Exposure to trauma is highly common worldwide (
1), ranging from interpersonal assaults to disasters, wars, and pandemics. Ensuing trauma-related psychopathology is common, broad, and diverse. Although a history of traumatic events is found across a spectrum of psychiatric disorders, including anxiety (
2), depressive disorders (
3), bipolar illness, and schizophrenia (
4), posttraumatic stress disorder (PTSD) (
5) is the most researched trauma-related psychiatric disorder over the past four decades. A 2013 World Health Organization study of 21 countries estimated that 3.6% percent of the world’s population suffers from PTSD (
6). In the United States, the lifetime prevalence of PTSD among adults is estimated at 6.8% (
6), with a current past-year prevalence of 3.5% (
2). Military personnel, facing higher risk for trauma exposure through combat, injury, captivity, and sexual assault (
7,
8), face even higher rates, reaching up to 30%.
Despite extensive research, available psychotherapies and pharmacotherapies for PTSD have shown only limited benefits. For example, for prolonged exposure—the gold-standard PTSD treatment—nonresponse rates range from 25% to 60%, with dropout rates reaching 50% (
9,
10). Similarly, few medications have been found to ameliorate PTSD, with small effect sizes (
11). Military veterans, a highly trauma-exposed population, benefit even less from existing treatments and have higher attrition rates (
12).
The cause of limited treatment efficacy in PTSD may lie not only in the treatments themselves but in the heterogeneity within the diagnosis of PTSD. PTSD is currently defined by exposure to a wide variety of traumatic events and by a broad constellation of physical, affective, behavioral, and cognitive symptoms. Improving the diagnostic specificity of PTSD would yield more homogeneous patient samples and increase the likelihood of identifying clinically meaningful neurobiological markers, which could in turn serve as objective, measurable targets for novel and specific treatments. In trying to address the problem, functional neuroimaging studies have become central to efforts to characterize neural markers of PTSD. Commonly they include task-based functional MRI (fMRI), aiming to elucidate brain regions that are differentially activated during processing of affective and cognitive stimuli, and resting-state fMRI (rs-fMRI) experiments, aiming to identify brain-wide networks that are altered in psychiatric disorders. This review covers progress in these areas, highlighting current limitations and ways to overcome them.
Task-Based fMRI of Fear Processes in PTSD
Heightened fear response has been considered a central feature of PTSD. Translational neuroscience research has mainly focused on fear-learning processes as an important set of mechanisms (
13). At the core of this interest is the question of why some people develop difficulties distinguishing between safe and dangerous cues in the aftermath of trauma exposure.
This line of work was inspired by Pavlov’s famous classical conditioning experiments (
14), exploring processes by which pairing an aversive unconditioned stimulus (e.g., an electric shock) with a conditioned stimulus (e.g., a red light) could generate a conditioned response (e.g., freezing). In humans, a wide range of behavioral and neuroimaging paradigms have been used to explore fear learning and extinction, both among healthy, untraumatized individuals and among trauma-exposed individuals with and without PTSD (
15). Such paradigms usually comprise an acquisition (i.e., conditioning) phase followed up by an extinction learning phase, during which the conditioned stimulus (e.g., the red light) is repeatedly presented without the unconditioned stimulus (e.g., the shock) until expression of the fear response is diminished. In some cases, after some time has elapsed, the return of fear is assessed in a subsequent extinction recall phase. Enhanced fear response to the conditioned (CS+) and unconditioned (CS−) stimuli during fear conditioning, as well as reduced extinction learning (e.g., enhanced fear response to the CS+ during extinction), were found to characterize patients with PTSD compared with trauma-exposed healthy control subjects and/or healthy individuals with no trauma exposure (
16–
26). Research has also implicated pathological fear conditioning as preceding the onset of posttraumatic stress symptoms, reflected in stronger fear responses to the CS+ and reduced extinction learning (
27–
30).
In healthy humans, extensive research has documented relatively consistent patterns of brain activation in subjects undergoing fear conditioning and extinction tasks. Conditioning was found to be associated with increased activation of the amygdala, the dorsal anterior cingulate cortex (dACC) and the anterior insular cortex (
31,
32). Extinction, which involves new learning (rather than unlearning of acquisition), engages the medial prefrontal cortex (mPFC) and the ventromedial PFC (vmPFC) during both extinction learning (
33) and recall (
34), which has been interpreted as reflecting inhibitory processing within the extended fear network (
35,
36). The insular cortex and dACC are also activated during extinction learning and extinction recall (
33).
