DSM is a classification system of psychiatric disorders based on the clustering of psychiatric symptoms in patients as observed by clinicians.
1 There is a growing body of evidence, however, that a factor structure underlies, and can cut across, DSM diagnoses.
2–4 It has been hypothesized, but not yet tested, that these factors underlying DSM diagnoses will be more closely associated with the neuroanatomical bases of psychiatric symptoms than DSM diagnosis. In the current study, we determined the factor structure of psychopathology underlying the DSM diagnoses of 199 Vietnam War veterans who suffered penetrating brain injuries and 55 matched control participants. We then determined which neuroanatomical structures, when damaged, were associated with higher or lower factor scores compared with participants without damage to that structure. We also compared the ability of DSM-IV categorical diagnoses, factors derived from DSM-IV diagnoses, and continuous self-report measures of depressive and anxiety symptoms to predict the neuroanatomical findings. This study had two goals: 1) to determine which specific brain regions are associated with core components of psychopathology and 2) to compare the ability of categorical DSM-IV diagnoses, factor scores underlying these diagnoses, and self-report of continuous measures of psychopathology to account for the neuroanatomical findings in patients with penetrating brain injuries.
Although there is significant overlap between the functions of specific brain areas and circuits, animal, human functional imaging, and lesion studies suggest that certain brain areas and circuits are preferentially associated with emotional and behavioral domains. These include structures that are involved in fear and arousal including the amygdala,
5 structures involved in reward learning such as the hippocampus,
6 and areas involved in decision making and reward processing such as the orbitofrontal cortex (OFC).
7 A premise of this study is that damage to different brain structures involved in emotion, arousal, and reward in humans will predispose to, or protect from, the development of specific psychiatric syndromes and symptoms.
8The National Institute of Mental Health’s Research Domain Criteria (RDoC) initiative is designed to redefine psychiatric syndromes on the basis of their underlying neural circuitry. Lesion studies, such as the current study, are an important component of this redefinition. The current study embodies the RDoC principles because it uses dimensional measures of psychopathology in addition to categorical measures, integrates neural circuits and observable behaviors, is translational, measures a spectrum of psychiatric symptoms, and defines a sampling frame (Vietnam veterans with brain injury and psychiatric illness).
Previous researchers have assessed the factor structure of DSM diagnoses.
2–4 There is not exact agreement about the underlying factor structure of psychiatric illnesses; however, a five-factor model
3 derived from Structured Clinical Interviews (SCIDs) with a large group of patients with axis I and II diagnoses has been replicated and demonstrated reliability and validity.
4,9 The factors, and the categorical disorders they encompass, are internalizing (anxiety and eating disorders, major depressive disorder, and borderline, paranoid, dependent, and obsessive-compulsive personality disorders), externalizing (substance use disorders and antisocial personality disorders), thought disorder (psychosis, mania, and paranoid, schizoid, and schizotypal personality disorders), somatoform (somatoform disorders), and antagonism (paranoid, antisocial, borderline, histrionic, and narcissistic personality disorders).
3 The factor structure underlying DSM diagnoses appears to be stable across time
10 and demonstrates cross-cultural validity.
11In the current study, we first attempted to replicate this factor structure in 254 Vietnam War veterans. Brain-behavior correlational studies in individuals with penetrating brain injury have been limited, and therefore we then determined whether damage to specific brain areas involved in behavior and emotion was associated with lower or higher scores on each factor. We hypothesized that damage to brain regions associated with emotional and behavioral function including the limbic and ventral frontal, but not control brain regions, such as the occipital cortex, would be associated with differential effects on core factors underlying DSM diagnoses. On the basis of previous research demonstrating an association between aggression and damage to the OFC in traumatic brain injury,
12 we hypothesized that damage to this region will be associated with increased externalizing symptoms. On the basis of large amounts of literature linking the amygdala to fear learning and negative valence,
5,13 we hypothesized that damage to this structure would reduce fear responsiveness and thus internalizing symptoms. Finally, we compared the ability of the identified factors with DSM diagnoses and self-report measures of depressive and anxiety symptoms to predict the degree of damage in affected brain areas.
Methods
Participants were seen as part of the W.F. Caveness Vietnam Head Injury Study, a longitudinal study of brain-injured veterans. This study had several phases of evaluation. The data for the current study were taken from phase III, conducted from 2003 to 2006 at the National Naval Medical Center in Bethesda, MD. During phase III, a Structured Clinical Interview for DSM-IV Patient Edition (axis I) (SCID-I/P)
14 was administered to all participants by a psychiatrist trained to administer the SCID (V.R. or E.D.H.). All participants also received extensive neuropsychological testing.
