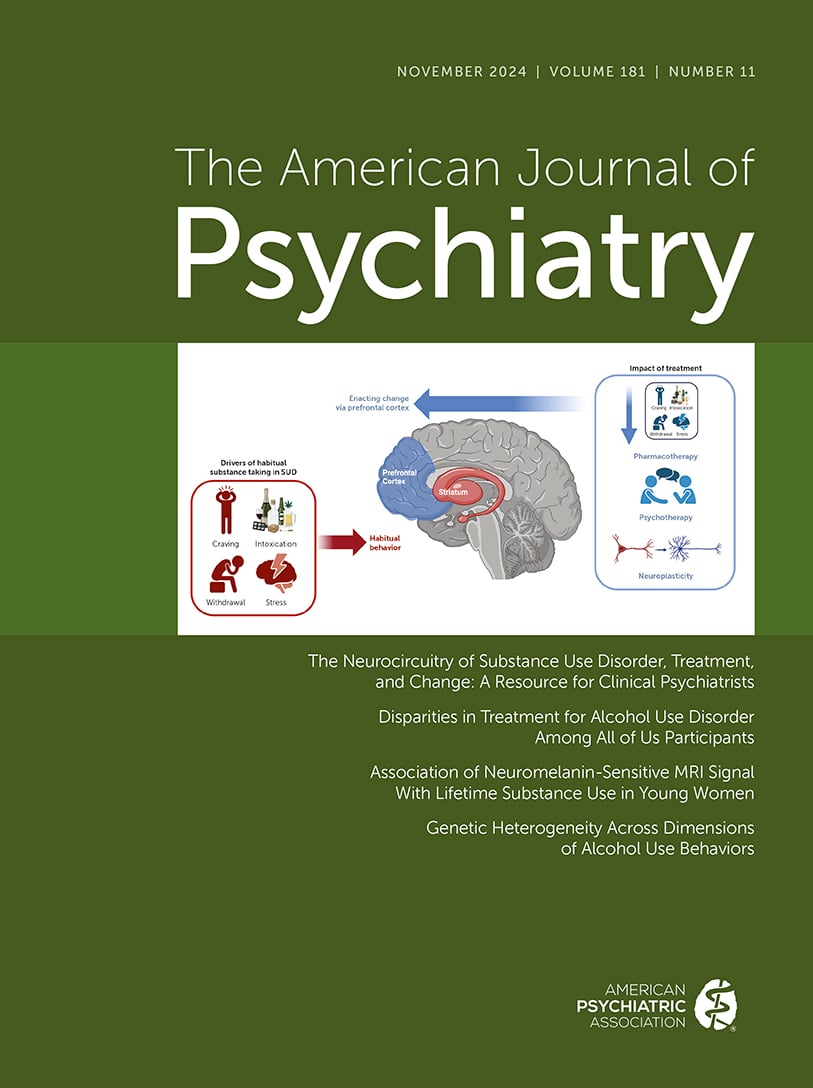
Substance use disorders (SUDs) are a significant public health challenge, impacting physical and mental well-being, academic and professional achievement, and interpersonal relationships. Adolescence is a significant period of neurodevelopment and a time in which individuals typically initiate substance use, leading to subsequent peaks in SUD rates in early adulthood, with over 27% of young adults ages 18–25 years reporting at least one SUD in 2023 (
1). Developmental plasticity at these ages may create a heightened window of vulnerability for the onset and escalation of problematic substance use behaviors, which generally follow a prototyped staging: exposure typically begins with binge use and intoxication, followed by withdrawal, and ultimately craving (preoccupation/anticipation), often in a repeating cycle (
2,
3). However, while human and animal studies have provided important insights into the mechanisms underlying this process, the lack of available noninvasive biomarkers has been an impediment to clinical translation.
