To our knowledge, this is the first report of altered sports-related behavior secondary to bvFTD. There are reports of preserved golf skills in a patient with short-term amnestic deficits secondary to Alzheimer’s disease
5 and in a patient with bvFTD and semantic deficits.
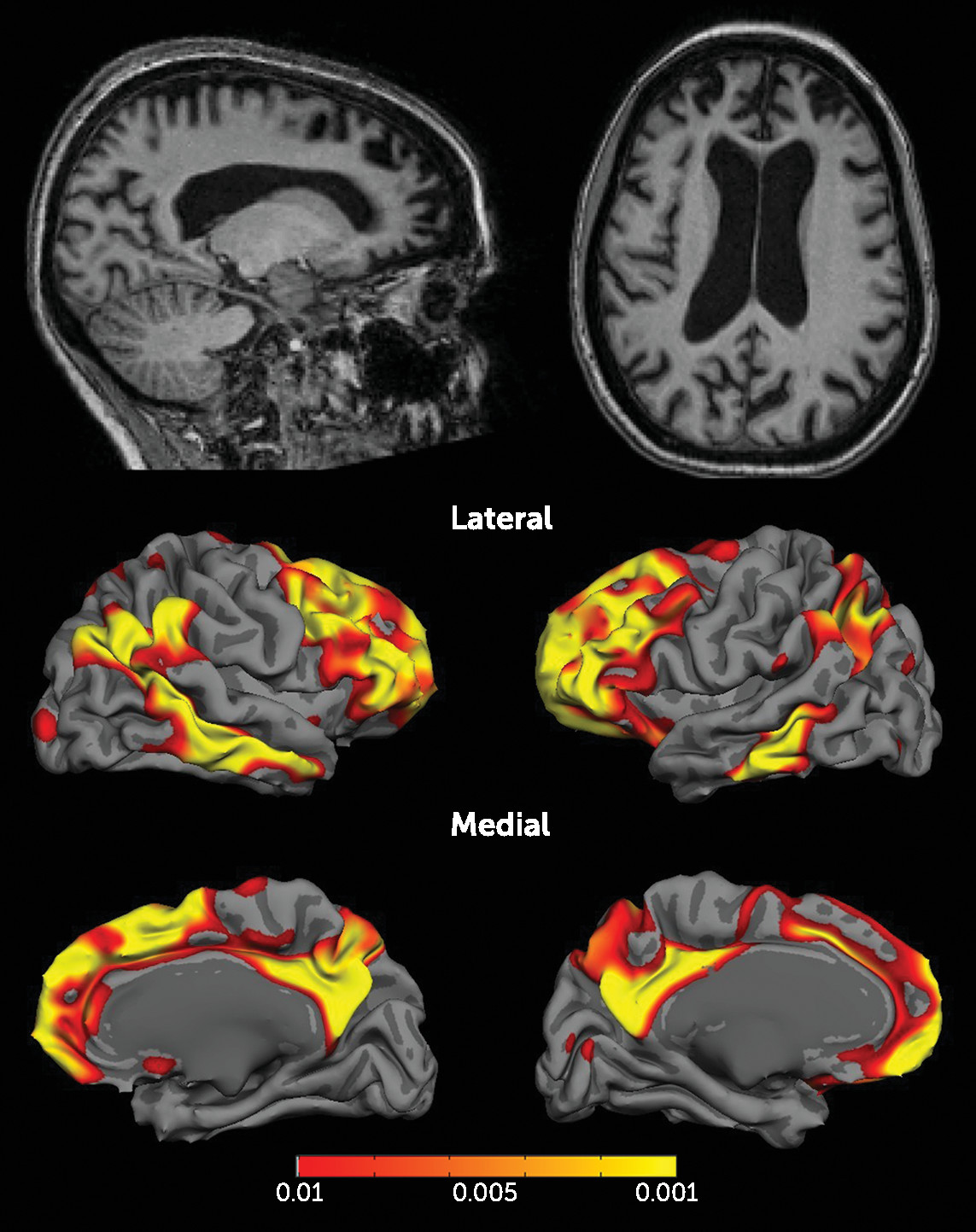
6 In our case, implicit procedural skills and semantic memory for tennis were preserved, but the patient lost monitoring skills as a result of distractibility and executive deficits. The preservation of her motor abilities is striking in light of her significant frontoparietal atrophy, which is probably explained by the relative sparing of the primary motor/sensory strip and basal ganglia (
Figure 1). The preservation of semantic memory is consistent with the limited left temporal pole involvement.
The improvement of her game was attributable to a loss of self-doubt and inhibitions that can stifle performance in sports, which relates to the concept of flow.
4 Flow is the state of experience of total absorption by an activity, accompanied by feelings of control, joy, and time distortion.
4 A player experiencing flow will be perceived as playing effortlessly, intuitively described as “playing out of his or her mind.” Sports psychologists try to help athletes reach this mental state, in which one enjoys the game without being overly concerned with the opponent and consequences of winning/losing. Negative self-inhibiting cognitions most likely involve the dorsolateral prefrontal cortex, and it has been hypothesized that flow could be related to decreased frontal activity.
7 Although there are inherent limitations to studying this subjective state with neuroimaging,
8 this case provides some support for this hypothesis. This patient’s severe bilateral dorsolateral prefrontal cortex atrophy seems to prevent her from engaging in self-defeating cognition. In addition, flow is associated with a transient dissociative loss of self-awareness,
4 which parallels the sustained loss of self-awareness in bvFTD. It is conceivable that atrophy in medial frontal areas involved in social cognitive skills
9 and risk/reward analyses (orbitofrontal cortex)
10 are responsible for her lack of consideration for the opponent and her loss of the fear of losing.
As demonstrated by this case, athletic activities can provide a real-life experiment to detect early social cognitive deficits (e.g., respect for rules/norms, risk/benefit assessments, and theory of mind). We argue that behavioral changes in sports and games should be explored during the clinical assessment of bvFTD. Finally, this case provides a heuristic lesion-based model of the neurobiology underlying flow.
4