The exploration of fear-related processes has also been enriched by seminal research focusing on cellular and molecular mechanisms of extinction. For example, the roles of brain-derived neurotropic factor (BDNF) and its receptor, TrkB, were documented in relation to memory formation associated with conditioning and extinction (
37,
38). Another line of research has translated basic findings to the clinic. For example,
d-cycloserine, a partial agonist at the
N-methyl-
d-aspartate (NMDA) receptor, has been shown to enhance extinction of fear memories in rodents (
39), leading to initial testing of its role in humans undergoing extinction paradigms (
40). These efforts have mostly been validated as proof of concept but have yet to yield consistent clinical benefits.
Taken together, fear processing in healthy humans involves the dorsal and ventral medial prefrontal cortex, including anterior cingulate cortex (ACC) subregions and the insula, hippocampus, and amygdala, comprising a large fear-related network responsible for both learning and memory processes. Research into both this neural circuity and its cellular and molecular mechanisms has enhanced our knowledge of fear processing, serving as a stepping stone toward a greater understanding of fear-related disorders (
13) and toward the ultimate goal of identifying reliable, specific treatment targets and developing better treatments.
Patients with PTSD are behaviorally hyperresponsive to environmental threats, consistently showing persistent and exaggerated threat responses in conditioning research paradigms, even in the presence of safety cues (
15). Studying neural activity during fear learning and extinction processes has the potential to clarify mechanisms underlying these behaviors. A series of fMRI studies reported reduced activation of the mPFC, ACC, amygdala, and hippocampus during both conditioning and extinction learning in PTSD (
15,
41,
42). A meta-analysis of emotional processing studies, including differential cue-conditioning paradigms, reached similar conclusions, finding that patients with PTSD showed hypoactivation of the amygdala, vmPFC, dorsomedial PFC, ACC, and anterior hippocampus when compared with patient comparison subjects (with social anxiety disorder or specific phobia) during a variety of emotional processing tasks (
31). However, other PTSD studies have yielded mixed results. During conditioning, some have reported reduced amygdala activation (
43), whereas others have reported no alterations in amygdala activation (
23,
44,
45). Moreover, increased amygdala activation during extinction learning (
23) and extinction recall (
44) have also been reported in some studies (
45).
Mixed results involved other regions as well. For example, heightened dACC activation during extinction recall has been reported in some studies (
23,
45), whereas others have implicated middle cingulate alterations (
44). Also, lower vmPFC and hippocampus activation found during extinction recall in one study (
23) were not replicated in a subsequent study using the same fMRI task (
45). While several studies have pointed to no alterations in amygdala activation (
23,
44,
45) or reduced amygdala activation (
43) during conditioning, in a recent meta-analysis of fMRI studies (
46) we found that PTSD patients demonstrated increased fear circuit activation, including the amygdala, regardless of the experimental phase studied—conditioning, extinction learning, or extinction recall. Specifically, amygdala hyperactivation was found during conditioning, followed by failure to reduce this activation during extinction learning and extinction recall. This pattern was accompanied by failure to activate the hippocampus and deactivate the parahippocampal gyrus during extinction learning, suggesting that PTSD patients exhibit higher threat arousal throughout the experimental phases.
Overall, studies in healthy humans have documented relatively consistent patterns of brain activation in subjects undergoing fear conditioning and extinction tasks. Based on diverse paradigms, a wealth of knowledge presents exciting promise for a better understanding of fear- and anxiety-related disorders (
13), and as such was the basis for the establishment of the Research Domain Criteria (RDoC) project at the National Institute of Mental Health (
47). In PTSD, however, results are less encouraging. While there is general agreement that PTSD patients exhibit difficulties in distinguishing between safe and threat cues in the aftermath of trauma exposure, absence of consistent findings regarding the underlying circuitries and mechanisms hinder our understanding of the pathophysiology of PTSD and preclude the identification of objectively measured treatment targets that would advance clinical research and personalized care.
