Children across the United States grow up in vastly different environments that shape their responses to stress and ability to function later in life. Uncontrollable factors such as the neighborhood children are born into can contribute to significant early-life adversity, such as enduring socioeconomic disadvantage or increased risk of violence exposure. In the United States, Black children are disproportionately burdened with these adverse life experiences compared with White children (
1). Current U.S. Census data show that Black households, on average, have a lower median income, lower educational attainment, and higher rates of unemployment and poverty compared with White households (
2). Moreover, research suggests that Black children are more likely to be exposed to trauma and domestic violence and are more likely to have a parent who died, an incarcerated parent, or divorced or separated parents compared with White children (
3–
5). Additionally, research has shown that Black children live in disproportionately disadvantaged neighborhoods and are more likely than White children to be exposed to neighborhood violence (
6,
7). These racial disparities are not random. Rather, they are deep-rooted structural inequalities that result from a history of disenfranchisement of racially minoritized groups (e.g., slavery, segregation) that reinforce themselves through societal norms and practices (i.e., systemic racism) (
8).
Early-life adversity can have lasting negative consequences on mental health in adulthood. Several studies have found positive associations between childhood adversity (e.g., witnessing violence and low socioeconomic status) and prevalence of poor psychosocial and behavioral outcomes later in life, including posttraumatic stress disorder (PTSD), anxiety, and depression, problematic drug and alcohol use, low life satisfaction, suicide attempts and ideation, and perpetration of violence (
9–
15). Thus, the literature demonstrates a strong relationship between adverse life experiences and outcomes such that more adversity experienced in childhood is tied to a greater risk of deleterious mental health outcomes later in life. Further, recent research has emphasized that different types of adversity are associated with distinct outcomes. Specifically, “threat” type adversity (e.g., physical or sexual abuse, witnessing violence) is more often associated with dysregulated emotional responses, whereas “deprivation” type adversity (e.g., poverty, neglect) is more typically associated with language and cognitive deficits (
16–
18).
Previous work has shown that early exposure to adversity (i.e., either threat or deprivation) is associated with structural alterations of brain regions, such as the prefrontal cortex (PFC), amygdala, and hippocampus, which support healthy emotional functioning in response to threat and stress (
19–
21). Therefore, racial disparities in childhood adversity may contribute to race-related differences in the structure of the PFC, hippocampus, and amygdala. The Adolescent Brain and Cognitive Development (ABCD) Study, a large MRI study of childhood development in the United States, may be well-suited to investigate the impacts of racial disparities in adversity on the brain. Previous ABCD Study analyses have found that socioeconomic status (
22) and trauma exposure (
23) are associated with differences in thickness and volume of threat-related brain regions, and that greater neighborhood disadvantage is associated with greater amygdala reactivity in response to faces (
24). Further, socioeconomic status partially mediates the association between race and some aspects of gray matter morphology (
25,
26). Relatedly, previous work outside the ABCD Study found lower neural reactivity to threat within the PFC, hippocampus, and amygdala in Black participants compared with White participants, and these differences were partially attributable to racial disparities in negative life experiences (
27). The literature thus suggests that adversity is associated with differential structure and functional responses within threat-related neural circuitry, although no work that we are aware of has investigated the relationship between racial disparities in adversity and the structure of this circuitry as a whole during childhood. While emergent research has investigated the impacts of racial discrimination on the brain, it is also important to understand how contextual factors (e.g., systemic racism) may also impact threat neurocircuitry (
28–
31). Understanding the potential effects of such disparities on these brain structures is critical for a fuller understanding of the impacts of stress on the developing brain and creating generalizable neurobiological models of disease.
