Interpersonal conflicts and other relational difficulties are important predisposing vulnerabilities or perpetuating factors affecting patients with functional neurological disorder (FND), also referred to as conversion disorder, which is a common neuropsychiatric condition characterized by unexplained limb weakness, gait difficulties, nonepileptic seizures, abnormal movements, or sensory deficits.
1–3 According to attachment theory, interpersonal difficulties may arise throughout the lifespan in part from insecure attachment tendencies based on childhood maltreatment and poor caregiver relationships.
1 While individuals with secure attachment generally enjoy more consistent nurturance in childhood and exhibit a positive view of the self and others,
4,5 adults with insecure attachment experience interpersonal challenges. Those with dismissing attachment are thought to have had early childhood experiences marked by emotionally unresponsive caregiving, resulting in overcompensated self-reliance combined with discomfort in closeness to others.
1,4 Adults with preoccupied attachment are more likely to have had inconsistently responsive caregiving, resulting in overvigilance, poor self-esteem, and a dependence on the approval of others.
6,7 Fearfully attached individuals often experienced affectionless, critical, and rejecting caregiving, thus leaving them with a negative view of the self and others. Adults with a fearful attachment crave social attachments, but are frequently stymied by their fears of intimacy and rejection, resulting in an urge to flee.
8 Although insecure attachment styles have been linked to somatization and emotional dysregulation,
7,9 few studies in FND populations have examined neuropsychiatric factors associated with attachment styles, which are also important considerations affecting doctor-patient encounters.
8While two studies found no differences in attachment styles between patients with epilepsy and those with psychogenic nonepileptic seizures (PNES or dissociative seizures),
10,11 another revealed higher levels of fearful attachment in individuals with PNES.
12 In the latter study, abuse and neglect correlated with insecure attachment.
12 Furthermore, in patients with PNES, depression and anxiety have been linked to avoidant or anxious attachment styles, relationship conflicts and lack of relationship depth, indicating a role for attachment in the development of concurrent psychopathology.
11 In pediatric FND populations, distinct attachment styles may be linked to specific symptom profiles, implying an interplay between relationship difficulties and functional neurological symptoms.
13 The heterogeneity of group-level differences also highlights the importance of considering individual differences in FND populations using a neurobio-psycho-social perspective.
14,15 Additionally, very few studies have investigated attachment styles in other motor FND subpopulations, such as functional movement disorders (FMD) or functional weakness.
In this prospective cohort study, we used a within-group design to investigate relationships between attachment styles, demographic variables, motor subtypes, and other neuropsychiatric factors, including self-reported symptom severity, adverse life event burden, affective symptoms, resilience, and personality dimensions in 56 patients with motor FND. We hypothesized that insecure attachment styles would relate to functional neurological symptom severity and several predisposing vulnerabilities for the development of FND including trauma burden, affective symptoms, maladaptive personality traits, and impaired stress coping.
Methods
Fifty-six patients with motor FND (mean age=40.2 years [SD=13.0]; women, N=41; men, N=15; illness duration=3.3 years [SD=3.7]) were recruited from the Massachusetts General Hospital FND Clinic.
14,16 Patients met criteria for clinically established functional movement disorders (N=29), psychogenic nonepileptic seizures (documented cases, N=21; clinically established cases, N=1; probable cases, N=2), or functional limb weakness (positive examination findings, N=20; probable paroxysmal functional weakness based on history and longitudinal follow-up, N=1). Seventeen of the 56 patients had mixed-motor FND, 16 also showed functional speech symptoms, and 12 exhibited splitting-of-the-midline sensory deficits (for further details, see Table S1 in the
online supplement). Patients with major neurologic comorbidities (N=7) or comorbid epileptic seizures (N=4) were also included. Exclusion criteria included illiteracy, history of mania or psychosis, active suicidality, and current illicit drug abuse or alcohol dependence. The study subjects provided written informed consent as approved by the institutional review board of Partners HealthCare.