15 Of the 254 participants evaluated in phase III, 55 were combat-matched control participants and 199 had suffered a brain injury. The control participants had served in Vietnam during the same years as the head-injured patients, were of the same age, and had comparable combat exposure.
Table 1 provides the characteristics of the participants. All of the participants were used to derive the factors, but only the brain-injured patients were used in the imaging analysis. All study procedures were approved by the Institutional Review Board of the National Naval Medical Center. All participants gave written informed consent in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
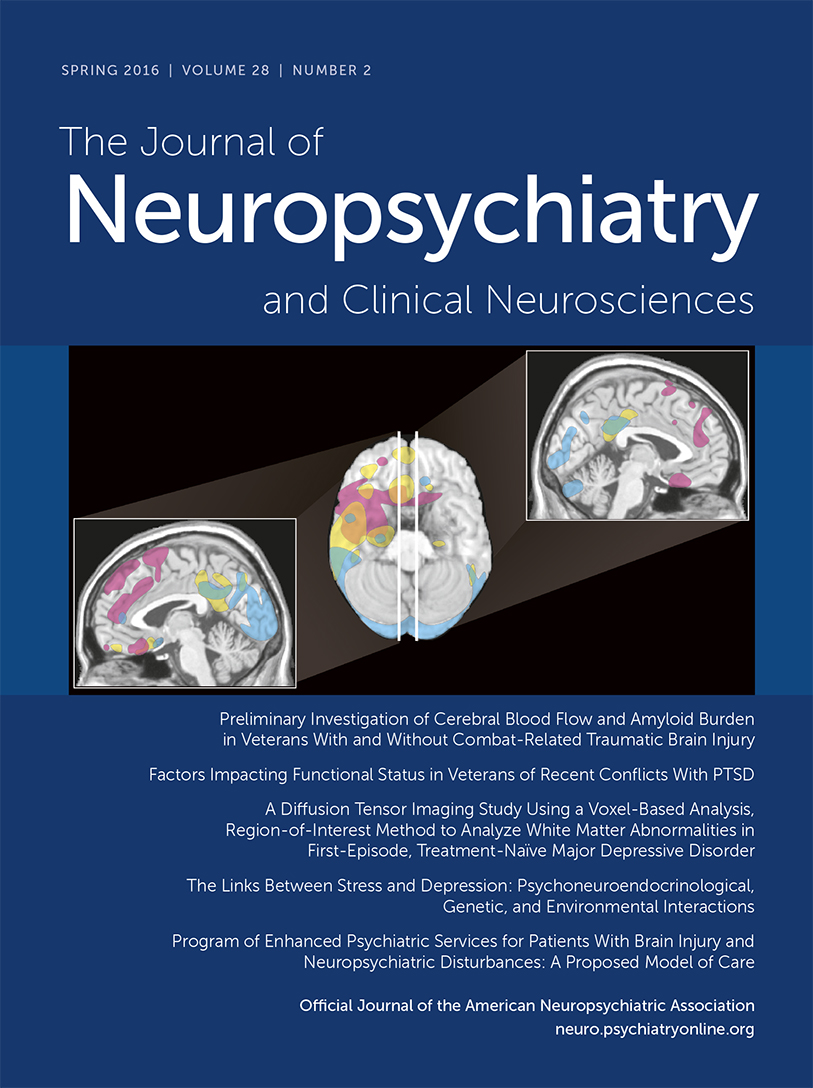
All of the brain-injured participants received an axial noncontrast CT scan during phase III on a GE Medical Systems Light Speed Plus CT scanner in helical mode. CT was used because many of the participants had residual metal in their heads, precluding MR imaging. Images were reconstructed with an in-plane voxel size of 0.4×0.4 mm, overlapping slice thickness of 2.5 mm, and a 1-mm slice interval. Lesions were manually traced by one of the authors (V.R.) and reviewed by another author (J.G.), who was blind to the results of the clinical evaluations. Percentages of each Brodmann's area damaged were determined using the Analysis of Brain Lesions (ABLe) software.
15,16 [Raymont et al.
15 provide more details of the procedure.] All participants gave informed consent, and all procedures were approved by the appropriate institutional review board.
