Evaluation of Cognitive Impairment in Older Adults
Abstract
Introduction
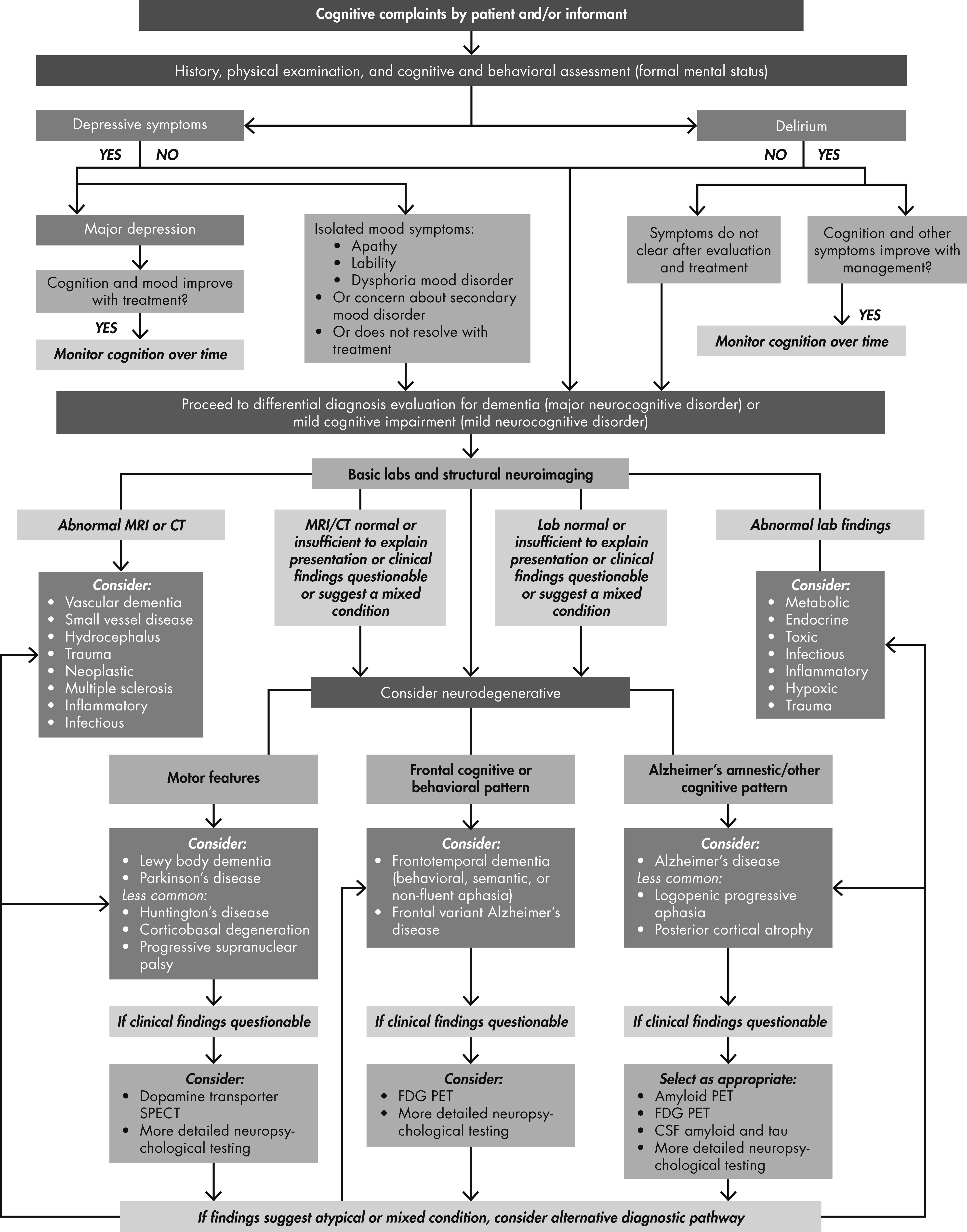
Key Features of Nondementing Disorders
Depression Characteristics
Delirium Characteristics
Mild Cognitive Impairment and Dementia Characteristics
Overview
| Disorder | Temporal Course | Presenting Symptoms | Physical Exam | Neuropathology | Laboratory | Neuroimaging |
|---|---|---|---|---|---|---|
| MOST COMMON | ||||||
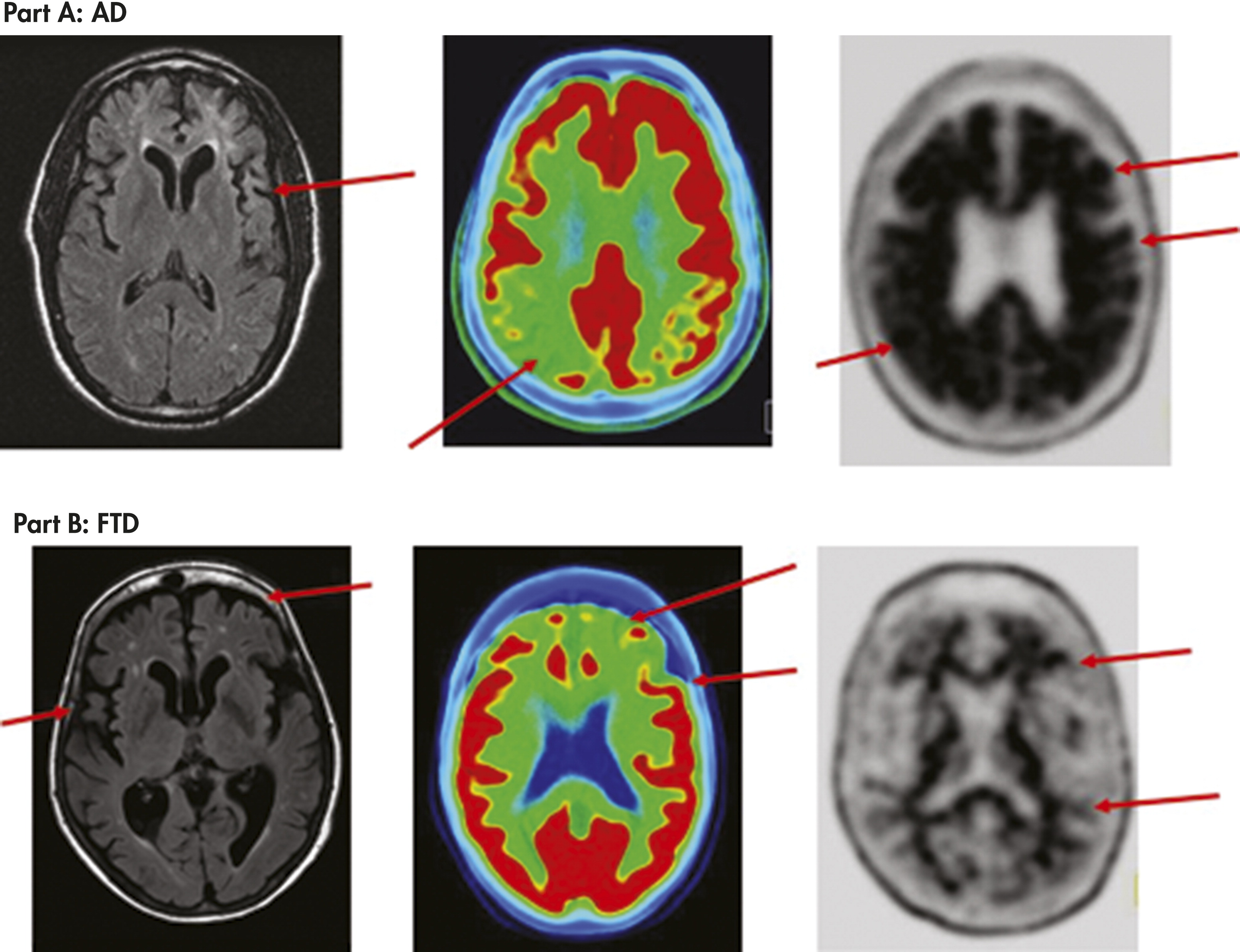
| Alzheimer’s Disease | Insidious onset, progressive course, typically in those over 70 but can start in 40s | Memory loss (amnestic) and difficulty with new learning, word-finding difficulty, anomia, visuospatial deficits, impaired insight, dysphoria, anxiety, apathy | Normal exam early; apraxia common later | Cortical atrophy, neuritic plaques (amyloid), neurofibrillary tangles (tau), amyloid angiopathy | Blood: normal or not contributory CSF: decreased amyloid- β1–42 and increased tau and phospho-tau Genetic: polygenic common; APOE-ε4 alleles confer greater risk for sporadic AD; rare autosomal dominant (familial) mutations in genes for APP, PS1 or PS2 | CT or MRI: generalized cortical atrophy, ventricles larger than expected for age MRI: hippocampal and cortical atrophy FDG PET: temporal/parietal hypometabolism Florbetapir PET: positive for brain amyloid |
| Frontotemporal Dementias | Insidious onset, progressive course, varies with subtype, typically in those 45–70 | Personality changes (disinhibition, self-care neglect, obsessive-compulsive) or language disturbance, executive impairment | Normal exam early; apraxia common later | Tau (sometimes as Pick bodies) or ubiquitin and TDP–43 proteins | Blood: normal or not contributory Genetic: familial forms with mutations on chromosome 17 (tau or progranulin gene) or chromosome 9 | CT or MRI: frontal and/or anterior temporal atrophy FDG PET: frontal and/or temporal hypometabolism Florbetapir PET: negative for brain amyloid |
