Anti-NMDA Receptor Antibody Positivity and Presentations Without Seizure, Involuntary Movement, Hypoventilation, or Tumor: A Systematic Review of the Literature
Abstract
Materials and Methods
Search
Study Selection
Data Extraction
Results
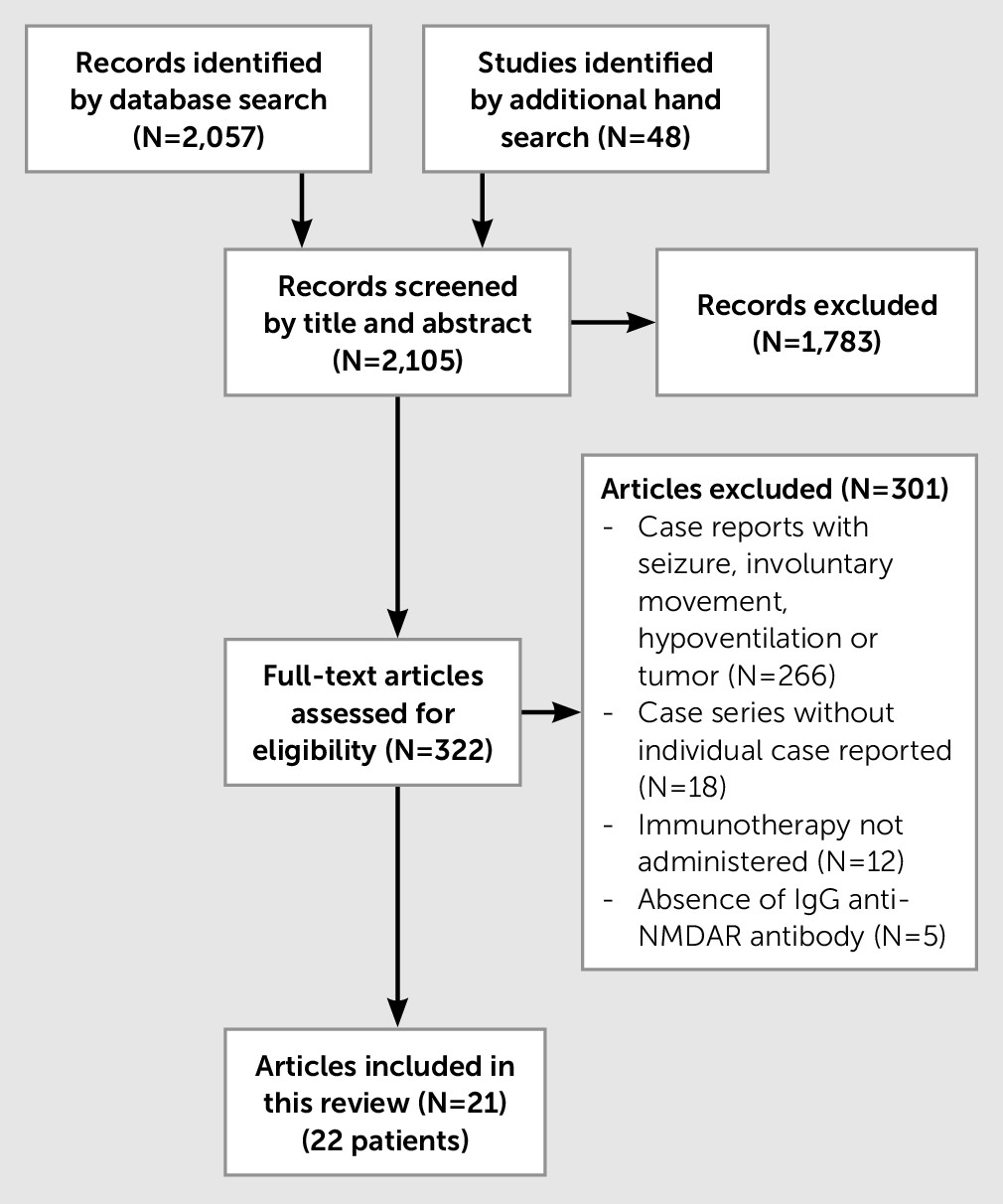
Literature Search
| Case No./Author/Publication Year | Sex/Age (Years) | Duration of Illness | Initial Diagnosis/Comorbidity | Psychiatric and Cognitive Symptoms | Neurological and Motor Symptoms | Abnormal Results for CSF/MRI/EEG | Anti-NMDAR/Abnormal Serum CSF | Immunotherapy (Order of Treatment) | Time From Initial Immunotherapy Until Clinical Improvement | Immunotherapy Response |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Zandi et al./20117 | Male/19 | 3 months | SCZ/– | Auditory hallucinations, thought disorder, grandiose delusions, deficits of recall and verbal fluency | Nil | NA/NA/NA | +/NA | PE, steroids | 3 weeks | Very much improved |
| 2. Suzuki et al./20118 | Female/70 | 6 months | NA/SSc | Dementia (10/30 on MMSE) | Ataxia, tremor, rigidity, muscle weakness | +/+/ NA | +/+ | Steroids, CTX | NA | Very much improved |
| 3. Lekoubou et al./20129 | Female/34 | 1 month | ADEM/– | Psychomotor agitation, echolalia and echopraxia, incoherent speech, delusions of persecution | Walking difficulties, disorientation, cerebellar ataxia, hemiparesis | +/+/NA | NA/+ | IVIg, steroids, RTX | <6 months | Much improved |
| 4. Lebon et al./201210 | Female/16 | 2 months | Primary psychotic disorder/– | Mutism, refusal to eat, infantile behavior, auditory hallucinations, incoherent speech, memory impairment, executive deficit, attention deficit | Nil | –/–/+ | +/NA | Steroids, IVIg | 9 months | Very much improved |
| 5. Yuan et al./201311 | Female/22 | 3 weeks | NA/– | Affective lability, grandiose thoughts, paranoid delusion, auditory and visual hallucinations, deficits of verbal fluency, visuospatial deficit, hemispatial neglect, memory impairment | Nil | +/–/+ | NA/NA (Positive in serum or CSF or both) | Steroids, IVIg, PE, RTX | 6 months | Much improved |
| 6. Yau et al./201312 | Female/5 | 1 week | NA/– | Fluctuating level of consciousness, mutism, impaired speech, irritability | Nil | +/–/+ | –/+ | IVIg | 1 week | Very much improved |
| 7. Tüzün et al./201313 | Female/42 | 2 weeks | NA/– | Mild Executive Deficit | Double vision, difficulty walking, limited vertical gaze | +/+/– | +/+ | Steroids | 2 months | Very much improved |
| 8. Leypoldt et al./201314 | Male/24 | 1 day | Relapse of HSVE/– | Mania, irritability, racing thoughts, pressured speech, memory impairment, attention deficit | Nil | +/+/– | +/+ | Steroids | 1 week | Much improved |
| 9. Kayser et al./20135 | Male/19 | 2–3 months | Demyelinating disease/– | Aggression, excessive eye blinking, grandiosity, delusional thinking | Nil | +/+/– | +/NA | Steroids, AZA | 9 months | Very much improved |
| 10. Kayser et al./20135 | Female/20 | NA | NA/– | Delusion, depression | Nil | +/+/NA | +/+ | Steroids, IVIg, RTX, MMF | NA | Very much improved |
