To the Editor: Catatonia is a harmful medical condition that is characterized by abnormality of movement and behavior arising from either neurological or psychiatric conditions. Catatonia includes behavioral, motor, cognitive, affective, and sometimes autonomic disturbances.
1 Pooled case reports suggest that catatonia owing to an underlying general medical condition or resulting from a psychiatric disorder can be treated similarly, and the catatonic symptoms as well as the underlying illness must be addressed in both types. As highlighted by Northoff,
2 catatonia is theoretically related to complex dysfunction or change in “top-down modulation” mechanisms. This change, which reflects “vertical modulation” of caudate and other basal ganglia by GABA-ergic mediated orbitofrontal cortical deficits, may lead to motor symptoms commonly observed in catatonia. We report a case of a 47-year-old man presenting to the emergency room with catatonia.
Case Report
The patient presented to the emergency room because he had headaches, diminished movements, mutism, and automatisms for the last month, with intensification of symptoms in the last 5 days. He was diagnosed with paranoid schizophrenia 20 years ago, and he had received pharmacotherapy with first-generation antipsychotic drugs, including haloperidol (up to 15 mg/daily for 6 months) and chlorpromazine (up to 600 mg/daily for 6 months), since this diagnosis. However, clinical efficacy was limited because of adverse effects. In fact, extrapyramidal symptoms secondary to both first-generation drugs led to treatment discontinuation. By that time, the patient underwent a new treatment protocol with risperidone, which would theoretically cause fewer extrapyramidal symptoms. After 4 months of treatment, a dose of 6 mg was reached. The patient presented with clinical amelioration of his symptoms and no adverse effects were reported.
For the last 15 years, the patient had received community treatment with risperidone (6 mg/daily), but his condition evolved with some episodes of reacutization of symptoms after the medication was discontinued. Whenever there was intensification of psychiatric symptoms, they were characterized by persecutory delusions, auditory hallucinations, and cognitive impairment. During this time, risperidone was used as monotherapy and the patient showed amelioration of psychotic symptoms after the drug was reintroduced. The patient had no history of catatonia or other neurological symptoms.
In the last year, the patient’s parents reported that he was not receiving any pharmacological treatment because of his persecutory delusions. The family managed the patient's care, however challenging, at home without medical assistance. In the last month, the clinical scenario evolved with new unusual features that were not previously present. The patient’s symptoms included headaches, rigidity, posturing, negativism, staring, diminished movements, and automatisms with a worsening pattern in the last 5 days. The patient could not eat by himself, exhibited stereotypical movements, and was unable to establish verbal communication. In fact, the patient manifested echolalia (i.e., automatic repetition of vocalizations made by another person). Considering both the new pattern of symptoms and the severity of the clinical scenario, the family finally decided to seek medical attention for the patient.
Given the presence of catatonic symptoms, the patient underwent an investigation protocol with a neuroimaging assessment (CT scan), laboratory tests, and an EEG study. The evaluation protocol followed a normative guideline in our academic service to adequately assess the etiology of catatonia. This protocol follows recommendations that were previously reported in the medical literature.