| Vascular Dementia | Abrupt onset and stepwise deterioration for large vessel disease; slowly progressive for small vessel disease | Any cognitive or behavioral pattern; depressed mood common; inattention, retrieval memory complaints common | Focal neurological deficits; gait disturbances; frontal release signs | Ischemic, hemorrhagic or hypoxic lesions; subcortical lacunes, small vessel ischemia, and/or large vessel infarcts; vasculitis; amyloid angiopathy | Blood: normal or evidence of hyperlipidemia or diabetes | CT or MRI: multiple strokes, ischemia, or hemorrhage MRI: subcortical lacunes, periventricular white matter changes, large vessel strokes, or hemorrhage |
| Dementia with Lewy Bodies | Progressive course but onset can appear to be subacute at times given the fluctuations and hallucinations that mimics delirium | Prominent visuospatial deficits, hallucinations, gait disturbance and falls | Extrapyramidal motor signs such as hypokinesia, rigidity and impaired balance | Lewy bodies (alpha-synuclein) | Blood: normal or noncontributory | Dopamine transporter scan: decreased dopamine integrity in basal ganglia Florbetapir PET scan: amyloid present in a substantial subgroup |
| Parkinson’s Disease Dementia | Insidious onset, progressive course | Visuospatial, executive, and retrieval memory deficits begin after long history of Parkinson’s disease | Extrapyramidal motor signs such as hypokinesia, festinating gait, resting tremor, and cogwheeling, and impaired balance | Lewy bodies (alpha-synuclein) | Blood: normal or noncontributory | Dopamine transporter scan: decreased dopamine integrity in basal ganglia Florbetapir PET scan: amyloid present in a small subgroup |
| LESS COMMON | ||||||
| HIV Dementia / Neurocognitive Disorder | Subacute onset, static or progressive course over weeks to months | Mental slowness, impaired concentration, forgetfulness, and apathy | Slowed motor skills, ataxia, weakness, leading to paraplegia | Reactive gliosis, microglial nodules in subcortical white matter and loss of cortical neurons | Blood: Positive for HIV CSF: abnormal but nonspecific | CT or MRI: generalized atrophy, periventricular white matter abnormalities |
| Prion / Creutzfeldt-Jakob Disease | Rapid dementia with death after several months to one year | Fatigue, mood issues, insomnia, memory, executive, visuospatial and language deficits | Startle, myoclonus, tremors, incoordination, gait disturbance | Neuronal loss, vacuolization of gray matter (spongiform appearance), gliosis | CSF: elevated 14–3–3 protein, neuron-specific enloase, total tau, phospho-tau EEG: bilateral periodic discharges | MRI FLAIR: multifocal cortical>subcortical hyperintensities FDG PET: multiple diffuse regions of cortical and subcortical hypometabolism |