Each psychiatric diagnosis coded by the SCID was determined to be present or absent, and these data were used in the factor analyses. Only axis I diagnoses obtained from the SCID performed during phase III were used (we did not collect information on axis II personality disorders). Lifetime as well as active diagnoses were used (i.e., a participant who was judged as meeting criteria for posttraumatic stress disorder (PTSD) 20 years before phase III who no longer met criteria would be considered positive for PTSD, as would a participant with current PTSD that developed 1 year before evaluation). If a patient met criteria for more than one psychiatric disorder, all disorders were included in the analyses. We required that diagnoses meet the following characteristics to be included in the factor analysis: meet full DSM criteria for the disorder (subthreshold diagnoses were not used), affect at least 10 participants, and not be substance induced or induced by a medical condition or not otherwise specified. We used substance abuse diagnoses separately from alcohol abuse. In addition, we collapsed the individual substance abuse diagnoses (e.g., cocaine abuse, marijuana abuse) into a single variable of substance abuse, which was coded as present or absent. The following axis I diagnoses met these criteria and were included in the factor analysis: major depressive disorder, psychosis, alcohol abuse, substance abuse, panic disorder, social phobia, specific phobia, and PTSD. To identify latent factors of DSM diagnoses, each psychiatric diagnosis item was modeled using a two-parameter logistic model based on item response theory.
17 The estimation was done in the mirt R package,
18 and the loading matrix was rotated using oblique rotation. The chi-square test was used to test model fit.
The 23 neuroanatomical regions of interest (ROIs) were defined before the analysis. The ROIs provide whole-brain coverage except for the cerebellum. We identified ROIs that have been associated with psychiatric symptoms both from the RDoC workshops and from a large functional imaging literature in humans associating brain regions including the amygdala, basal ganglia, hippocampus, thalamus, insula, orbitofrontal cortex, dorsolateral prefrontal cortex, and cingulate cortex with psychiatric symptoms (anatomic definitions of the ROIs are included in
Table 2). This literature is too large to review here, but readers are referred to the RDoC workshop source documents for further discussion (
www.nimh.nih.gov/research-priorities/rdoc/index.shtml). The distinction between the ventral and dorsal striatum is behaviorally salient, but we did not have patients with ventral striatal damage isolated from dorsal striatal damage; therefore, the more general designation “basal ganglia” was used. As control ROIs, we used the parietal, temporal, and occipital cortices. The laterality of the cortex and amygdala (left or right) was coded because no participants had bilateral amygdala involvement, but lesions of other subcortical structures were not lateralized because they were commonly bilaterally involved. This resulted in the identification of 23 neuroanatomical regions serving as potential correlates of psychiatric symptoms: 1) cortical areas (left and right anterior cingulate, posterior cingulate, insula, medial OFC, lateral OFC, dorsolateral prefrontal cortex, temporal, parietal, and occipital lobes [18 regions]) and 2) subcortical regions (left and right amygdala, and bilateral basal ganglia, thalamus, and hippocampus [5 regions]). For all 18 cortical areas, we summed the percentage of each component Brodmann area lesioned to arrive at a total “lesion score” for each cortical ROI. That is, if a Brodmann area were entirely involved by the injury, it would have a percentage of 100%, and if 50% of the volume were involved, the percentage would be 50%. Because of difficulty in determining percentage involvement of the subcortical structures, involvement of the subcortical structures was coded as absent (0) or present (1). Hence, for both the cortical and subcortical ROIs, a higher lesion score indicates more severe damage. Partial correlations were performed between the proportion of damage to each region and the derived factor values, controlling for age, education, global cognition (defined as the total score on the Mini-Mental State Examination [MMSE]), and total percentage of the entire brain lesioned by injury. We did not correct for multiple comparisons because the analysis was hypothesis driven. We then performed hierarchical linear regressions to compare the relative abilities of three measures to predict the lesion scores in the brain regions identified in the partial correlations: 1) factor scores, 2) individual DSM diagnoses that significantly weighted on those factors, and 3) continuous symptom measures of depression and anxiety (the Beck Depression Inventory [BDI] II total score
19 and the Hamilton Anxiety Scale Total score
20).
Results
The exploratory factor analysis suggested that a two-factor model was the best fit (Bayesian Information Criterion [BIC]=1827, χ
2(6)=7.52, p=0.28), compared with a three-factor model (BIC=1753.2).
