Recent neuroimaging and neuropsychiatry research in bipolar disorders have demonstrated significant white-matter abnormalities.
1 Prefrontal white-matter abnormalities have been found in first-episode bipolar disorder.
2 Compared with healthy controls, people with bipolar disorders revealed significant abnormalities in corpus callosum,
3 deep white matter,
4 anterior-limbic neural substrate,
5 and bilateral corona radiata and right anterior thalamic radiation.
2 Disorganization in white-matter tract and myelin sheath alteration has been described in bipolar disorder. In contrast with bipolar disorder, schizophrenia patients presented with alterations in both radial and axial diffusivity, suggesting increased water content outside the axonal space. This suggests different pathophysiological mechanisms in bipolar disorder and schizophrenia.
6This case report aims to highlight a condition in which central demyelination has been associated with bipolar disorder. Also, this case brings out the complexity in diagnosis and cognitive dichotomy in managing a patient with label of psychiatric disorder. Written consent has been obtained from the patient’s parents.
Case Report
A 28-year-old Chinese man presented with a background history of normal development and no past history of medical or psychiatric illness. His marriage failed in 2003, and he developed depressive illness in 2006. He was treated with fluoxetine, 20 mg daily, with good recovery. Diagnosis of mania with psychosis was made in 2007, when he presented with insomnia, overfamiliarity, increased goal-directed activity, elated mood, agitation, and irritability, and auditory hallucinations for several weeks. He responded well to a combination of olanzapine 2.5 mg nocte and sodium valproate (modified release) 500 mg daily. Based on the presentation of mania with psychosis and previous history of depression, diagnosis of Bipolar I Disorder was made. He achieved remission without much difficulty and later was maintained on sodium valproate (modified release) 500 mg daily.
In June 2008, he presented to the hospital with fever, chills, vomiting, headache, and unstable gait for a week. On examination, he had central and peripheral cyanosis, weak radial pulse, hypotension, and hyponatremia. After admission, his Glasgow Coma Scale (GCS) score deteriorated rapidly, and he had to be transferred to the Intensive Care Unit (ICU). He was presumed to have neuroleptic malignant syndrome (NMS) due to olanzapine, despite lack of muscle rigidity, diaphoresis, tremor, or incontinence, and his highest creatine kinase was 167 U/L. He was also suspected to have sodium valproate-induced Syndrome of Inappropriate Antidiuretic Hormone (SIADH) because of hyponatremia, even though no urine osmolality test was done; he had hypotension and required fluid resuscitation. The psychiatric unit reviewed him again in November 2008 and concluded that he was in remission from Bipolar I Disorder.
He presented to the hospital again in February 2009 with a 1-week history of fever, reduced oral intake, vomiting, dehydration, drowsiness, and hyponatremia. His serum sodium level was 110 mmol/L on admission, with urine ketone of 2+. His hyponatremia was thought to be due to severe lack of oral intake. He was later discharged and transferred to our hospital for further management of his psychiatric condition. The provisional diagnosis then was Bipolar I Disorder in Depressive Phase.
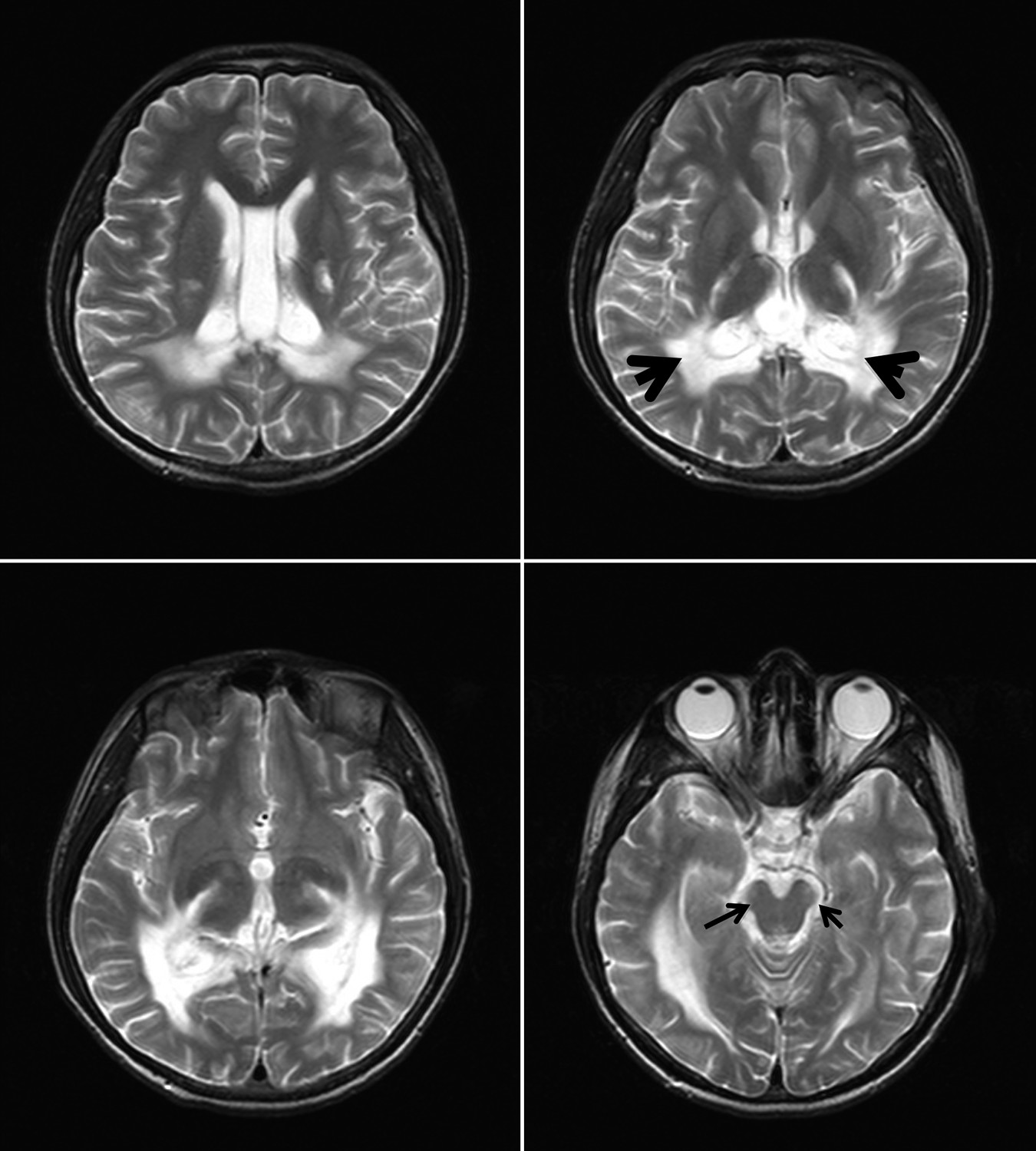
