LE was initially identified as a paraneoplastic neurologic syndrome usually associating with intracellular onconeural antibodies, such as Hu antibodies, CV2/CRMP5 antibodies, Ma2 antibodies, and amphiphysin antibodies.
3 Lately, some types of antibodies against cell membrane antigen, such as voltage-gated potassium channels antibodies (VGKC-abs), N-methyl-D-aspartate receptor (NMDAR) antibodies, and other antibodies, were found in patients who usually do not have cancer.
4 Previous studies mainly focused on the features and treatments of LE. Little was known about what kind of antiepileptic drugs (AEDs) was effective in treating this kind of seizure disorders. Here, we describe two cases of adult onset TLE with VGKC-abs-associated LE in China. This is the first reported Chinese case; we propose that levetiracetam (LEV) may be a useful treatment for this kind of TLE.
Case Reports
Case 1
A 57-year-old right-handed woman was admitted to our hospital with a 9-day history of short-term memory loss and psychiatric symptoms without fever. She suffered from recurrent episodes of fear without hallucination when few people around. Moreover, she had two episodes of generalized tonic-clonic seizure (GTCS) 9 days before admission. After admission, the patient appeared to have complex partial seizure (CPS), seven to eight times per day.
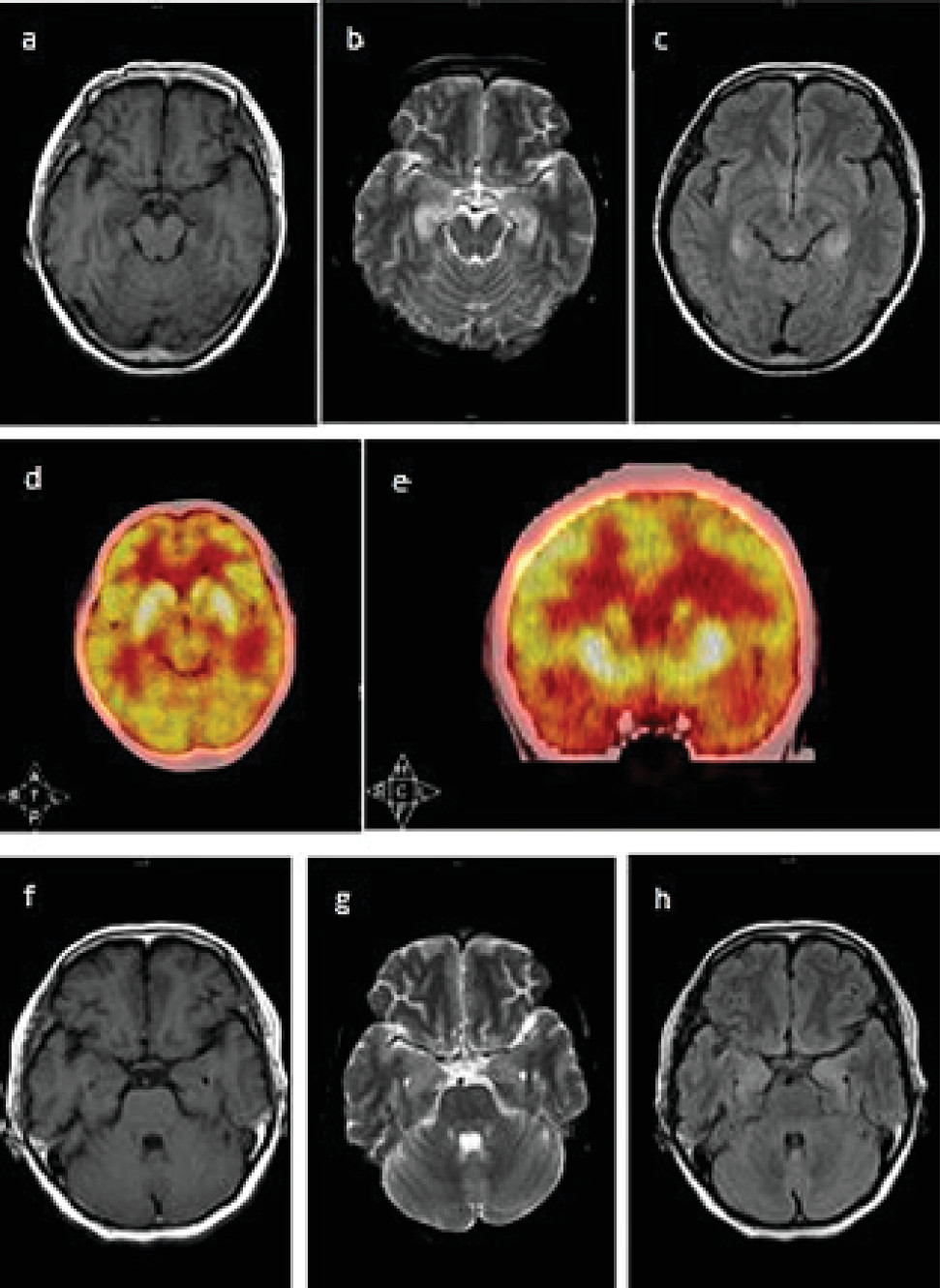
Physical examination showed short-term memory impairment and time disorientation. Laboratory tests demonstrated a persistent hyponatremia (117−131mmol/L) and hypochloremia (85.2–94.7mmol/L). Other routine blood tests were normal, such as chest X-ray, CSF examination, and bone marrow puncture. Electroencephalograph (EEG) showed generalized slow activity without epileptic discharges. The Mini-Mental State Examination (MMSE) score was 9/30 (illiterate). Brain MRI demonstrated bilateral increased signal in the medial part of the temporal lobe on T2-weighted and fluid-attenuation inversion recovery (FLAIR) images (
Figure 1 a‒c). Positron emission tomography/computed tomography (PET/CT) showed hypermetabolism in bilateral hippocampus (
Figure 1 d and e).