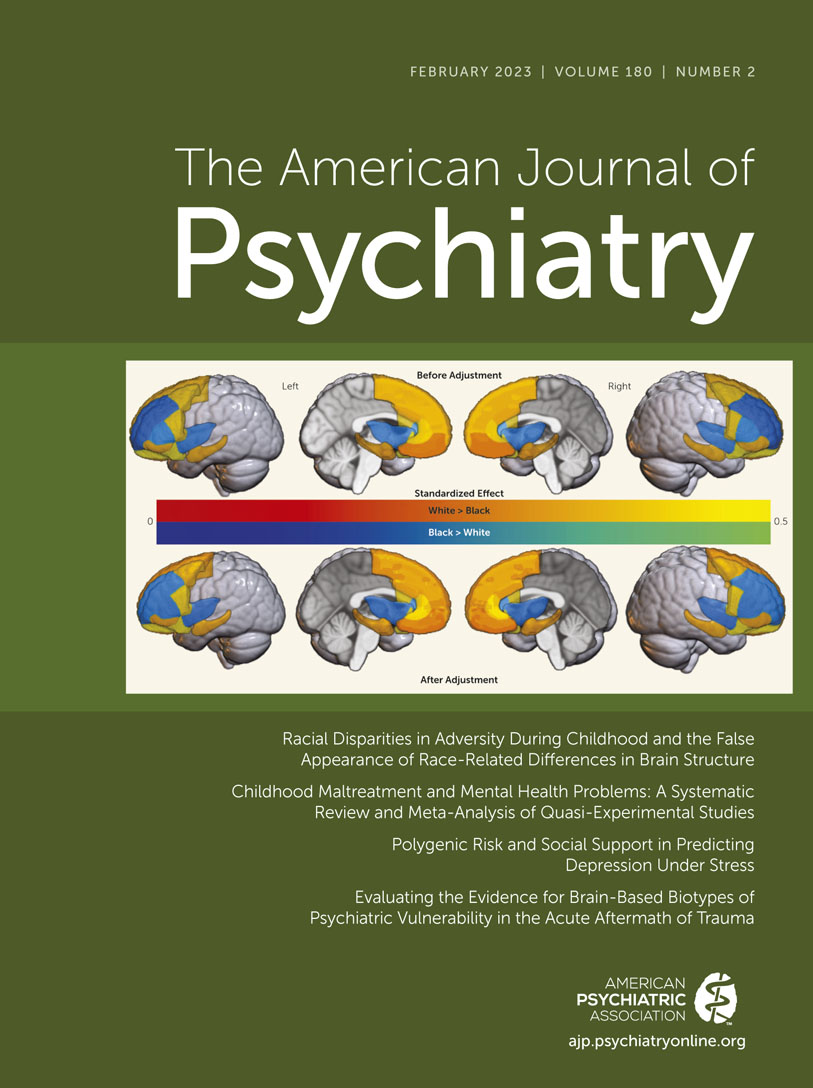
In this study, we investigated the relationship between racial disparities in adversity exposure and race-related differences in brain structure among participants in the ABCD Study. We hypothesized that Black American children would have experienced more adversity than White American children in the sample. We further hypothesized that greater exposure to adverse life experiences would be related to lower gray matter volume in the amygdala, the hippocampus, and several subregions of the PFC. Finally, we anticipated that Black and White children would show differences in gray matter volume of these regions and that these differences would be partially explained by racial differences in exposure to adversity.
Discussion
In this study, we investigated the neuroanatomical consequences of racial disparities in adversity during childhood. We found that, compared with White American children, Black American children endorsed more traumatic events, material hardship, and family conflict and lived in more disadvantaged neighborhoods, and their caregivers had lower income and educational attainment and were more likely to be unemployed. Greater exposure to these adversities was linked to lower gray matter volumes in the amygdala and several subregions of the PFC. Accordingly, Black children showed lower gray matter volumes in the amygdala, the hippocampus, and several subregions of the PFC compared with White children. Accounting for racial disparities in exposure to adversity partially mediated race-related differences in a number of regions, including the caudal anterior cingulate, lateral orbitofrontal gyrus, and superior frontal gyrus. However, although our findings held when other adversity disparities were considered, such as pollution exposure, there remain other structural inequities that may contribute to race-related differences in the brain, which must be investigated in future research. Taken together, our findings highlight the impact that disparities in early-life adversity have on race-related differences in the structure of neural circuitry associated with PTSD and other trauma- and stress-related disorders.
One way to conceptualize the present findings is that a significant portion of the gray matter volume differences reflect racial disparities in toxic stress. Toxic stress refers to prolonged exposure to adverse experiences that leads to excessive activation of stress response systems and an accumulation of stress hormones, which in turn disrupt the immune and metabolic regulatory systems and ultimately the developing architecture of the brain (
44–
46). Importantly, the effects of toxic stress may be dependent on the relative timing of stress exposure. The PFC, amygdala, and hippocampus undergo rapid development beginning in early childhood and continuing until early adulthood (
47), and this development is punctuated by sensitive periods where stress may have a larger impact (
48,
49). In fact, previous work suggests that exposure to adversity during these sensitive periods may have direct effects on the PFC, amygdala, and hippocampus as well as on subsequent threat responses and regulation (
50–
54). Moreover, our results showed that income was the most common predictor of gray matter volume disparities, aligning with previous research showing that the effects of low socioeconomic status, and specifically low income, have profound effects on neurobiological trajectories (
22,
24,
25,
55–
57). Taken together, early-life adversity may act as a toxic stressor that disproportionately impacts Black children as a result of their significantly greater exposure to adversity and contributes to differential neural development of key threat-processing regions.