Table 3 shows the factor loadings. Factor loadings with an absolute value >0.5 were considered significant. All significant factor loadings were positive (
Table 3). For factor 1, significant factor loadings were major depressive disorder, panic disorder, social phobia, and PTSD. This factor was labeled internalizing because of its correspondence with the internalizing factor defined in previous studies.
3 The second factor demonstrated significant loadings with alcohol and substance abuse and is termed externalizing because of its similarity with the previously defined factor.
3 We did not identify the somatization or antagonism factors identified by Kotov et al,
3 but this was expected because the diagnoses that form the basis of these factors (somatoform and personality disorders) were not included in this analysis. Very few of the participants met criteria for somatoform disorders, and we did not assess personality disorders. We also did not detect the thought disorder factor in the two-factor model.
Table 2 shows all partial correlations between the brain ROIs and factor scores. We controlled for overall cognition (with the total MMSE), education, age, and total percentage of brain lesioned. We found significant negative correlations between the internalizing factor and damage to the left amygdala (
r=–0.187, p=0.02), and bilateral basal ganglia (
r=–0.185, p=0.02), indicating that higher lesion scores were associated with lower internalizing. We also found a negative correlation between the externalizing factor and the bilateral hippocampi (
r=–0.164, p=0.037) and a positive correlation with the left medial OFC (
r=0.165, p=0.04), indicating that higher lesion scores for the bilateral hippocampi were associated with a decrease in externalizing and for the left medial OFC, an increase in externalizing. There were no other significant partial correlations.
The amygdala and basal ganglia are adjacent and are frequently injured together in penetrating injury. To better understand whether damage to the amygdala or basal ganglia was driving the association with the internalizing factor, we performed stepwise multiple regressions with lesion score in the left amygdala and bilateral basal ganglia as the independent variable and the internalizing factor score as the dependent variable. The model using only the left amygdala accounts for the majority of the variance (R2=0.032, F=5.834, p=0.012) compared with the model with the left amygdala and bilateral basal ganglia (R2=0.048, F=4.456, p=0.01).
We next performed linear regressions with the lesion scores in the left amygdala, bilateral basal ganglia, bilateral hippocampi, and left medial OFC as the outcome and the factor scores derived from the DSM diagnoses, the presence or absence of the DSM diagnoses themselves, and dimensional measures of symptoms of depression and anxiety (total BDI II and total Hamilton Anxiety Scale) as the predictors to determine the ability of these measures to predict the anatomical findings (
Table 4). As defined by the adjusted
R2, factor scores best predicted left amygdala and bilateral hippocampal involvement, whereas DSM diagnoses best predicted bilateral basal ganglia and left OFC involvement (
Table 4).
Discussion
This study had two goals: 1) to determine which specific brain regions are associated with core components of psychopathology and 2) to compare the ability of DSM diagnoses, factor scores, and self-report measures of psychopathology to account for the neuroanatomical findings of our participants. We found a similar structure in our veterans as found by other researchers in their neurologically intact psychiatric outpatients,
2–4 suggesting that these factors are valid measures of psychopathology in our population. The two factors we identified correspond to the previously defined internalizing and externalizing factors underlying psychiatric diagnoses.
3 Damage to the left amygdala was associated with decreased internalizing. The association between the left amygdala and internalizing agrees with a previous study from our group in these participants that demonstrated a markedly decreased prevalence of PTSD in those with amygdala damage.
8 The amygdala plays a key role in arousal and fear response
21 and is crucial for the acquisition of conditioned fear in animals.
22 The amygdala is a central brain region involved in the Negative Valence domain of the RDoC initiative. We could expect that damage to the amygdala would interfere with both normal and pathological arousal (e.g., PTSD) and, thus, would be associated with decreased internalizing, especially in comparison to a control group of combat-exposed veterans with a high prevalence of PTSD, as in the current study.
In previous studies, the externalizing factor has been associated with alcohol and substance abuse and antisocial personality disorder.
3 We found that damage to the left medial OFC was associated with increased externalizing and the hippocampus with decreased externalizing. The medial OFC is involved in evaluating expected outcomes of actions, and damage to this region is associated with increased impulsivity and impaired long-term decision making in humans and animals.
23–25 This can be seen clinically in that patients with medial OFC damage often choose to perform actions that provide short-term reward at the risk of future negative consequences
26 and in the laboratory in which these patients demonstrate selective deficits on gambling tasks.
