Borderline Personality Disorder and Suicidality
Abstract
Scope and Nature of the Problem
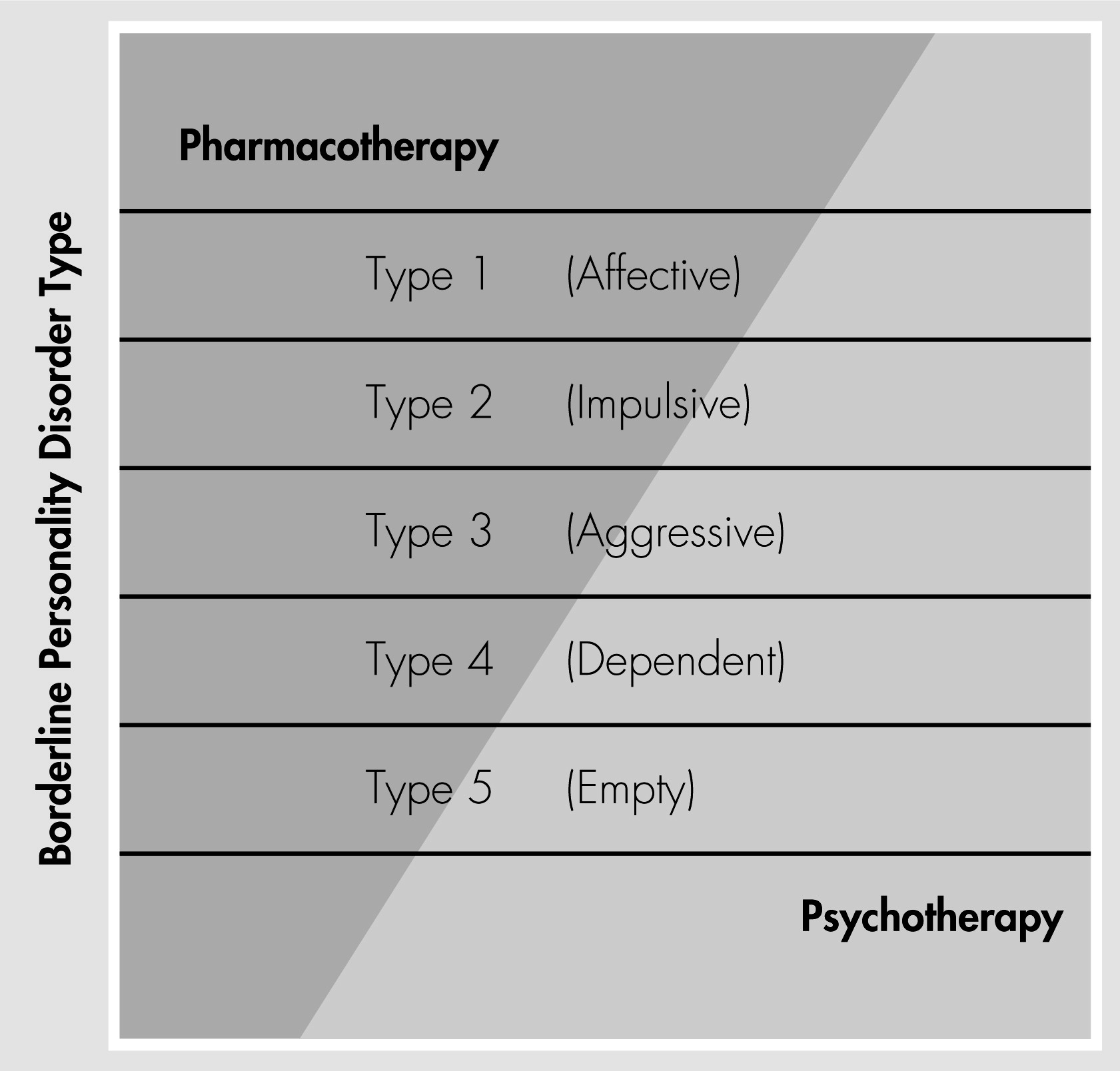
Heterogeneity of Borderline Personality Disorder
| Type | Description | Presumed DSM-IV-TR Prototypical Criteria | |
|---|---|---|---|
| 1: Affective | An atypical, moderately heritable form of mood disorder, precipitated by environmental stress. Akiskal and colleagues (4, 5) described a “subaffective” disorder, and Klein and Liebowitz (6) described “hysteroid dysphoria,” both of which resemble a form of borderline personality disorder characterized by the predominance of affect dysregulation. | Criterion 6: affective instability due to marked reactivity of mood (dysphoria or anxiety) | Criterion 5: recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior |
| 2: Impulsive | A form of impulse control disorder, reflecting an action-oriented inborn temperament. A number of reports have characterized borderline personality disorder as an impulse-spectrum disorder, because it shares a propensity to action and overlaps with other disorders of impulse control, such as substance use disorders and antisocial personality disorder (7–10). | Criterion 4: impulsivity in at least two areas that are potentially self-damaging | Criterion 5: recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior |
| 3: Aggressive | A primary constitutional temperament (11) or a secondary reaction to early trauma, abuse, or neglect (12). A predominance of aggression in borderline personality disorder could be correlated with lower levels of serotonin in the central nervous system or with other neurotransmitter or neuroendocrine irregularities (9). | Criterion 8: inappropriate, intense anger or difficulty controlling anger | Criterion 6: affective instability due to marked reactivity of mood (irritability) |
| 4: Dependent | An intolerance of being alone. Masterson and colleagues (13, 14) proposed that, in some cases, the presence of parental intolerance of the development of autonomy in the child could lay the foundation for future borderline pathology. Gunderson (15) described a similar but somewhat broader concept—intolerance of aloneness—as a common defining characteristic of many patients with borderline personality disorder. | Criterion 1: frantic efforts to avoid real or imagined abandonment | Criterion 6: affective instability due to marked reactivity of mood (anxiety) |
| 5: Empty | Lack of a stable sense of self, reflecting inconstant early parenting. Adler and colleagues (16, 17) proposed that the child’s experience of parental inconstancy and lack of empathy could interfere with the establishment of basic trust, resulting in an inability to evoke soothing memories of good, nurturing internal objects. | Criterion 7: chronic feelings of emptiness | Criterion 3: identity disturbance: markedly and persistently unstable self-image or sense of self |
Prevalence of Suicidality in Borderline Personality Disorder
Suicidality Versus Self-Injurious Behavior
“Develop, with the patient, a mutual plan that protects the patient’s life and the integrity of the treatment.”