All study subjects completed the Relationship Scales Questionnaire (RSQ)
5 as the primary study measure. In addition, self-report measures characterizing functional neurologic symptom severity and the spectrum of common predisposing vulnerabilities and perpetuating factors were also obtained: Patient Health Questionnaire-15 (PHQ-15),
17 Screening for Somatoform Symptoms Conversion Disorder Subscale (SOMS:CD),
18 Dissociative Experiences Scale (DES),
19 Somatoform Dissociation Questionnaire-20 (SDQ-20),
20 Short Form Health Survey (SF-36),
21 Beck Depression Inventory-II (BDI),
22 Spielberger State-Trait Anxiety Inventory (STAI-T),
23 NEO Five-Factor Inventory-3 (NEO),
24 Toronto Alexithymia Scale (TAS),
25 Barrett Impulsivity Scale (BIS),
26 Connor-Davidson Resilience Scale (CD-RISC),
27 Childhood Trauma Questionnaire (CTQ),
28 Life Events Checklist-5 (LEC),
29 and Posttraumatic Stress Disorder (PTSD) Checklist-5 (PTSD-CL5).
30 All individuals also underwent a Structured Clinical Interview for DSM-IV-TR Axis I Disorders.
The RSQ is a 30-item continuous measure of attachment with four established dimensions: secure, fearful, dismissing, and preoccupied.
5 The PHQ-15 and the SOMS:CD denote functional neurological symptom severity. The DES and SDQ-20 are measures of psychological and somatoform dissociation, respectively. The SF-36 assesses mental and physical health status. The STAI-T, BDI, and PTSD-CL5 scales record state-trait anxiety, depression, and PTSD symptom severity, respectively. The TAS evaluates alexithymia, and the NEO assesses five validated personality dimensions. To measure childhood/adolescent and lifetime trauma burden, the CTQ and LEC-5 “happened to me” indices were used. Lastly, the CD-RISC and BIS evaluate resilience and impulsivity, respectively.
Dependent variables included RSQ subscores for secure, fearful, dismissing, and preoccupied attachment styles. Pearson correlations for continuous variables and independent sample two-tailed t tests for dichotomous variables were performed for univariate screenings. Clinical and psychometric variables that showed a statistically significant relationship with any of the RSQ subscores (p<0.05) were entered into separate multivariate linear regression analyses. For any regression model demonstrating collinearity (tolerance<0.20), automated stepwise linear regression was performed. All analyses were performed in IBM SPSSv23 (Chicago).
Results
In univariate tests, secure attachment positively correlated with NEO-extraversion (r=0.47, p<0.001), SF-36 mental health (r=0.30, p=0.03), FMD subtype (t=2.27, p=0.03) and CD-RISC scores (r=0.47, p<0.001); secure attachment negatively correlated with NEO-neuroticism (r=−0.44, p=0.001), TAS (r=−0.47, p<0.001), STAI-T (r=−0.42, p=0.001), and PTSD-CL5 (r=−0.30, p=0.03) scores (for further details, see Table S2 in the online supplement). In a multivariate linear regression analysis, there were no statistically significant variables independently associated with secure attachment.