Suspecting virus encephalitis at first, IV acyclovir (10 mg/kg for 14 days) was started, and seizures were treated with LEV (500 mg bid). Four days later, the frequency of seizure declined obviously to three to four times per day. Two weeks later, the seizure was totally under control, but the psychiatric symptoms did not improve. Fifteen days after admission, we started to give this patient IV methylprednisolone (500 mg/day for 5 days), and her symptom improved dramatically. Then, the patient continued to use AEDs (LEV 500 mg bid) after discharge.
Two months later, the patient returned to our hospital for a follow-up visit. Her serum sodium level had returned to normal (139 mmol/L), and she did not have any psychiatric symptoms or episodes of seizure. MMSE score rose to 13/30 (illiterate). Furthermore, the signal of the medial temporal lobe on T2-weighted and FLAIR images had also reduced within two months (
Figure 1 f‒h). Antineuronal antibodies (Hu, Yo, Ri, Ma1/2, CV2/CRMP-5, and amphiphysin) were negative. Serum VGKC-abs level and CSF VGKC-abs level before the prescription of methylprednisolone were 130.54 pmol /L and 161.14 pmol /L, respectively (cutoff value: 100 pmol/L). Antibody titers were measured with ELISA (1:5 dilution, Kingmed Diagnostics, Chengdu, China). We did not test the antibodies 2 months later because the patient refused.
Case 2
A previously healthy 45-year-old woman presented with three episodes of generalized seizure evolving to status epilepticus 3 months prior to admission, each seizure lasting more than 10 minutes. She gradually developed disorientation, and psychiatric symptoms manifested as personality change, unwillingness to communicate with others, anxiety, panic, visual and auditory hallucination, persecutory delusion, and aggressive behavior.
This patient had elevated TPOAb (179.20 IU/L) and TgAb (157.40 IU/L), but other hormones, such as ACTH, LH, GH, FSH, PTC were normal. She also had hyponatremia (130–133 mmol/L) and hypochloremia (95–96 mmol/L). Other laboratory and radiological examinations did not reveal any signs of infection or tumor. Her serum VGKC-abs level and CSF VGKC-abs level before the prescription of methylprednisolone were 112.35 pmol/L and 194.63 pmol/L, respectively. After that, we give the patient IV methylprednisolone (500 mg/day) and oral LEV (500 mg bid) simultaneously. However, 5 days later, the patient was automatically discharged even though her symptoms did not fully resolve. At discharge, IV methylprednisolone was stopped, and LEV was continued to be used in the same dose. When the patient returned to our hospital for a follow-up visit 2 months later, she did not have any episode of seizure and her psychiatric symptoms also improved.
Discussion
Combining the patients’ history, laboratory tests, imaging examinations, and response to treatment, we considered these two patients to be nonparaneoplastic VGKC-abs- associated LE. This is in accordance with newly proposed diagnostic criteria for LE.
5,6VGKC-abs-associated LE constitutes approximately 30% of all autoimmune encephalitis with antibodies to cell membrane antigens.
7 VGKCs are widely expressed throughout the entire nervous system and are critical in establishing the resting membrane potential and generation of neuronal action potentials, some subtypes, such as VGKC1.1, VGKC1.2, VGKC1.6, were strongly expressed in the hippocampus molecular layer.
8 Recent studies suggest that these antibodies seem to target associated VGKC-complex proteins instead of Kv1 subunits. These targeted proteins include leucine-rich, glioma inactivated 1 (Lgi1), and contactin-associated protein-2 (Caspr2). In patients with positive Lgi1-Abs, the probability of occurrence of seizure is more common than the patients with positive Caspr2-Abs.