Comorbidity
Treatment and Management
Risk Factors and Prediction of Suicide
| Risk Factor |
|---|
| Prior suicide attempts (20, 29, 37–39) |
| Comorbid mood disorder (20, 29, 34, 37) |
| High levels of hopelessness (37) |
| Family history of completed suicide or suicidal behavior (39) |
| Comorbid substance abuse (20, 34, 40, 41) |
| History of sexual abuse (42) |
| High levels of impulsivity and/or antisocial traits (29, 37, 39, 41) |
Treatment of Borderline Personality Disorder
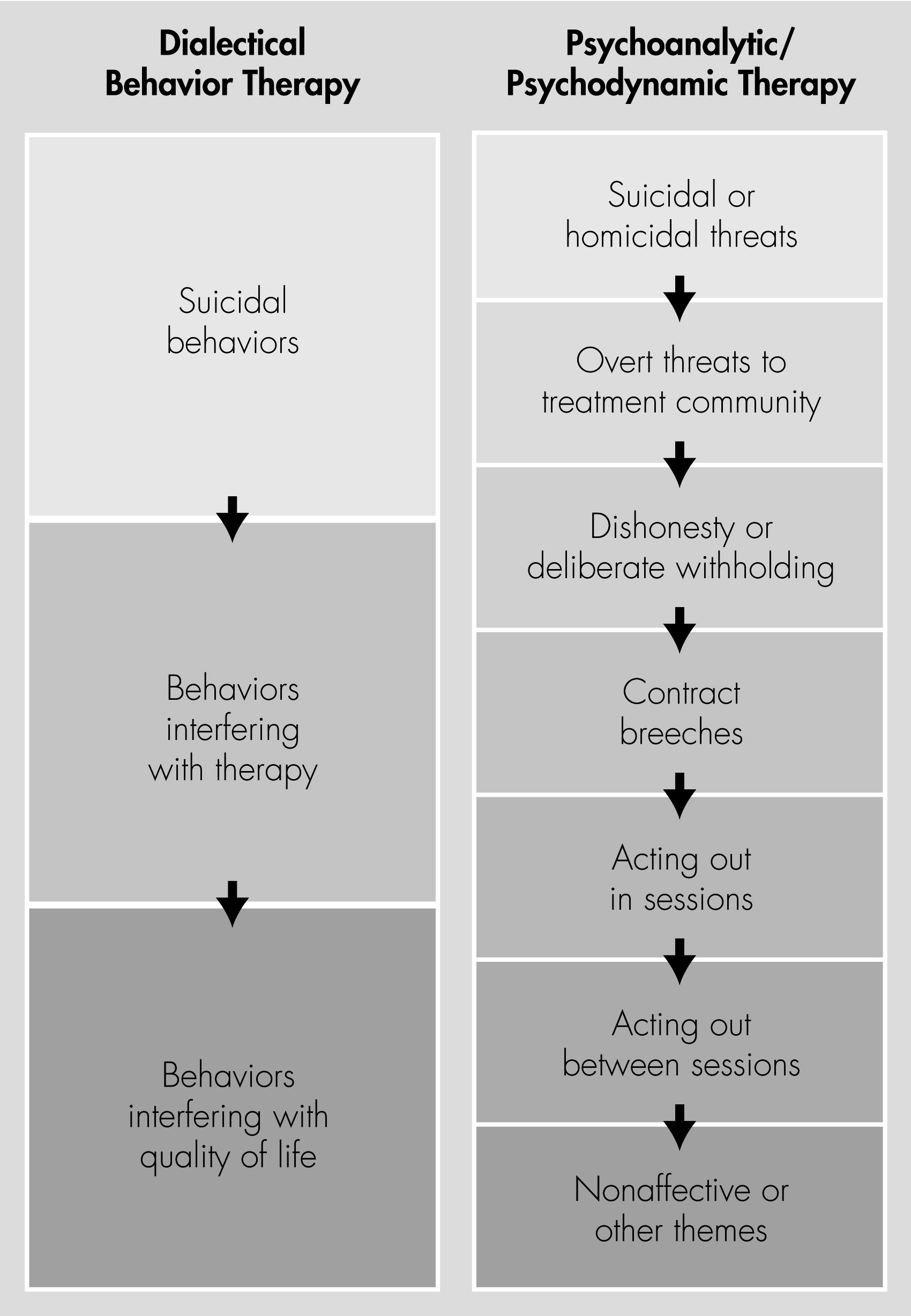
Management of Suicidal Concerns in Psychotherapy
Role of Hospitalization
Summary and Recommendations
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