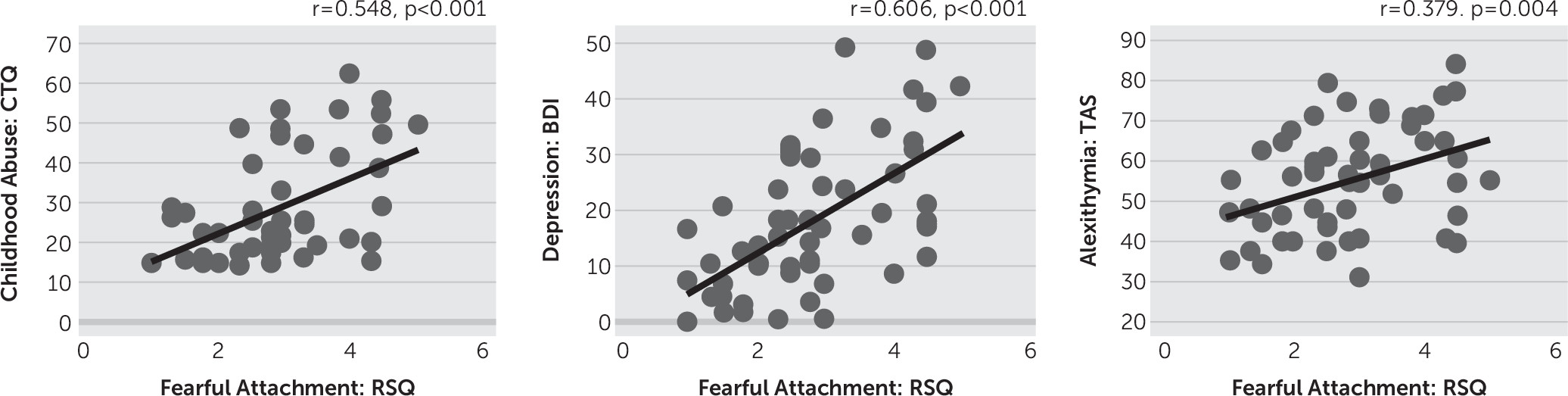
Fearful attachment positively correlated with PHQ-15 (r=0.35, p=0.009), SDQ-20 (r=0.43, p=0.001), DES (r=0.57, p<0.001), LEC ‘happened to me’ (r=0.37, p=0.005), CTQ-abuse (r=0.55, p<0.001), CTQ-neglect (r=0.34, p=0.01), TAS (r=0.38, p=0.004), BDI (r=0.61, p<0.001), STAI-T (r=0.56, p<0.001), PTSD-CL5 (r=0.49, p<0.001), PCS (r=0.51, p<0.001), and NEO-neuroticism (r=0.48, p<0.001) scores. Additionally, fearful attachment negatively correlated with being married (t=−2.09, p=0.04), NEO-extraversion (r=−0.40, p=0.003), CD-RISC (r=−0.30, p=0.03), and SF-36 mental health (r=−0.48, p<0.001) scores. Collinearity testing, as measured by tolerance scores less than 0.20, showed that STAI-T was collinear with several psychometric variables. Therefore, we performed an automated stepwise linear regression using all statistically significant univariate variables, which identified CTQ-abuse (standardized beta=0.39, p<0.001), BDI (standardized beta=0.39, p<0.001), TAS (standardized beta=0.22, p=0.03), and not being married (standardized beta=−0.25, p=0.009) to be significantly associated with fearful attachment (
Table 1) (
Figure 1). This model explained 60.9% of the variance in fearful attachment style scores.
Given the robust relationship between fearful attachment style and childhood abuse burden, we performed a post hoc analysis to evaluate the relationships between fearful attachment and CTQ-abuse subscales (sexual, emotional, and physical). Performing a single linear regression with fearful attachment scores as the dependent variable and all three CTQ-abuse subscales as independent variables, the magnitude of sexual abuse (standardized beta=0.29, p=0.03) and emotional abuse (standardized beta=0.49, p=0.002) independently correlated with fearful attachment. This model explained 37.0% of the variance in fearful attachment style scores.
In univariate tests, preoccupied attachment positively correlated with DES (r=0.38, p=0.004), NEO-neuroticism (r=0.34, p=0.01), STAI-T (r=0.28, p=0.04), BIS (r=0.28, p=0.04), and PCS (r=0.32, p=0.02) scores; preoccupied attachment was negatively associated with NEO-conscientiousness (r=−0.32, p=0.02). In a multivariate linear regression analysis, no variables independently correlated with preoccupied attachment.
Dismissing attachment was negatively associated with being married (t=−2.41, p=0.02) and white ethnicity (t=−2.13, p=0.04) in univariate analyses. Neither variable remained statistically significant in a multivariate linear regression analysis. Also, across all univariate analyses, there were no statistically significant differences in attachment subscale scores between patients with isolated FND (N=45) and the 11 individuals with FND and comorbid major neurologic conditions.
Discussion
The positive correlation between fearful attachment tendencies and childhood traumatic experiences across motor FND subtypes reinforces the notion that early-life maltreatment is connected to insecure attachment in adulthood. While not all individuals with FND endorse adverse early life events, childhood trauma is a well-documented risk factor for FND
31 and has been linked to functional neurologic symptom severity.