The neurobiological basis of the addiction cycle has been extensively linked to the mesocorticolimbic dopamine (DA) system. Dopaminergic projections from the ventral tegmental area (VTA) of the brainstem to the nucleus accumbens (NAcc) as well as various regions of the prefrontal cortex (PFC) are central to the etiology and symptomatology of SUDs. Similar to natural rewards, addictive substances modulate dopaminergic activity in the NAcc (
4), which regulates reward expectation, motivation, and feelings of pleasure (
5). Pharmacologically induced increases in extracellular DA release are thought to play a critical role in motivational processes such as the enhancing and reinforcing properties of substances and substance-related cues (
3) and the formation of reward-related associations that regulate future substance use behavior (“incentive salience”). Like the NAcc, the PFC receives dense dopaminergic projections from the VTA, and increases in DA release contribute to PFC-mediated aspects of goal-directed action selection (
5), which may contribute to overlearning of drug-related cues and overvaluation of drugs relative to other goals (
3). Both the NAcc and PFC, as well as circuit-level interactions between these regions, undergo substantial maturation from adolescence into young adulthood (
6,
7) and are sensitive to repeated substance use, which can induce neuroplastic changes that contribute to adaptations in motivational drive (
8).
In adults, positron emission tomography (PET) studies have demonstrated enhanced DA release in response to several classes of drugs—including stimulants, nicotine, and alcohol—with the magnitude of the DA response related to the degree of “high” experienced (
4). In contrast, studies of chronic substance use on dopaminergic signaling have largely suggested
hypodopaminergic function (
3,
4), with dependence associated with reductions in striatal D2/D3 receptor availability, striatal DA release, and DA synthesis capacity (
2). Similar effects have been observed within prefrontal cortical areas such as the orbitofrontal cortex and the cingulate gyrus (
3,
4), potentially reflecting long-term dysregulation of top-down control mechanisms over striatal DA. In the context of brain measures that index cumulative DA function, these findings make distinct predictions: measures sensitive to drug-related DA release may be elevated following repeat use, while chronic DA
hypofunction may predict depression of DA markers. Further, these may not be mutually exclusive but instead reflect different stages of addiction, with initial elevation of DA responses (during binge/intoxication) followed by DA reductions during chronic stages. These predictions are further complicated by the possibility that individual differences in DA function precede use by conferring risk (i.e., predisposition) for drug-seeking behaviors. However, the lack of noninvasive biomarkers sensitive to dopaminergic physiology has constrained efforts to resolve these hypotheses.
To overcome these limitations, Perlman et al. (
9) leveraged MRI-based measures of brainstem neuromelanin (NM). Neuromelanin is a dark pigment found primarily in the brainstem that forms in catecholaminergic neurons largely through the oxidative polymerization of DA and noradrenaline (
10). NM accumulates when there is DA production and release that exceeds presynaptic reuptake (
11), supporting inferences that higher levels of NM reflect increased cumulative DA release (
12). It is important to note that NM binds with iron to form a paramagnetic compound that can be readily detected through specialized magnetic resonance (MR) sequences (
13), suggesting the possibility of a noninvasive marker of brainstem DA neurobiology. While NM has historically been used to localize and segment visually apparent subregions of the substantia nigra (
14,
15), a key advance, including from this research group, has been to leverage quantitative measures of NM to assess DA neurophysiology within brainstem regions including the VTA.
Using this approach, Perlman et al. identified altered levels of brainstem NM associated with the degree of substance use in a young adult cohort, with greater lifetime substance use associated with increased NM. It is interesting that this association was driven by subregions with high levels of NM signal, particularly within the VTA, underlining a key role of this region’s DA projections in substance use behaviors. The specificity of these associations, which were not present when considering full anatomical regions, suggest a high degree of heterogeneity in the extent to which DA projections may contribute to drug seeking and addictive behaviors.
Perlman et al.’s study targeted young adults (ages 20–24) in relatively early stages of substance use but spanned a wide range of substance use severity. This included substantial representation for those without demonstrated patterns of problematic substance use; 60% of participants included in the study did not meet criteria for any SUD. The pattern of results reported, with increases in NM associated with greater lifetime substance use, may thus support a model in which increased substance use is associated with elevated indices of lifetime cumulative DA function from repeated exposure to drugs of abuse. One possibility is that since NM accumulation occurs when DA release exceeds the capacity for presynaptic reuptake, episodes of binge use and intoxication may result in high levels of cytosolic DA, which may be particularly effective in driving NM accumulation.