| Huntington’s Disease | Gradual decline | Personality changes, executive function abnormalities | Chorea and athetoid movements | Neuronal loss in striatum and at times in cortical regions | Genetic: >26 CAG trinucleotide repeats on short arm of chromosome 4 | CT or MRI: caudate atrophy, boxcar ventricles |
Dementia due to Alzheimer’s Disease
Vascular Dementia
Dementia With Lewy Bodies
Parkinson’s Disease Dementia
Frontotemporal Dementia
Office Evaluation of Depression, Delirium and Dementing Disorders
Office-Based Cognitive Assessment
| Features | MMSE | MoCA | AD8 | SLUMS | SAGE |
|---|---|---|---|---|---|
| Scoring range | 0–30 (higher score better) | 0–30 (higher score better) | 0–8 (score >2 indicates impairment) | 0–30 (higher score better) | 0–22 (higher score better) |
| Domains tested | Orientation, attention, comprehension, calculations, memory, language, constructions | Orientation, memory, clock, constructions, fluency, language, abstraction, calculations, executive, attention | Informant rating of patient’s judgment, interests, memory, ADLs, orientation | Orientation, memory, animal fluency, attention, clock drawing | Orientation, language, calculations, memory, abstraction, executive, constructional ability |
| Administration | Clinician with patient | Clinician with patient | Clinician with informant and patient | Clinician with patient | Patient (self-administered) |
| Advantages | Well-known scale; used also in delirium but cannot distinguish delirium and dementia; often used as proxy to stage dementia severity | Less ceiling effect than MMSE due to greater difficulty and more executive function tests; more sensitive to mild impairments than MMSE; used in delirium also | More aimed at dementia than mild stages; not for use in delirium | Less ceiling effect than MMSE due to greater difficulty; emphasizes memory tasks; different cutoffs for Mild NCD and dementia | Done without clinician; good correlation to clinician-administered tests; less ceiling effect than MMSE due to greater difficulty and more executive function tests; able to distinguish between MCI and dementia |
