To the Editor: Besides tremor, movement disorders are uncommon in multiple sclerosis (MS) being even rarer at the disease presentation.
1 We describe a patient with a history of recurrent major depression that, during treatment, developed excessive eye-blinking. This finding led to the diagnosis of a primary progressive MS.
A 55-year-old Caucasian woman was observed because of a major depressive episode with suicidal ideation. At this time, the patient disclosed a progressive 4-months history of excessive eye blinking and mild gait difficulties. She had a past medical history of chronic obstructive pulmonary disease and a 5-year history of recurrent major depressive disorder on treatment with paroxetine 20 mg q.d. during the last 2 years. There was no other history of psychiatric or tic disorder. Neurological examination disclosed a slow, wide-based gait. There was a slight paresis of left hip flexion (4+/5), with generalized brisk osteotendinous reflexes. There were no other focal signs. Simultaneously, excessive suppressible, eye-blinking movements (more than 1 blink/second) classified as tics were observed, with both a clonic and a dystonic component.
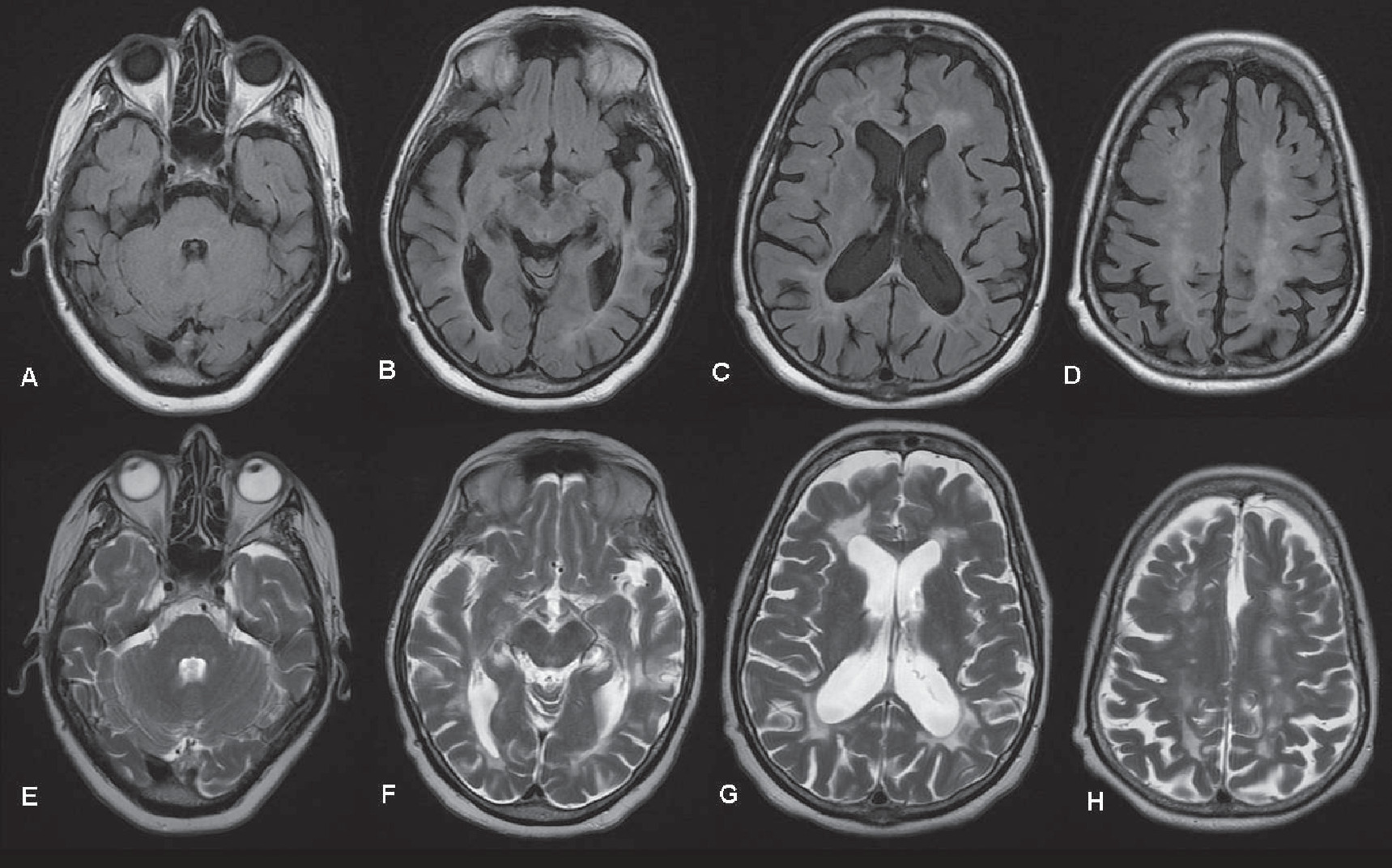
Brain MRI revealed multiple hyperintense lesions in T2-weighted images suggestive of MS (
Figure 1). The cerebrospinal fluid (CSF) study showed a protein content of 29 mg/dL and no cellular content. Oligoclonal IgG bands were found in the CSF. A diagnosis of probable primary progressive multiple sclerosis (PPMS) was made. McDonald 2010 criteria for PPMS were fulfilled on follow-up. Complementary testing was negative for other causes.
The patient stopped paroxetine and was started on mirtazapine 15 mg and venlafaxine 150 mg, with a clear reduction of the excessive eye movements. Nine months after discharge she maintains infrequent subtle dystonic tics.
Tics can be a secondary manifestation of many CNS disorder, including neurodegenerative, metabolic, infectious, or inflammatory disorders. Adult-onset tics are rare, and a de novo presentation should always lead to a search for a secondary cause.
2Neurophysiology and functional studies support a network dysfunction involving the cortical-basal ganglia and limbic-motor circuits in tic disorders.
3 Simultaneously, clinical evidence and molecular imaging studies support a role for dopamine in tics.
4 Paroxetine, a selective serotonin reuptake inhibitor (SSRI), was associated with tics relapse in patients with a previous history of a tic disorder,
5 possibly related to its affinity for the dopamine transporter (DAT), enhancing dopaminergic transmission.
We propose that in this patient, MS progression induced the accumulation of multiple lesions in prefrontal and frontostriatal connections providing the anatomofunctional structure for a tic disorder. Facing the increase in lesion burden, paroxetine dopamine-enhancing activity facilitated the manifestation of clinically significant tics. The notable improvement, but not disappearance of tics, with the suspension of paroxetine raises the hypothesis of a relationship of this drug with the tic severity, in the presence of a chronic secondary tic disorder.
To our knowledge, tic disorders were never described as a primary manifestation of MS. This report expands the spectrum of the differential diagnosis of adult-onset tic disorders.