Given the cohort characteristics, the impact of longer-term regular substance use on markers of NM accumulation remains an open question. Past characterizations of NM in substance use have produced conflicting results, possibly reflecting the differential pattern of results expected early in substance exposure—which may be dominated by drug-related elevations in NM accumulation—from later in the addiction cycle, when DA hypofunction may lead to an overall suppression in cumulative indices of DA. Continued studies tracking individuals over time, and across stages of addiction, will help elucidate whether these associations between NM and substance use vary as individual progress through addiction stages.
To date, most studies in humans have been conducted in adults and thus have not addressed whether dopaminergic alterations may reflect a preexisting vulnerability marker, rather than a long-term consequence, of substance use on dopaminergic structure and function. For example, an alternative interpretation of the present results is that individual differences in dopaminergic physiology may confer risk for escalation to more compulsive or problematic substance use (
8,
16) rather than simply reflecting cumulative exposure. Since few neuroimaging studies of substance use in humans have longitudinally investigated drug-naïve youths (i.e., assessing substance use
initiation), these hypotheses remain largely untested (
17). MRI-based NM (NM-MRI) is a non-invasive measure that makes it ideal for such studies: unlike PET, which provides a direct measure of DA but necessitates radiation exposure during acquisition, NM-MRI is easily acquired in pediatric populations and can be acquired repeatedly without concerns of cumulative radiation exposure. These properties make NM-MRI ideal to disentangle hypotheses of the role of DA in substance use, including through longitudinal studies beginning prior to initiation. Such longitudinal study designs have recently been applied through several large-scale developmental neuroimaging studies, including the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) study (
18) and the Adolescent Brain and Cognitive Development (ABCD) study (
19). Although these studies did not include measures of brainstem NM, integrating NM-MRI in similar future longitudinal neuroimaging studies of youths will help to begin to address these questions.
Perlman et al.’s results further reinforce the need to consider sex-related differences in the underlying neurobiology of SUDs. Post-hoc analyses indicated that NM-substance use associations were predominantly observed among female participants. Prior characterization of potential sex differences has been hampered by study designs, particularly in animal research, which do not adequately sample across sexes in order to address shared and distinct biological mechanisms (
20). The cohort presented by Perlman et al. drew from an existing study of female participants, and despite additional data collection among male participants, the final cohort remained unbalanced (118 female and 31 male participants). Thus, while the results raise the possibility of sex-specific DA contributions to substance use, further work is needed to determine if this pattern of results reflects power of the available cohort or a true divergence of mechanisms.
Interpretation of these findings depends critically on understanding the precise mechanisms of NM accumulation, and ongoing work to better characterize the sensitivity of NM-MRI to different aspects of DA function is crucial to further understand its utility as a potential clinical biomarker or mechanistic index of DA for substance use research (
21). For example, phasic and tonic DA release may play critical and distinct roles in the etiology of SUDs (
22,
23), but how these aspects of DA function differentially contribute to the measured NM signal is unknown. Furthermore, NM is particularly visible in MRI when bound to iron, which itself has been shown to be an indirect marker of cumulative DA availability, particularly in the striatum (
6). More fully characterizing NM-iron interactions is thus critical to better understanding the nature of the NM signal.
Finally, Perlman et al.’s results build upon a growing line of work demonstrating associations between NM and a number of other conditions marked by dopaminergic disfunction, including schizophrenia (
24), Parkinson’s disease (
11), and more (
12). Continued work is thus needed to understand whether NM associations vary across conditions or whether NM represents a transdiagnostic marker of generalized catecholamine system integrity (
25). These results and remaining open questions highlight the exciting potential of MRI-based NM assessments to advance our understanding of DA function in psychiatric diseases, including substance use disorders.