Resting-State fMRI Connectivity in PTSD
Task-based fMRI methods have been criticized for limited test-retest reliability and failure to replicate findings (
48), two features crucial to trusting emerging scientific results (
49). This is especially problematic in task-based fMRI research when a) sample sizes are small, b) data per participant are limited, c) a single task rather than a composite task measure is used, and d) brain activity is assessed in individual brain regions (
50). Conversely, MRI resting-state functional connectivity (rsFC) methodologies have increasingly shown greater reliability when using large-scale connections between distributed brain regions (
51) and when used in big data projects (e.g., the Enhancing Neuroimaging Genetics Through Meta-Analysis [ENIGMA] consortium [
52]) employed across different psychiatric disorders. rsFC has shown relative stability and reproducibility over time, and low performance demand on participants yields high compliance, which minimizes behavioral confounders normally found in task-based fMRI (
53). These features make rsFC particularly suitable for clinical studies, and if it is shown to predict specific outcomes, it has potential for clinical application given its standardization and relatively low cost.
To capture a large range of neural aberrations, applying a network approach to rsFC data may have particular additional advantages. Specifically, the high intrinsic connectivity networks (ICNs) method has the potential to identify functionally distinct brain networks. Because ICNs are identified with data-driven decomposition approaches, their identification is less biased and does not require a priori hypotheses (
54). Research shows that PTSD is associated with abnormalities in a host of ICNs, including the salience network, default mode network, and executive control network as well as in connectivity between them (
42,
55). For example, within the salience network, encompassing the ACC and the anterior insula as its central nodes, studies have found enhanced connectivity between amygdala and insula in individuals with PTSD relative to trauma-exposed and non-trauma-exposed healthy control subjects (
42,
56,
57), suggesting a potential neural signature of hypervigilance (
42,
57). Evidence for decreased connectivity between nodes of the default mode network (e.g., posterior cingulate cortex, precuneus, vmPFC, and hippocampus) has also been found in PTSD (
56,
58,
59), suggesting a putative signature for depersonalization and derealization (
60).
Yet, here too, divergent findings have been reported (
55). For example, within the salience network, connectivity between the amygdala and the dACC has been shown to be higher (
61), lower (
55), or unaltered (
57) in individuals with PTSD compared with control subjects. Both higher (
62) and lower (
58) between-network connectivity between default mode network nodes, such as the posterior cingulate cortex/precuneus and the salience network, has been demonstrated in individuals with PTSD compared with control subjects. Several studies have reported reduced connectivity between amygdala and inferior frontal gyrus, vmPFC, and middle frontal cortex (
61,
62), whereas others found no differences in connectivity between the amygdala and the vmPFC pathway (
55).
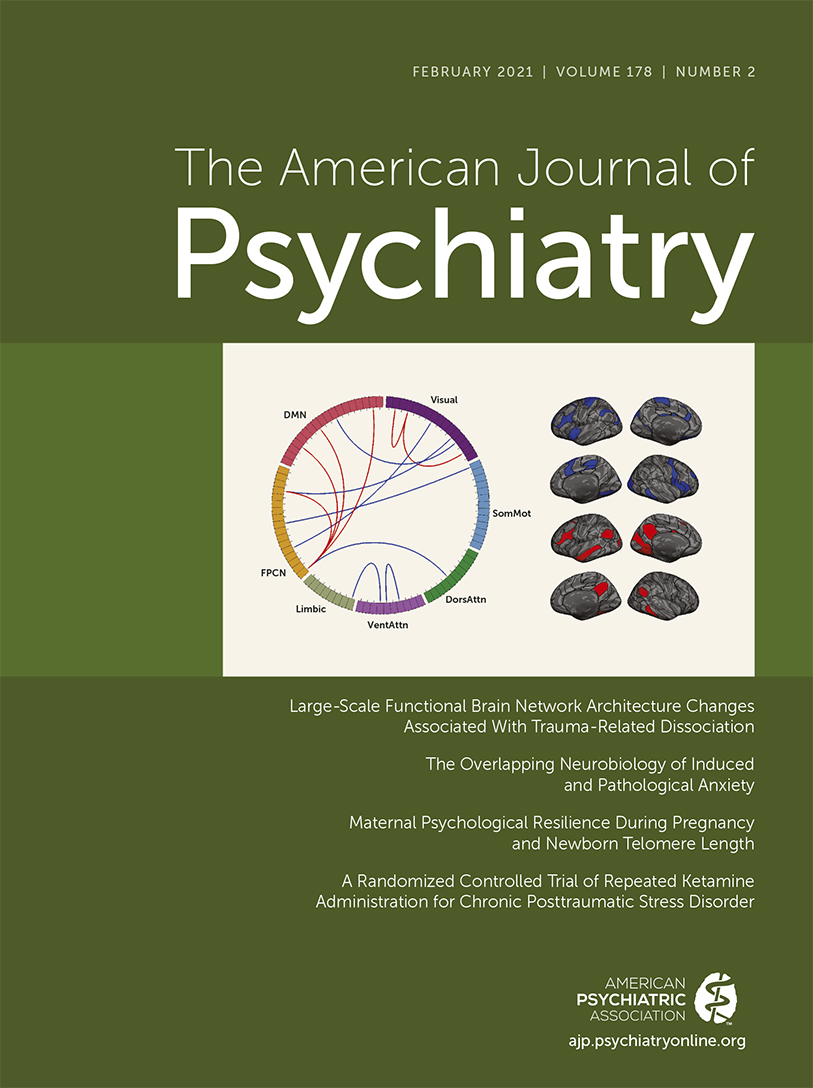