| 11. Kuppuswamy et al./201415 | Male/35 | 2 weeks | Primary psychotic disorder/– | Depression, suicidality, grandiosity, impulsivity, mutism, posturing, staring, ambitendency | Nil | –/–/– | +/+ | Steroids, PE, AZA | 4 months | Very much improved |
| 12. Finke et al./201416 | Male/67 | 2 weeks | HaNDL/– | Confusion, agitation, aggressiveness, retrograde amnesia, memory impairment, attention deficit | Transient hemiparesis, transient aphasia | +/–/+ | –/+ | Steroids, PE, AZA | 6 weeks | Much improved |
| 13. Byrne et al./201417 | Male/4 | 2 days | NA/– | Confusion, agitation | Dysphasia, coma | –/+/+ | +/NA | Steroids | 4 days | Very much improved |
| 14. Takeda et al./201418 | Male/35 | 6 days | Herpes encephalitis/– | Delirium, violent behavior, delusions, disorientation | Diplopia, paraparesis, hypoesthesia, ptosis | +/+/NA | NA/+ | Steroids, PE, CTX | 12 months | Much improved |
| 15. Fleischmann et al./201519 | Female/37 | 5.5 years | NA/MS and SS | Delusions, bizarre behavior, aggressiveness, memory impairment, Dementia (14/30 on MMSE), disorientation, executive deficit | Gait ataxia, dysarthria | +/+/ NA | +/+ | Steroids, AZA, CTX, NTL, PE, MTX | Nonresponse | Death (urosepsis) |
| 16. Cuende et al./201520 | Female/61 | 3 months | NA/RA | Memory loss | Dizziness, unsteady gait, muscle weakness, speech problems | +/–/NA | +/+ | IVig | NA | Very much improved |
| 17. Kruse et al./201521 | Female/14 | NA | NA/– | Anxiety, depressed mood, disinhibited and disorganized behavior, reduced verbal output, slow speech, learning difficulty | Transient arm numbness, difficulty with complex motor tasks | +/–/+ | –/+ | NA | NA | Very much improved |
| 18. Sühs et al./201522 | Female/23 | 2 years | Psychiatric disorder/– | Fearful behavior, stereotypical repetitive movements, loss of orientation, memory impairment, executive deficit | Nil | +/–/+ | +/NA | Steroids | 1 month | Very much improved |
| 19. Orengo et al./201523 | Female/29 | 3 months | NA/serum aquaporin-4 antibody positive | Anorexia, abulia, mutism, immobility, nonsensical speech, memory impairment | Imbalance and vertigo, facial numbness, ataxia | +/+/NA | –/+ | Steroids, PE, RTX | NA | Much improved |
| 20. Gahr et al./201524 | Male/34 | 1 week | Psychotic mania/– | Impulsivity, aggressiveness, hostility, dysphoric mania paranoid ideation hyper-religiosity | Nil | +/+/NA | +/+ | Steroids, IVIg | NA | Very much improved |
| 21. Senda et al./Epub ahead of print 20156 | Female/33 | 2 years | SCZ/HT | Auditory and visual hallucination, delusions of persecution, delusion of control agitation, memory impairment, executive deficit | Nil | –/–/– | NA/+ | Steroids, IVIg | 3 months | Much improved |
| 22 Lalanne et al./201525 | Female/31 | NA | Psychotic depression | Melancholia, depression, cenesthopathy, memory impairment, attention deficit | Nil | NA/+/+ | NA/+ | Steroids, IVIg | 5 weeks | Very much improved |
Clinical Characteristics
Test Results
Immunotherapy and Outcome
Discussion
Diversity of Clinical Characteristics
Response to Immunotherapy
Detection of Anti-NMDAR Antibodies
Definition of Atypical Presentations
Conclusions
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).