To the Editor: Cryptococcosis is the most common mycotic infection of the CNS and primarily manifests as meningitis. Cryptococcal infection of the nervous system was first described early in the beginning of the last century. Thus far, few cryptococcal infection cases have been reported to be associated with HIV-positive patients. Here, the authors report a rare case of a 75-year-old male patient with no previous history of any systemic diseases such as diabetes, hypertension, or another immunocompromised condition, but with a cryptococcoma in his brain.
Cyptococcosis, the most common mycotic infection of the CNS, primarily manifests as meningitis. This ubiquitous organism typically enters the human body via the respiratory tract and then spreads hematogenously from the lung to the CNS.
1 According to the analysis of the French Cryptococcosis study group, of the 1057 cryptococcosis cases, 86% involved patients with AIDS. Malignancies (32%), organ transplantation (19%), and corticosteroid therapy (33%) were the main predisposing conditions in 163 patients without AIDS.
2Intracranial cryptococcosis primarily manifests as meningitis, headache, fever, and nuchal stiffness. In some cases, mass lesions can also develop.
3 Here the authors report a case of cerebral cryptococcoma found in a 75-year-old male patient who had no diabetes, hypertension, or AIDS, nor received immunosuppressive medications, and he did not present any manifestations of meningioencephalitis.
Case Report
A 75-year-old man was admitted to our hospital because he had right side weakness. The symptom had been progressive for several days prior to his admission. The patient had no severe headache or fever. He exercised regularly and did not drink, smoke, or take drugs. Physical examination showed weakness in his right arm, as well as in his right leg to lesser degree, and mildly diminished touch sense in the right limbs compared with the left ones. Physical examination showed no choking, hemianopia, ataxia, or dysarthria.
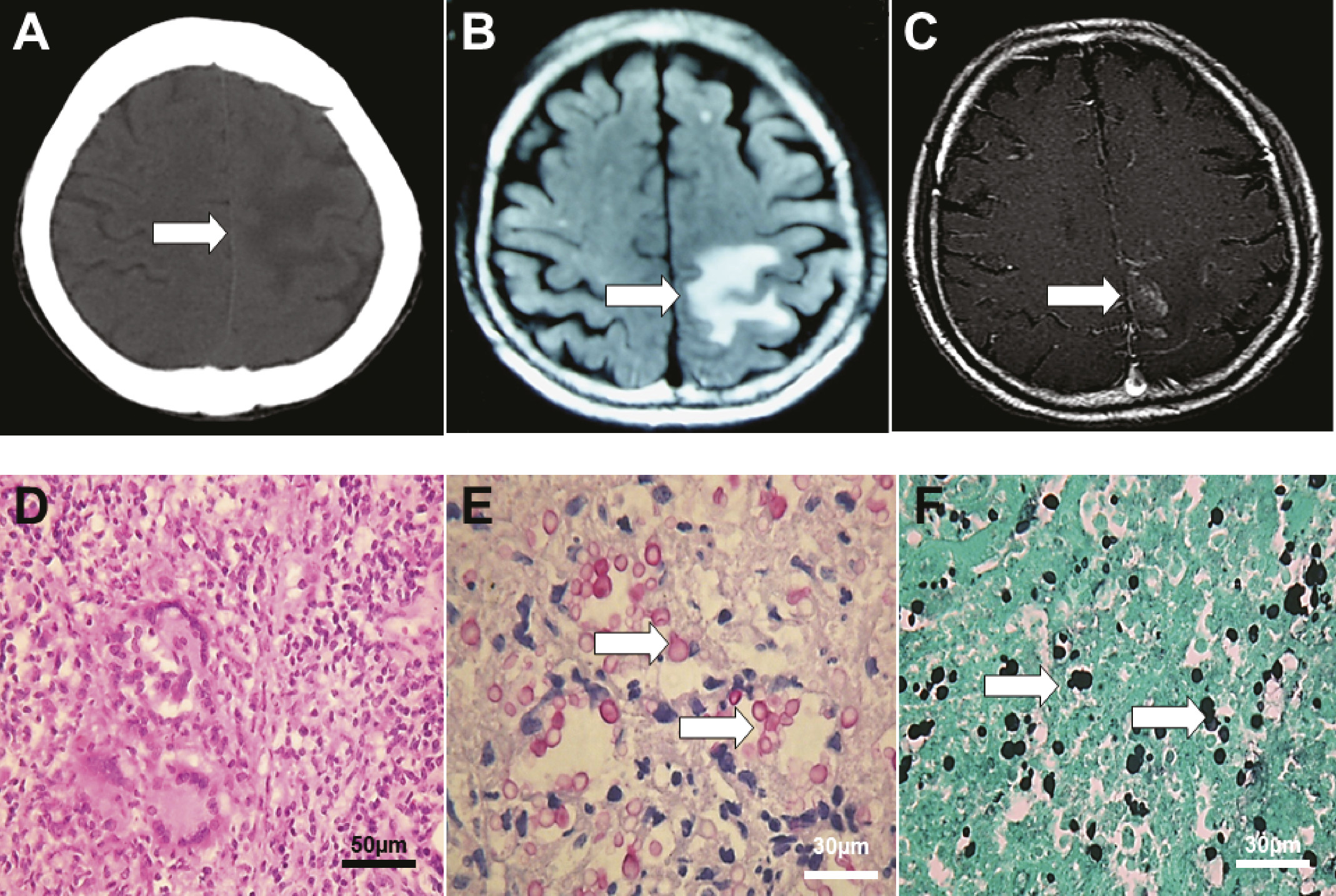
Laboratory tests showed that the patient’s hematocrit was 0.37, and the white cell count was 6600/mL, with 68% neutrophils, 2% eosinophils, and 24% lymphocytes. Repeated tests for HIV were negative. CT scans (
Figure 1A) and MRI scan showed a single mass with focal white matter edema located at the left parietal lobe adjacent to the falx cerebri (
Figure 1, B and C). A brain tumor was suspected, and a neurosurgeon was then consulted for excision at the sixth day after admission. Histopathology results showed acute and chronic inflammation with necrosis and granulomatous inflammation (
Figure 1D); Periodic acid-Schiff stain and Grocott's methenamine silver stain were positive for Cryptococcus elements (
Figure 1, E and F). Intravenous fluconazole therapy was started after surgery. The patient died from systemic sepsis at the 17th day after surgery.
Discussion
Cryptococci prey on individuals with abnormal cell-mediated immunity caused by a variety of debilitating conditions. The major cause of immunocompromise is AIDS in both western
3 and eastern countries.
4 Majors symptoms are headache (83%), vomiting (65%), proptosis (48%), and visual disturbance (48%).
5 Yu et al.
4 reported that two-thirds of patients presented with the triad of fever, headache, and neck rigidity.
This case is very unique because the patient never complained about headache, fever, or visual problems except for weakness in his right limbs and his brain scan showed a locus resembling a malignant or metastatic tumor that mimics that of a central necrotic brain tumor rather than a pygenic brain abscess. The patient’s living space was free from pigeons and domestic fowl. The laboratory tests showed no HIV antibody in his serum. He had no diabetes, malignancies, or hematological disorders.
In conclusion, cryptococcosis is easily misdiagnosed in HIV-negative patients because cerebral cryptococcoma is rare in HIV-negative patients, and there is a misconception that the disease affects mainly immunocompromised individuals.