To the Editor: Intravenously administered tissue plasminogen activator (IV-tPA) remains the only approved drug therapy for achieving arterial recanalization in acute ischemic stroke. Timely administration of IV-tPA often results in rapid recanalization and rapid clinical recovery. However, rapid recanalization of an occluded intracranial artery rarely can lead to cerebral hyperperfusion syndrome, with variable presentations. We present a case that showed an excellent early recovery after IV-tPA for severe acute ischemic stroke. However, the patient developed severe suicidal ideation on Day 3. We present clinical and various imaging studies to elucidate the underlying pathophysiological mechanisms.
A 73-year-old man presented with sudden left-sided weakness for 140 minutes. Clinical evaluation revealed blood pressure 157/75mmHg and severe left hemiplegia (Power Medical Research Council Grade 0/5). The National Institutes of Health Stroke Scale (NIHSS) score was 19 points.
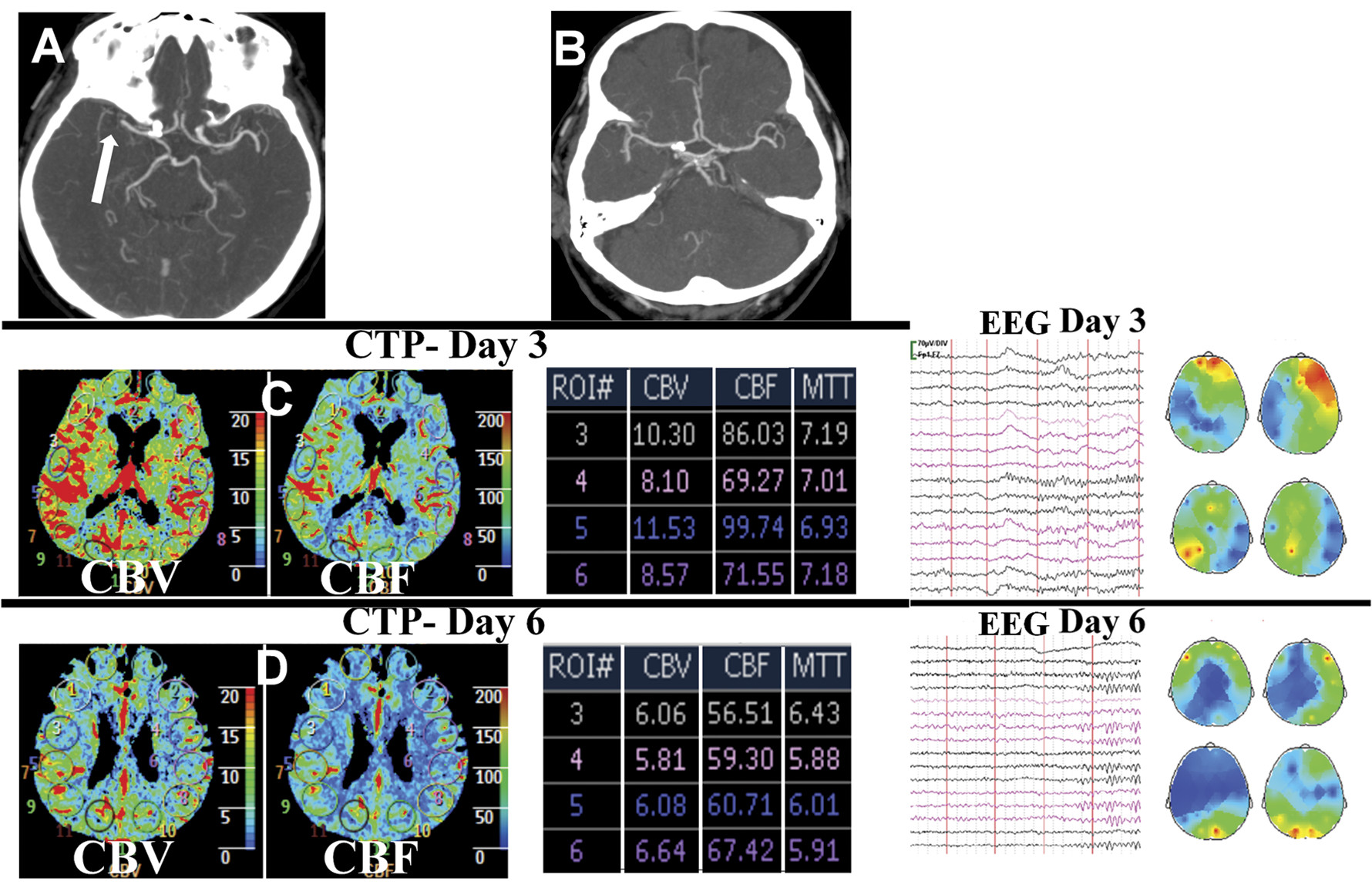
No abnormalities were noted on the emergently performed brain computerized tomography (CT). However, CT angiography (CTA) revealed right middle cerebral artery (MCA) occlusion (
Figure 1 [A]). Intravenous thrombolysis and continuous transcranial Doppler (TCD) monitoring, commenced at 180 minutes from symptom-onset, resulted in complete recanalization of right MCA at 14 minutes after treatment onset. This was accompanied by rapid and persistent clinical recovery (NIHSS score 1 point at 1 hour). Neurological examination, brain CT, and CTA (
Figure 1 [B]) performed on Day 2 were unremarkable.
Despite brilliant clinical recovery, our patient displayed severe suicidal ideation on Day 3. He had never suffered from depression or any psychiatric illness in past. Brain magnetic resonance imaging showed an acute lacunar infarction in the putamen. Repeat TCD showed considerably elevated flow velocities in right MCA (3 times more than the left). Further evaluation of cerebral hemodynamics by CT-perfusion (CTP) revealed relative right MCA territory hyperperfusion (
Figure 1). Suspecting that regional hyperperfusion was responsible for his suicidal ideation, we refrained from initiating any medications. Head-up position, fluid restriction, and aggressive blood pressure control (to 120/80 mmHg) resulted in rapid improvement in psychiatric features during the next 2 days. CTP performed on Day 6 revealed normalization of cerebral perfusion parameters (
Figure 1). Since his hospital discharge, on Day 7, he has remained well during the past 1 year.
“Reperfusion injury” after reversible ischemia may result in myocardial stunning in some cases.
1 Similar “ischemic stunning” of the brain has been proposed in acute ischemic stroke when clinical recovery does not accompany successful systemic thrombolysis.
2 Acute suicidal ideation, despite brilliant early recovery in our patient was unexpected. We hypothesized that the regional hyperperfusion led to the reduced neuronal activity (neurovascular uncoupling), manifesting as severe psychiatric disturbance. Our hypothesis was supported by the significant right fronto-temporal slowing on electroencephalography (EEG), performed on Day 3 (
Figure 1). Rapid clinico-psychiatric recovery accompanied normalization of cerebral perfusion (Day 6 CTP in
Figure 1) and neuronal activity (Day 6 EEG in
Figure 1).