The impacts of toxic stress may be immediate or temporally delayed, depending on the specific brain region. For example, one study examining the effect of childhood sexual abuse on regional brain development (
58) found an association between abuse and lower hippocampal volume at ages 3–5 but with lower frontal cortex volume at ages 14–16. In the present study, no effects of adversity were found in the hippocampus, although effects were found in the amygdala and the prefrontal cortex, potentially reflecting the impact of differential sensitive periods of brain development in these regions. A potential delayed effect may partially explain the relatively small magnitude of racial differences in gray matter volume of threat-related regions. Specifically, it may be that the disparities in adversity do not lead to major immediate differences but will be potentiated into adulthood in either brain structure or brain function (
27). Future analyses of the longitudinal ABCD data set may shed light on what potential long-term impacts these disparities may have on the brain and behavior. In sum, our findings may reflect the neuroanatomical consequences of racially disparate environments of toxic stress.
We note here that many of the observed race-related and adversity effects had relatively small effect sizes despite many findings being highly statistically significant. The ABCD Study has high statistical power for small effects, afforded by its large sample size, and these effects are likely more accurate to the general population than traditionally large effects in small sample sizes. A recent review of effect sizes in ABCD analyses (
59) demonstrated that the median in-sample effect size across multiple instruments (161 variables representing all questionnaires and tasks) was 0.03. The authors found a slightly larger median effect size (0.05) when mimicking “real-world” analyses of ABCD data. Thus, the observed effects of race-related disparities on brain structure are in line with, and larger than, other observations from analyses of ABCD data.
The present findings should be considered in light of several limitations. Our analyses were limited to parent-identified Black and White participants and did not include participants with other racial identities. Although the ABCD Study is one of the largest studies of children’s brains, there was a limited amount of data on non-White and non-Black children (note that only 15.7% of the participants in the present sample were Black and only 17.6% were not Black or White). Unequal sample sizes can impact statistical group comparisons. Further, many neuroimaging studies have demographically unrepresentative samples that can impact the generalizability of research findings. Thus, we echo the recommendations in previous reports to increase representation of non-White racial/ethnic groups to address broader questions on the impact of racial and ethnic disparities across groups (
60). Another limitation of the present study is the lack of longitudinal MRI data. Our analyses were focused on the impact of racial disparities on the earliest available assessment of brain structure. However, future analyses of the longitudinal MRI data in combination with potential changes in adversity may be useful to test nuanced questions about the role of adversity on race-related differences in brain development. An additional limitation is the potential role of other adversity types on race-related differences in brain structure. We focused on structural adversities but could not capture certain aspects (e.g., nutritional differences or direct toxin exposure), and our analyses did not focus on other factors, such as racial discrimination (
61). Nutritional and racial discrimination data were collected 1 year after the baseline visit, precluding any meaningful interpretations with the baseline MRI data. Although we assessed pollutant exposure at the neighborhood level, more direct measures of toxin exposure, such as those available from baby teeth collected in the ABCD Study, may provide more granular information in future analyses. Recent studies demonstrate that racism and racial discrimination directly affect brain structure and function and are associated with poor mental health outcomes (
28–
30,
62–
64), and thus future research should further explore these relationships in children. Finally, although we assessed adversity, it is unclear when these adversities occurred or for how long. Information on the timing and duration of the children’s adversity exposure could allow us to draw stronger conclusions about its effect on brain development.
In summary, we have shown that differential exposure to childhood adversity contributes to racial differences between Black American and White American children in gray matter volumes of brain regions key to emotion regulation. The disparities in gray matter volume observed in this study may be a consequence of long-term dysregulation of threat-related neural circuitry. The findings from this study thus have important implications for our understanding of the impact of socioeconomic and environmental inequalities on mental health in the United States and our understanding of racial differences in psychiatric disorder development, particularly PTSD, for which the literature on lifetime prevalence is mixed (
65–
70). Although more research is needed on the neurobiological consequences of racial disparities in childhood adversity, the present findings offer new insight into biological impacts of disproportionate stress exposure.