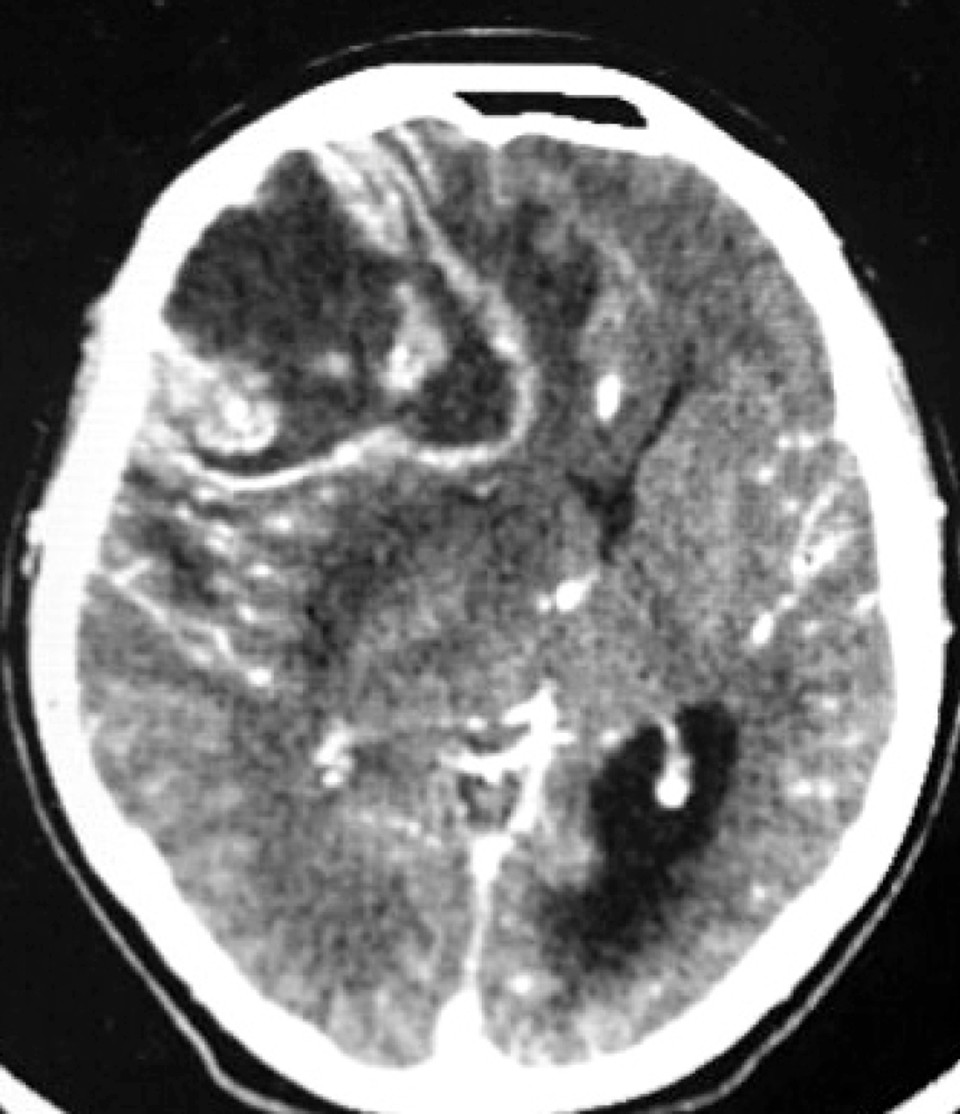
3 Results on complementary examinations showed an expansive lesion at the right frontal cortex with compression and displacement of normal brain tissue (
Figure 1). All laboratory and EEG test results were normal. The patient underwent a surgical procedure with both diagnosis and treatment proposals. Surgical pathology results confirmed glioblastoma multiforme. By the time this case was reported, the patient was still receiving intensive care treatment.
Discussion
Catatonia may follow nonpsychiatric conditions such as brain tumors, neuroinfections, encephalopathy, stroke, Parkinson’s disease, and nonconvulsive status epilepticus. Treatment of the underlying condition usually resolves catatonic symptoms and also portends outcome. Physicians should screen patients who are suspected to have an occult medical cause of catatonia, with a focus on the patient’s history, vital signs, and neurological examination. Serum electrolyte measurements and toxicology screens may be useful in ruling out metabolic or toxic causes.
4A review of 261 published cases of catatonia found that no relevant psychiatric disorder was associated with the catatonic state in 75% of patients.
5 The most common cause of catatonia was injury to the CNS, whether from stroke, trauma, vasculitis, tumor, or anoxia.
A recent critical literature review also highlighted that catatonia disorder resulting from general medical conditions should be considered in every patient with catatonic signs.
6 Catatonia is associated with significant morbidity and mortality if left untreated. Evidence indicates that the risk for permanent disability increases after 4 days of persistent catatonia. The long-term course of catatonia is also determined by the etiology of the syndrome. An etiological evaluation in patients manifesting catatonia should be performed rapidly to guide adequate treatment protocols.