To the Editor: We appreciate the opportunity to read and respond to the insightful letter from Drs. Woods, Yung, McGorry, and McGlashan, leaders in this field of research. They point out two possible confounding effects of our analyses, which concluded that the effect of duration of untreated psychosis (DUP) on long-term outcomes in schizophrenia was explained by lead-time bias. The first point concerns the sample selection, and the second concerns the level of treatment the patients received. We discuss these two points in turn.
Dr. Woods and colleagues note that including only those individuals with a diagnosis of schizophrenia at the last observation could have biased the sample toward poor outcomes. However, we note that the relationship between DUP and outcomes has been largely observed among those with schizophrenia (
1–
3). Indeed, fitting the same multilevel spline models to data from individuals in the Suffolk County Mental Health Project cohort with diagnoses other than schizophrenia found no effect of DUP on either mean psychosocial function or trajectories of psychosocial function.
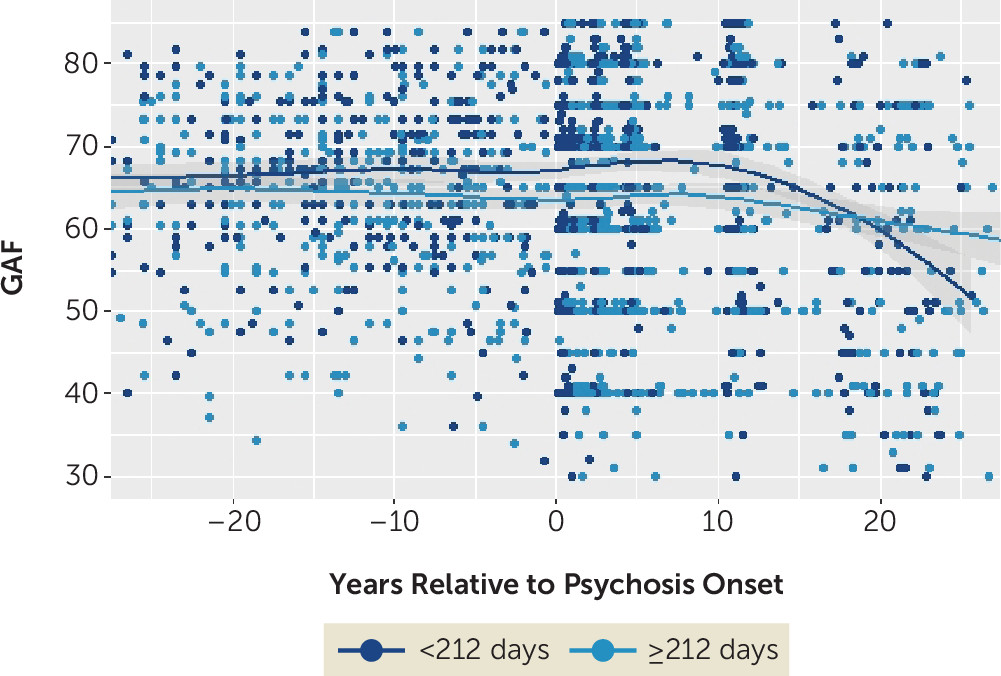
Figure 1 depicts a LOESS plot of trajectories as measured by the Global Assessment of Functioning Scale (GAF) as a function of DUP dichotomized at the median of 212 days, which shows the overlap between these groups.
Second, we note that previous studies of this cohort have documented substantial diagnostic shifts, such that by 24 months after first admission, more than 20% of those diagnosed with schizophrenia shifted into this group from other diagnostic categories (
4). By the 10-year follow-up, more than 45% of this group included individuals who had been reassigned from other diagnostic categories (
5). As of the 20-year follow-up, this number had reached nearly 50%. Approximately 28% of this group had a baseline diagnosis of other psychotic disorder, while 10% were originally diagnosed with bipolar disorder, 20% with major depressive disorder, and 2% with substance-induced psychosis. For this reason, those with a last available diagnosis of schizophrenia have shorter DUPs (median days, 310) and better baseline psychosocial function (mean GAF score, 52.52) than those with a baseline diagnosis of schizophrenia (median DUP days, 358; mean GAF score, 48.93; both p values <0.01), but not worse outcomes (20-year GAF scores were 52.52 and 48.93, respectively; p=0.33). In sum, selecting the sample based on the last available diagnosis captured a group of individuals with diverse initial presentations and a broad range of DUPs and did not create a bias toward poor outcomes.
Dr. Woods and colleagues suggest that halting decline may require interventions more potent than those received by the Suffolk County cohort. The treatment received by this cohort is primarily pharmacological and is not comparable to the vocational rehabilitation, family education, and individual therapy implemented in NAVIGATE (
6), OnTrackNY (
https://www.ontrackny.org), and a number of other early intervention programs. Such comprehensive coordinated specialty care programs may be more effective—although long-term follow-up of these cohorts is needed.
However, we do not find evidence that the Suffolk County cohort is atypical, as Dr. Woods and colleagues suppose. Before adjustment for lead-time bias, the association between DUP and psychosocial function was moderate in size (Cohen’s d=0.75, p<0.001). Meta-analytic evidence indicates that outcomes in the Suffolk County cohort are consistent with other representative samples with first-admission psychosis (
7). Therefore, although the treatment is not equivalent to that received by patients in clinical trials, it is representative of treatment received by patients with first-admission psychosis. As such, this cohort is important for understanding the current state of intervention for schizophrenia in the community.
In sum, we believe that our sample is an informative one in which to evaluate the association between DUP and long-term outcomes. Results support our finding that lead-time bias confounds the association between DUP and illness course in schizophrenia.