26,27 Substance abuse in humans is associated with decisions with poor long-term consequences and decreased volume in the medial OFC.
28 Previous studies, including in this population, have demonstrated that damage to the medial OFC increases aggression, which is associated with the eternalizing factor.
12,29,30 There is also emerging evidence that damage to the lateral OFC can result in lower levels of aggression.
31 The medial OFC is also closely tied to social cognition, and the interaction of decision making, aggression, and social cognition remains to be clarified.
32 The hippocampus is essential for reward-learning and appears to play an important role in the development of addiction.
33 Damage to the hippocampus could be associated with decreased development of alcohol and substance abuse, as observed in this study.
Imaging studies have indicated the important role of the medial OFC in the self-perception of mood and anxiety.
34,35 Deactivation of this region, especially the subcallosal cingulate, is associated with a decrease of depressive symptoms in patients with severe major depressive disorder.
36 Patients with neurodegenerative disease that affects the OFC (such as behavioral variant frontotemporal dementia) usually demonstrate a syndrome of poor decision making and im-pulsivity similar to the externalizing factor detected in the current study, in addition to emotional blunting.
37 In contrast, patients with subcortical neurodegeneration that initially spares the OFC (such as Huntington’s and Parkinson’s diseases) will usually manifest internalizing symptoms of depression, irritability, and anxiety,
38,39 suggesting that a functioning OFC is necessary both for the normal experience of emotion and the pathological experience of excessive emotion including depression and anxiety.
Factor scores best predicted left amygdala and bilateral hippocampal involvement, whereas DSM diagnoses were associated with bilateral basal ganglia and left OFC involvement. The anatomical measures accounted for a small amount of the variance in the psychiatric measures, stressing the importance of other variables, such as experience and genetics, in the development of psychiatric disorders. There has been extensive debate recently on whether categorical DSM diagnoses or dimensional measures will perform better to elucidate the biological bases of psychiatric symptoms. The data from this study suggest that there may not be a simple answer to that question and the best type of measure to use may vary depending on the symptom of interest and the biological associations investigated (e.g., anatomy and genetics). The self-report measures underperformed the diagnostic measures for all regions. The factor scores, DSM diagnoses, and symptom measures differ in many ways (lifetime versus point prevalence, continuous versus categorical, etc.), and further research is required to determine which of these differences are the most salient to the biological association investigated.
This study had several limitations. First, the number of participants with certain diagnoses (notably somatoform and eating disorders) was insufficient to derive factors detected by previous analyses,
3 and some diagnoses (e.g., psychosis) were rare, possibly underpowering the ability to detect some anatomical associations. Also, we did not assess personality disorders. Second, the brain injuries were not randomly distributed, and some brain areas were overrepresented and others underrepresented in this sample (
Table 1). Third, although our factor scores provided continuous measures of psychopathology, they were derived from categorical DSM diagnoses with all of their inherent limitations including a dichotomous outcome and questionable generalization to people without psychiatric disorders. Third, we did not exclude participants with psychiatric illness that preceded their brain injury. Finally, our participants were all men in their sixth decade of life who experienced significant psychological, and most of them physical, combat trauma. They were at elevated risk for externalizing disorders but had a reduced risk for internalizing disorders compared with women.
40 A criticism of studies of the association of individual ROIs and psychiatric symptoms has been that brain circuits, rather than individual regions, are likely most associated with psychiatric symptoms.
41 We agree with this viewpoint, but brain circuits are composed of individual regions, each of which likely contributes a unique component to psychiatric syndromes. Thus, studies of individual brain regions and structures can be complementary to analyses of circuits.
41The results suggest that DSM-based categorical diagnostic approaches can be useful in evaluating psychiatric symptoms. The observed associations between the anatomical regions with brain lesions and psychiatric diagnoses are consistent with a large scientific literature associating limbic structures including the amygdala, hippocampus, and OFC in mood and anxiety disorders. Traumatic brain injury does not always increase psychopathology. Damage to some structures (e.g., the left amygdala in the current study) can result in decreased psychiatric symptoms, likely through disruption of normal emotional responses. These results agree with previous findings associating the amygdala with the Negative Valence Domain of the RDoC initiative. Further studies of anatomy and pathophysiological changes, particularly with longitudinal follow-up, may help to clarify the brain mechanisms underlying psychiatric disorders and improve the accuracy of psychiatric diagnosis and future therapeutics.