Two recent studies have used innovative methodologies to analyze rsFC data. The first aimed to clarify neural markers of PTSD from trauma-exposed healthy control subjects, and the second sought to subtype PTSD diagnosis. Zilcha-Mano et al. (
63) utilized a support vector machine model, a multivariate pattern recognition machine learning technique well suited for discriminating high-dimensional rsFC fMRI data, to differentiate PTSD from trauma-exposed healthy participants. rsFC data from 103 civilians with PTSD and 76 trauma-exposed healthy participants were used, yielding a 70.6% accuracy rate in discriminating between the two groups, with findings implicating within-network connectivity differences in the executive control network, prefrontal network, and salience network, suggesting increased salience processing at the cost of awareness of internal thoughts and autobiographical memory (
55). Individuals with PTSD also showed decreased connectivity within the executive control network, potentially representing diminished emotion regulation abilities and inability to down-regulate negative emotions (
64). Maron-Katz et al. (
65) applied a data-driven approach to identify PTSD subtypes based on rs-fMRI data. They compared abnormal features in the data from 87 veterans with PTSD and 105 combat-exposed healthy subjects. Two distinct PTSD subgroups emerged: one showing abnormally low connectivity between the visual and sensorimotor networks, the other showing the opposite pattern of abnormally high connectivity between these networks, as well as abnormally low connectivity between these two networks and the frontoparietal control network. This latter group also demonstrated abnormally high connectivity within the frontoparietal control network. Importantly, an additional analysis of EEG assessment at rest confirmed this subtyping.
These efforts to characterize the neural signatures of PTSD via utilization of rs-fMRI connectivity data are potentially promising given the improved stability and reproducibility, low cost, and low performance demand from participants, yielding high compliance, compared with task-based fMRI. Yet, the abundance of inconsistent results, similar to the diversity of findings observed for task-based fMRI studies, is discouraging. Although methodological variation in scanning and scanning parameters and small sample sizes with power limitations may account for some of the observed inconsistency of the neuroimaging findings in PTSD, another contributing factor is the extensive heterogeneity within the diagnostic category of PTSD, making study samples excessively confounded, both clinically and neurobiologically.
Heterogeneity of PTSD
Psychiatric diagnoses, including PTSD, continue to rely on traditional diagnostic systems, defined exclusively by human experiential terms, and neglecting more objective illness markers. For more than four decades, this pervasive categorical approach to diagnosis has been constructed largely from opinions of experts tasked with the development of DSM and ICD diagnostic criteria. While convenient for clinical work and insurance purposes, diagnostic categories to date are not objectively measured neurobiologically valid taxonomies, which are greatly needed to improve treatment efficacy in this age of personalized medicine. As stated earlier, this may be an important reason why treatments work for only small subsets of patients within broad diagnostic categories.