32–34 Our findings extend prior evidence of relationships between fearful attachment and early traumatic experiences in PNES,
12 demonstrating overlapping trauma-attachment relationships across the spectrum of motor FND. Studies have also observed higher incidence of insecure attachment and childhood trauma in patients with somatic symptom disorders.
35 Our post hoc analyses demonstrate that sexual and emotional abuse each independently contribute to the development of fearful attachment in patients with motor FND. As noted by Wearden and colleagues, fearful attachment, which combines a negative view of the self with a negative view of others, can arise from past rejection or caregiver maltreatment, resulting in abandonment anxiety and a fear of intimacy in interpersonal relationships.
9 This phenomenon may explain why patients with FND who were married reported lower fearful attachment tendencies, though this study only examined marital status, as opposed to marital quality or relationship stability, which may be potential topics for future research.
In patients with FND, fearful attachment also positively correlated with alexithymia and depression, factors that we have previously linked to decreased self-reported resilience in a recently published study from our lab in this same cohort.
14 Alexithymia, or difficulty identifying and expressing emotions, has been associated with insecure attachment in patients with somatic symptom disorders and constitutes an obstacle to healthy emotional and personal interactions.
36 Alexithymia is commonly identified as an important predisposing vulnerability in patients with FND
10,37,38 and may partially explain the misattribution of emotional states as physical phenomena given nuanced connections between stressful life events, affective dysregulation, and physical symptoms. This explanation may be in line with alexithymia-related somatosensory amplification, which attributes increased interoceptive arousal and somatic misattribution to alexithymic patients.
39 Additionally, depression is a common comorbidity in FND,
16,40,41 and links between depression, health-related quality of life and prognosis have been well described in FND populations.
42,43 In the context of recognized associations between fearful attachment and depression,
44 PTSD
45 and dissociation,
46 our finding suggests that links between negative affective symptoms and fearful attachment are present across multiple psychopathologies.
Across attachment styles, personality traits, resilience, and anxiety appear to also be important factors connected to patients’ approaches to interpersonal relationships based on our preliminary univariate analyses. We have previously linked adaptive and maladaptive personality traits to self-reported stress coping (resilience) in patients with FND,
14 and personality traits may influence concurrent pathophysiology, symptom profiles, and prognosis in FND populations.
43,47 Furthermore, self-reported resilience was closely linked to secure attachment and inversely associated with fearful attachment in univariate analyses, suggesting that healthy interpersonal relationships are an important component of adaptive stress coping. In this study, secure, fearful, and preoccupied attachment styles related to neuroticism, a factor that plays a role in the development of mood and affective disorders more broadly.
48 Additionally, anxiety, another common comorbidity in FND,
16,40,41 positively correlated with fearful and preoccupied attachment styles and negatively correlated with secure attachment. The lack of clear connections related to symptom severity and health status indicate that further studies of attachment with larger sample sizes are needed to investigate potential indirect links between attachment styles and symptom severity.
While this study aimed to examine relationships between attachment styles and other neuropsychiatric factors in FND, we did not obtain attachment data in healthy controls or other clinical populations, preventing analyses of group-level differences. We were also limited by a reliance on self-report measures and did not use gold standard structured attachment interviews,
13 leaving unaddressed potential differences between self-perceived interpersonal styles and more objective measures. Additionally, we included 11 FND patients with major neurological comorbidities to ensure that the study sample was representative of the overall FND population.
14 Lastly, we recruited patients across the motor spectrum of FND, given the many similarities among these subpopulations,
14,32 although this approach remains open to debate.
49 We observed only one univariate association between a motor FND subtype and an attachment style (individuals with FMD reported higher secure attachment tendencies compared with other motor FND subtypes), implying that insecure attachment styles were similar across motor FND subpopulations.
In conclusion, fearful attachment related to the magnitude of childhood abuse burden, alexithymia, depression, and marital status in patients across the spectrum of motor FND. These findings identify links between fearful attachment tendencies and several other risk factors for the development of FND. Future research is needed to determine the influence of insecure attachment styles on symptom onset and severity as well as clinical outcomes in FND.