9 Because the VGKC-abs were detected using ELISA, we did not further detect the Lgi1-Abs/ Caspr2-Abs.
These two cases prompted that VGKC-abs-associated LE may be an important cause for adult onset TLE. The clinical features of epilepsy in previously reported VGKC-abs-associated LE were summarized in
Table 1. Case series and case reports from January 2001 to December 2013, which refer to adult onset (>18 years old) VGKC-abs-associated LE, were included in
Table 1. Reviews, letters, case series, and case reports concerning other antibodies and children cases were excluded, as well as articles, which only discussed one part of LE (e.g., only MRI findings) or the clinical data are incomplete or unclear. VGKC-abs-associated LE is more common in men above 40 years old. Vincent et al. reviewed 10 patients with positive VGKC-abs associated LE, and seizures were present in nine patients during the acute phase of the disease, including GTCS and/or CPS. Additional features include hallucination, agitation, and behavioral disturbance. Hyponatremia is a common symptom.
10 Antibodies to VGKC may also associate with paraneoplastic LE because of thymoma or small cell lung cancer, but more frequently with nonparaneoplastic LE.
10The most common abnormalities on brain MRI is increased signal in medial temporal lobe on T2-weighted and FLAIR images, either bilateral or unilateral, but it can also be normal.
11, 12 In a systematic review, neuroimaging investigations revealed baseline MRI changes in 70% cases.
13 A general tendency of mediotemporal signal regression is within 4–17 months (
Table 1), but some patients develop into hippocampal atrophy and hippocampal sclerosis.
4,12The relevance of clinical manifestation and antibodies titers has been confirmed in many researches.
14–16 With the antibodies titers declined, the clinical symptom can improve as well as the lesion on brain MRI. The antibodies titers of these two cases were relatively low, may be for the reason that the symptoms of these two cases were relatively mild and the samples were obtained at the early onset of the disease. Furthermore, the levels of VGKC antibodies in the CSF were higher in the CSF compared with serum in both cases, indicating intrathecal synthesis of antibodies, as previous reported in anti-NMDA-receptor encephalitis.
17Recently, there have been frequent descriptions of LE and refractory epilepsy (RE) secondary to antibodies to a broad variety of neuronal antigens.
18,19 VGKC-complex antibodies and similar antibodies have been identified in around 10% of unselected patients with unexplained and drug-resistant epilepsy.
20 For patient with RE or super RE, it is crucial to establish the underlying cause of seizures.
21 Both paraneoplastic and nonparaneoplastic LE may result in RE. Recent researches suggested autoimmune encephalitis may be an essential cause of nonconvulsive status epilepticus, especially anti-NMDAR encephalitis.
19 Compared with widely expressed NMDA receptors,
17 antibody associated with LE that strongly affects temporal lobe is the VGKC complex antibody.
22 Although the incidence of RE associated with anti-VGKC encephalitis remains to be determined, the typical medial temporal regions that anti-VGKC encephalitis affects may be a potential reason for RE.
23The main therapy for LE is immunotherapy. Corticosteroids, intravenous immune globulin (IVIg) and plasma exchange are most frequently used. Other immunosuppressive agents, such as cyclophosphamide and rituximab, can also be utilized.
7,11 Although immunotherapy is widely accepted for the treatment of LE, there are many side-effects and other risks.
20 Additionally, some patients respond poorly to immunotherapy and fully control of epilepsy needs a long time after immunotherapy and sometimes needs to be treated with AEDs simultaneously.
17,18Previous studies rarely focused on the treatment of seizure. Seizure in this disorder is generally difficult to control and often require treatment with multiple AEDs.
24 Only few studies mentioned the AEDs they prescribed. Phenytoin (PHT), phenobarbital (PB), valproic acid (VPA), clobazam (CLB), lorazepam (LRZ), lamotrigine (LTG), carbamazepine (CBZ), topiramate (TPM) and LEV were prescribed in previous reports of patients with positive VGKC-abs (
Table 1). But the relationship between the control of seizures and the prescription of AEDs didn’t point out explicitly. Thus, it is unclear which kind of AEDs is more effective for epilepsy induced by VGKC-abs associated LE. In our two cases, after using LEV, the seizure was under control, even before the administration of immunotherapy (Case # 1). In previous case reports, there are a few cases which responded well to AEDs alone.
20,25 Barajas et al. also reported a case who was treated with LEV and LTG and the patient reached seizure free within 24 months.
8 Until now, LEV has been proved to be safe and effective in treating acute seizure and status epilepticus.
26 Swisher et al. suggested that the combination use of PHT, LEV, and pregabalin (PGB) in brain tumor patients with refractory status epilepticus is safe and highly effective.
27 As demonstrated by these cases, we proposed that LEV may be a useful AEDs for seizure induced by LE. And this application did not have an obvious psychiatric adverse side effect.