The clinical definition of PTSD combines a multitude of anxiety-related, depression-related, and psychophysiological symptoms people commonly report after trauma exposure. The heterogeneity of PTSD has been amplified by revisions to the diagnosis in DSM-5, increasing the number of symptom clusters from three to four and the total number of symptoms from 17 to 20. With this change, thousands of different possible criterion subset possibilities may constitute a positive DSM-5 diagnosis of PTSD (
66), further diluting the clinical definition of PTSD.
This lack of diagnostic specificity for PTSD has several pitfalls that further undermine PTSD as a distinct diagnostic category. First, it is frequently comorbid not only with anxiety disorders (
67) and depression (
3) but also with schizophrenia (
4) and bipolar illness (
68). Second, as it lacks clear biological margins, PTSD shares biological underpinnings with other disorders (
69). Lastly, lack of specificity complicates our ability to determine the efficacy of new treatments or to track temporal changes in engagement of neural targets. There have, however, been encouraging efforts to address the diagnosis of PTSD by distinguishing PTSD alone from PTSD comorbid with major depression.
Investigating PTSD-MDD as a Potential PTSD Biotype
Comorbidity of PTSD and major depressive disorder (PTSD-MDD) is common and is associated with greater severity and worse clinical outcomes than PTSD alone. Up to 50% of PTSD cases, across multiple samples, also meet diagnostic criteria for major depression (
5). Compared with PTSD alone, patients with PTSD-MDD exhibit greater distress (
70), higher risk of suicidal behavior (
71), greater impairments in neurocognitive functioning (
72), and poorer treatment outcomes (
73). One factor previously linked to treatment outcome in PTSD is emotional engagement (
74). Since depression is frequently associated with emotion dysregulation, low motivation, and flattening of affect, it has been suggested that comorbid depressive symptoms in patients with PTSD may hinder treatment efficacy (
75). Indeed, previous research found that numbing symptoms and anhedonia (
76) predict treatment response in PTSD and that PTSD-MDD patients are more likely to drop out of cognitive-behavioral therapy treatments, including cognitive restructuring and imaginal exposure (
77,
78), to be nonresponders to prolonged exposure (
79), and to need longer treatment in psychotherapy (
80). In summary, a significant body of clinical research suggests that patients with PTSD alone and those with PTSD-MDD may have different clinical needs and hence may benefit from different, well-tailored treatments. No study to date has reported development and examination of novel treatments for patients with PTSD-MDD.
To determine whether specific treatments should be tested for PTSD-MDD, neuroimaging research can be used to examine and elucidate differences between PTSD alone, PTSD-MDD, and major depression alone. For example, a better understanding of the functional complexity of the amygdala in the past two decades (
81) and the distinctive roles its subregions may play in fear processing and response (
82) have raised the possibility that people with PTSD-MDD may show different connectivity patterns of amygdala subregions than people with PTSD alone. Specifically, whereas the basolateral amygdala regulates fear acquisition and evaluation of sensory information (
83) via connectivity with the prefrontal cortex, and hence would be expected to be compromised in PTSD, the centromedial amygdala is connected to the thalamus and the striatum (
84) regions, which are known to play a role in reward processing (
61,
85,
86) and hypothetically could be implicated primarily in PTSD-MDD. Following this line of thought, we recently compared rsFC of patients with PTSD-MDD, PTSD alone, and trauma-exposed healthy control subjects (
87). Patients with PTSD-MDD, compared with the other two groups, exhibited greater decreases in connectivity in both the basolateral amygdala–OFC, a fear-processing pathway, and in two striatal-subcortical pathways that play a role in reward processing: the nucleus accumbens–thalamus and nucleus accumbens–hippocampus. Thus, while patients with PTSD alone exhibited only fear processing disturbances, those with PTSD-MDD showed decreased connectivity in both fear and reward processing pathways, suggesting that PTSD-MDD is associated with multiple, substantial disruptions that include not only deficient fear extinction and consolidation of extinction, but also altered motivational function (
88) and memory formation (
89) during reward processing. Together, this expanded combination of aberrant neural pathways may indicate that exposure-based treatments such as prolonged exposure may not adequately treat patients with PTSD-MDD, requiring the development of combined treatments targeting both the fear and reward tracks.