| Pitfalls | Ceiling effect especially in more educated patients; executive testing limited, does not distinguish between MCI and dementia | Cannot distinguish between MCI and dementia | Does not measure cognition directly | Less evaluation of language, constructions, and executive abilities than MoCA or SAGE | Memory testing limited |
| Time to administer | 7–10 minutes | 10–13 minutes | 3 minutes | 10 minutes | 10–15 minutes |
| Cost | $1.23 to PAR | free | free | free | free |
| Specificity/ sensitivity to detect dementia | 84%/78% with cutoff 26 or less (122) | 87%/100% with cutoff of 25 or less (92) | 80%/84% with cutoff 2 or more (123) | Comparable to MMSE but better at detecting mild NCD (93) | 95%/79% with a cutoff of 16 or less to detect cognitive impairment and 95%/95% with a cutoff of 16 or less to detect dementia (94) |
| Obtaining test | Psychological Assessment Resources (PAR) | Mocatest.org | http://alzheimer.wustl.edu/about_us/pdfs/ad8form2005.pdf | medschool.slu.edu/aging successfully/pdfsurveys/slumsexam_05.pdf | sagetest.osu.edu |
Laboratory and Neuroimaging Testing
| Test | Major Depression | Delirium | Mild and Major Neurocognitive Disorders due to Neurodegeneration |
|---|---|---|---|
| Urinalysis | X | X | X |
| Blood | |||
| Hematology | X | X | X |
| Electrolytes, calcium, magnesium, phosphorus | X | X | |
| BUN and creatinine | X | X | |
| Fasting blood sugar | X | X | |
| Liver function testing | X | X | |
| Lipid profile | X | ||
| B12 and folate | X | X | X |
| TSH | X | X | X |
| Sedimentation rate | X | X | |
| Syphilis testing | X | X | |
| APOE | Typically for AD research | ||
| CSF | |||
| WBCs | As needed | ||
| VDRL | As needed | ||
| Amyloid-betab | If questioning AD | ||
| Tau and p-taub | If questioning AD | ||
| MRI | |||
| Structural | X | X | |
| Hippocampal volume | If questioning AD | ||
| Periventricular white matter changes | X | ||
| Florbetapir PET | If questioning AD | ||
| FDG PET | For differentiating AD and FTD | ||
| Dopamine transporter SPECT | If questioning DLB or Parkinson’s | ||
| Electroencephalogram | If clinical picture is unclear |
Other Neuropsychiatric Office Tests
Conclusions
Footnote
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