In our hospital, it was highly possible that he had an adrenal crisis, based on the persistent hyponatremia, despite aggressive fluid resuscitation, with unexplained shock, clinical history of nausea and vomiting, and metabolic acidosis. Addison’s Disease was quickly confirmed the next day with the Synecthen test. Serum cortisol in the morning was 103 nmol/l (normal: 119–618 nmol/l), and ACTH test showed no increase in cortisol level after 60 and 90 minutes. Magnetic resonance imaging (MRI) of the brain was taken during the admission, which showed persistent symmetrical, confluent bilateral signal-intensity changes in the parieto-occipital deep white matter, splenium of corpus callosum, and the corticospinal tract region. The three zonal regions were more appreciable in the latest MRI, as compared with the MRI performed 6 months earlier, with the lesion showing a more distinct margin and degree of rim enhancement. There were involvements of posterior limb of both internal capsules, with a more distinct abnormal hyperintense signal at the retrolenticular part and optic radiation. There was better appreciation of the signal changes in the brainstem, especially at both lateral lemniscus and brachum of inferior colliculus region, and pyramidal tract in pons and medulla oblongata. There was preservation of U-fiber. MRI features demonstrated a pattern consistent with the cerebral form of X-linked ALD with evidence of progression (
Figure 1). His phytanic acids level was 0 mg/100 mL (normal: <0.376), but his ratio of very-long-chain-fatty-acid (VLCFA) was abnormal. His C24:0/C22:0 ratio was 1.36824 (normal: <1.329), and C26:0/C22:0 was 0.0924956 (normal: <0.085). Mutational analysis revealed an
ABCD1 mutation. In conclusion, his diagnosis was adult-onset X-linked adrenoleukodystrophy (ALD), presented initially with Bipolar I disorder. A year later, he came for outpatient review and showed severe impairment in attention, visuoconstructional memory, executive, and language domains. He gradually deteriorated in terms of his cognitive state and later lost his vision and speech ability. A few months before he passed away, he lost the ability to walk. Neurological examination at the time showed hypertonia of limbs, increased deep tendon reflexes, and clonus. He passed away 2 years after the diagnosis was made.
Discussion
The complexity of this case lies in the fact that the patient had an Axis I diagnosis of Bipolar I Disorder and Axis III diagnosis of ALD, and his Axis I diagnosis preceded the Axis III condition. Many conditions with central demyelination have been linked with bipolar disorder, such as adult-onset metachromatic leukodystrophy
7 and adult-onset ALD.
8 Another learning point from this case is that it is not commonly appreciated that patients with ALD can first present in adulthood with psychiatric illness, such as bipolar disorder. Out of 13 published case reports with detail psychiatric history, 12 had symptoms of mania, and 9 of the 13 patients had a diagnosis of bipolar disorder.
7 This case also illustrates the importance of maintaining an open mind and performing neurological and radiological examinations on patients with atypical presentation, and who are not responding to standard treatment.
9Adult-onset ALD is a very rare condition. ALD is an X-linked peroxisomal disorder caused by a deficiency in the degradation of VLCFA due to mutation of the
ABDC1 gene on the X chromosome,
10 which leads to central and peripheral demyelination, with concomitant adrenal insufficiency.
7 Afflicted individuals may present with any combination of adrenal, gonadal, neurological, or psychiatric disorders. Most of them will have neurological involvement at some point during the course of their illness. Although the most common presenting features include abnormalities of gait and evidence of upper motor neuron involvement, mania and psychosis can be the presenting features.
11 In the case of psychiatric presentation, it is often difficult to accurately identify the onset of personality or mood changes; if noticed, they are often associated with other causes.