To the Editor: We report a case of a vascular malformation involving the right posterior subiculum and contiguous hippocampus, which was discovered incidentally at autopsy in a 52-year-old woman with lifelong history of mental illness and mild intellectual disability who died as a result of cardiorespiratory arrest and acute global anoxic/ischemic encephalopathy. As per family, patient was born by forceps delivery, and her cognitive deficit was attributed to an intrapartum brain injury. Psychiatric disturbances included dependent personality disorder, depression, and obsessive-compulsive disorder. Before her death, the patient was on valproic acid/divalproex 250 mg bid, quetiapine 200 mg–300 mg once daily, and fluoxetine 20 mg. Her medical history was also significant for colitis (not further defined), hypercholesterolemia, and obesity. There was no history of seizures, attention-deficit hyperactivity disorder, cerebral palsy, or Prader-Willi syndrome.
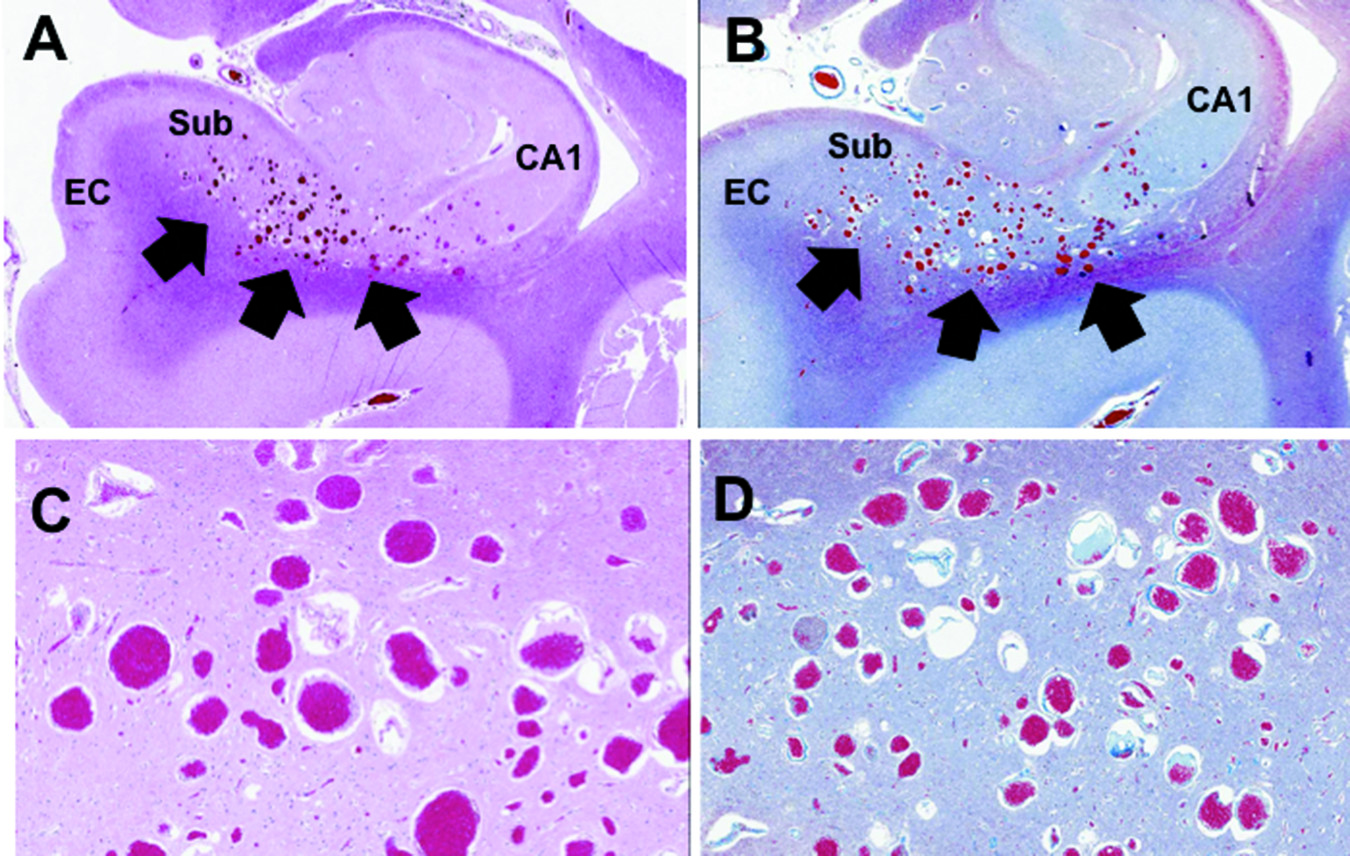
Neuropathological evaluation at autopsy revealed an unsuspected vascular malformation involving the right posterior subiculum and adjoining portion of the CA1 subfield of the hippocampus (
Figure 1 and
Figure 2 [A−D]), consistent with a capillary telangiectasia (
Figure 2 [A−D]), as opposed to a cavernous malformation, a developmental venous anomaly, or an arteriovenous malformation. There was absence of old peri-lesional hemorrhage, calcifications, or “steal effect.” Aside from extensive acute global anoxic/ischemic changes, mild subpial cortical gliosis, and mild cerebrovascular arteriosclerosis, the rest of the brain showed no malformation(s), neuronal migration disorder, destructive, demyelinating, or metabolic lesions. Importantly, there was no evidence of perinatal/intrapartum asphyxial brain damage, in the form of mesiotemporal/hippocampal sclerosis, ulegyria/cortical scarring, multicystic encephalopathy, or thalamic necrosis. Neurodegenerative changes were absent, and immunostains for hyperphosphorylated tau protein, β-amyloid peptide, and α-synuclein were negative.
Several decades ago, Malamud drew attention to psychiatric disorders associated with focal lesions of the limbic system in a series of 18 autopsied cases of tumors and history of seizures,
1 of which 9 focal lesions were in the temporal lobe (one vascular malformation). Since then, the association between medial temporal lobe and psychosis has been reported, mainly in the context of epilepsy,
2 schizophrenia,
3 and refractory obsessive-compulsive disorder.
4 The ventral subiculum has circuit connections with limbic areas involved in stress, affect, and reward.
5Capillary telangiectasias are rarely associated with neurological symptoms and, to our knowledge, this is the first such case reported in the subicular region of a patient with cognitive deficit and mental illness without history of seizure disorder. The present lesion is clinically, anatomically, and histopathologically distinct from the famous case of “Dr. Z,” originally described by Hughlings Jackson in the context of psychomotor epilepsy–also subsequently reported in a similar case—as these were instances of cavernous malformation confined to the lateral aspect of the entorhinal cortex, sparing the subiculum and hippocampus.
6Although the association of this unusual vascular malformation with the decedent’s lifelong intellectual disability and psychiatric manifestations remains speculative, it is nonetheless plausible, given the critical role of the posterior hippocampus and subiculum in cognitive and affective dysfunction. The case raises important questions about the role of these structures in intellectual disability, anxiety, and mood disorders.