implicate depression-related candidate genes. An insightful and thought-provoking review and overview article by Dr. Alan Schatzberg (
1), a leader in depression and psychopharmacology research from Stanford University, sets the stage for considering these articles. Schatzberg raises important questions relevant to diagnostic criteria for major depressive disorder, predictors of treatment response, and the methodological and experimental design issues necessary for the validation of new treatment approaches. We also have a commentary written by Drs. Myrna Weissman, Milton Wainberg, and Mark Olfson from Columbia University that emphasizes the efficacy of current evidence-based treatments and the importance of assiduously treating our patients suffering from depression (
2). This commentary challenges a recently published viewpoint (
3) suggesting that because of high placebo response rates and “spontaneous recovery,” clinicians should use a “watchful waiting” approach before starting antidepressant treatment.
Three research articles in this issue provide data focused on the prediction of treatment outcomes. The findings from Zisook et al. (
4), from a large Department of Veterans Affairs cohort, address the efficacy of augmentation or switching strategies in relation to severity of illness, presence of anxiety, and chronicity in patients who do not initially respond to an antidepressant. Jha et al. (
5) highlight irritability as a common and frequently underappreciated symptom of major depressive disorder and demonstrate that early treatment-related reductions in irritability are associated with better overall outcomes for depression. Finally, Kaster et al. (
6) point to symptoms and demographics that are associated with a more successful outcome for patients treated with dorsolateral repetitive transcranial magnetic stimulation. Danny Pine, co-chief of the National Institute of Mental Health Emotion and Development Branch and a deputy editor of the
Journal, contributes an editorial on the Jha et al. article that takes a deeper look into how we can conceptualize irritability occurring in major depressive disorder as well as the value in thinking about irritability from a developmental perspective (
7).
Two exciting articles in this issue are focused on the molecular underpinnings of depression and its treatment. In an article with very important implications, Border et al. (
8) systematically analyze large existing data sets from genome-wide association studies and conclude that there is a lack of evidence to support the involvement of 18 candidate genes that, in smaller published studies, were associated with depression per se or with a gene-by-environment interaction relative to developing depression. I note that we have purposefully included a molecularly focused translational animal model study in this issue to complement a ketamine maintenance treatment study by Phillips and colleagues (
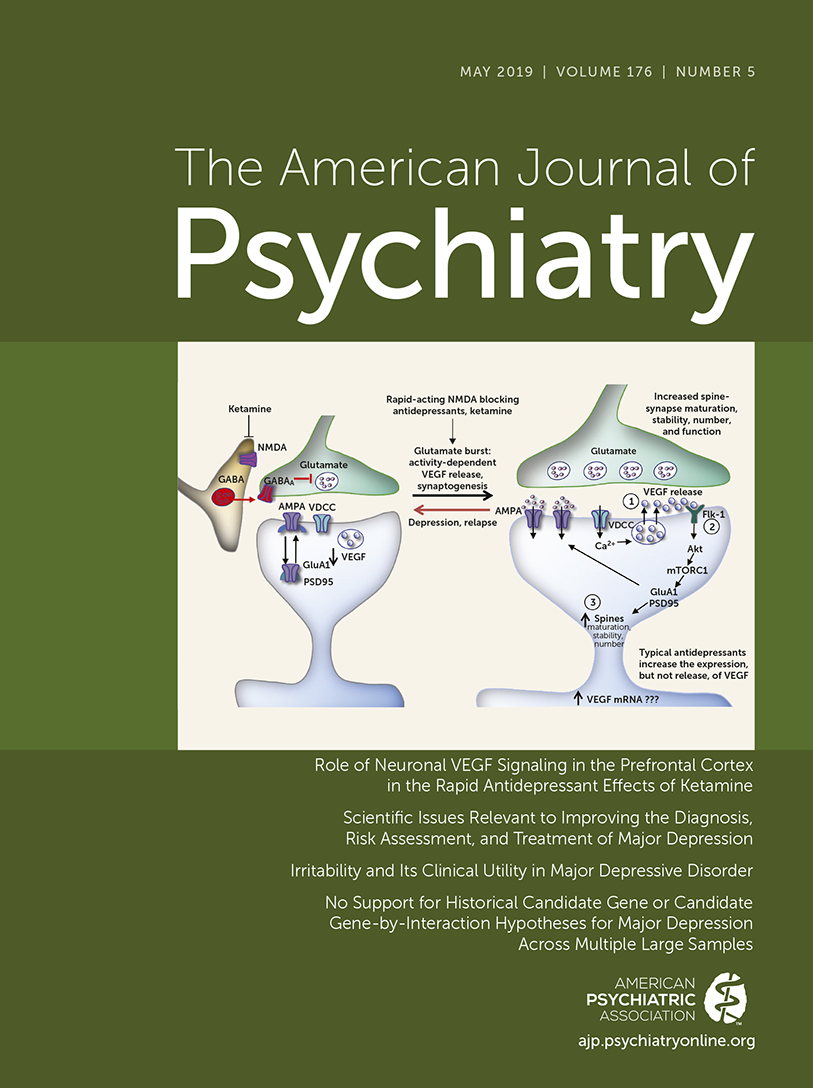
9). Here, Deyama et al. (
10) present data from a series of elegant rodent experiments that address brain region–specific molecular mechanisms underlying ketamine’s rapid antidepressant effects. These authors show in rodents that the vascular endothelial growth factor (VEGF) system in the prefrontal cortex is involved in mediating the antidepressant-like actions of ketamine. In an editorial on this article, Margaux Kenwood, a neuroscience Ph.D. candidate student, along with other members of my laboratory, provides a context for these preclinical data in relation to the value of animal models as they relate to clinical studies and the development of novel treatment strategies (
11).
In the article by Phillips et al. (
9), clinical concerns related to maintaining the efficacy of ketamine treatment are addressed. This is a vital issue because while ketamine has a rapid onset of action, it is unclear how antidepressant responses can be maintained with ketamine treatment. In a group of patients with treatment-resistant depression, the authors present data suggesting an effective strategy for increasing and maintaining ketamine responsivity over time. In Schatzberg’s overview, he comments on the challenges in understanding ketamine’s mechanism of action as well as critical clinical trial design issues that are important to understand in interpreting the data from the Phillips et al. article.
This issue of the Journal provides our readers with clinical and research information directly relevant to improving the care of patients with major depressive disorder. The authors of these papers are to be congratulated for their commitment to their research endeavors focused on understanding and better treating depression. As our scientific advances allow us to better understand the mechanisms underlying depression, the hope is that this will inform the development of interventions that are not only more effective but also permanently change depression-related neural circuit alterations. It would be wonderful, if someday, hopefully not too far in the future, we could help our patients not only get better acutely but also provide them with long-term symptom resolution that would obviate the necessity for ongoing treatment.