Additional evidence for differences between PTSD and PTSD-MDD may emerge from exploring intrinsic connectivity networks. Previous research on connectivity abnormalities in major depression (
90–
92) has pointed to hypoconnectivity within the executive control network and between frontoparietal systems and parietal regions of the dorsal attention network, hyperconnectivity within the default mode network, and hyperconnectivity between executive control network systems and regions of the default mode network. Yet, it remains an open question whether PTSD-MDD presents with connectivity abnormalities that are more similar to those observed in major depression alone than to those noted in PTSD alone.
Using innovative methodologies to analyze rsFC data with a larger sample, Zilcha-Mano et al. (
63) conducted a two-phase study. First, they used a support vector machine (SVM) model to compare network connectivity among individuals with PTSD-MDD (N=52) and PTSD alone (N=51). Next, they examined the utility of the identified network connectivity features in predicting treatment outcome in a subsample receiving prolonged exposure therapy. Using SVM with rsFC data achieved 76.7% accuracy in differentiating individuals with PTSD-MDD from those with PTSD alone. Among the most discriminative rsFC aberrations were those related to reward dysfunction (
93). Specifically, individuals with PTSD-MDD compared with those with PTSD alone showed aberrant alterations within the basal ganglia network (BGN), comprising the striatum (subdivided into the caudate nucleus and putamen), globus pallidus, and thalamus (
94), which has been found in previous studies to underlie reward behaviors (
95). Thus, altered BGN connectivity in individuals with PTSD-MDD, as opposed to those with PTSD alone, may underlie impaired motivation (
96). When exploring between-network impairments, altered connectivity was also found between the BGN and other related networks (BGN–dorsal attention network and BGN–salience network) in PTSD-MDD compared with PTSD alone. Lastly, testing the predictive utility of the PTSD-MDD signature revealed that the identified biomarkers discriminating PTSD alone from PTSD-MDD were not significantly associated with response to prolonged exposure treatment, suggesting that prolonged exposure alone, designed to address emotional and cognitive aspects of fear and anxiety, may not be sufficient for patients with PTSD-MDD, and augmentation with treatments addressing the reward circuitry should be considered.
Addressing diagnostic heterogeneity via detection of PTSD biotypes may reduce inconsistencies between studies and eliminate excessive noise and would likely improve effect sizes of clinical trials. The subtyping of PTSD diagnosis may require that current algorithms for evidence-based therapies for PTSD be transformed. For example, if a PTSD-MDD biotype with substantial corticolimbic dysregulation is further validated, PTSD-MDD patients may particularly benefit from treatments with the potential to activate reward circuitry (e.g., dopaminergic medications), either alone or in combination with exposure-based treatments.
The Promise of Big Data
Worldwide collaborations aiming to assemble big data projects hold great promise for improving our understanding of PTSD, refining its neural signatures, and using them to improve mental health care. Current projects, such as the ENIGMA-PTSD consortium, a global alliance of over 1,400 scientists across 43 countries (
52), have the capacity to utilize large-scale data sets (e.g., 3,000 multimodal scans) and worldwide expertise in computational and machine learning methods to address key shortcomings of previous research: small sample size, limited replicability, reliance on task-based fMRI only, and top-down approaches. For example, while analysis of rsFC data is ongoing, recent ENIGMA reports have confirmed the central role of the hippocampal structure in PTSD by identifying disrupted white matter organization measured by lower fractional anisotropy in the tapetum region of the corpus callosum (
97) and a smaller hippocampal volume (
98).
Big data projects will not only improve statistical power and reduce noise but also will facilitate the development of new models and their testing in independent samples, while using bottom-up, data-driven analytic approaches. Such approaches may clarify more reliable and replicable neural signatures of PTSD that can be used as novel treatment targets for current and future treatments. Big data can also help us understand the role of sex as a biological variable not only in the risk for PTSD but also in its neural function (
99), further facilitating treatment selection and improvement. Lastly, big data research can be harnessed to help us understand the heterogeneity of PTSD and discern novel subtypes, exploring the role of genetic variants in regulating the function of circuits and examining the relationships between neural markers and clinical symptoms, which eventually may contribute to the homogeneity of the diagnosis.