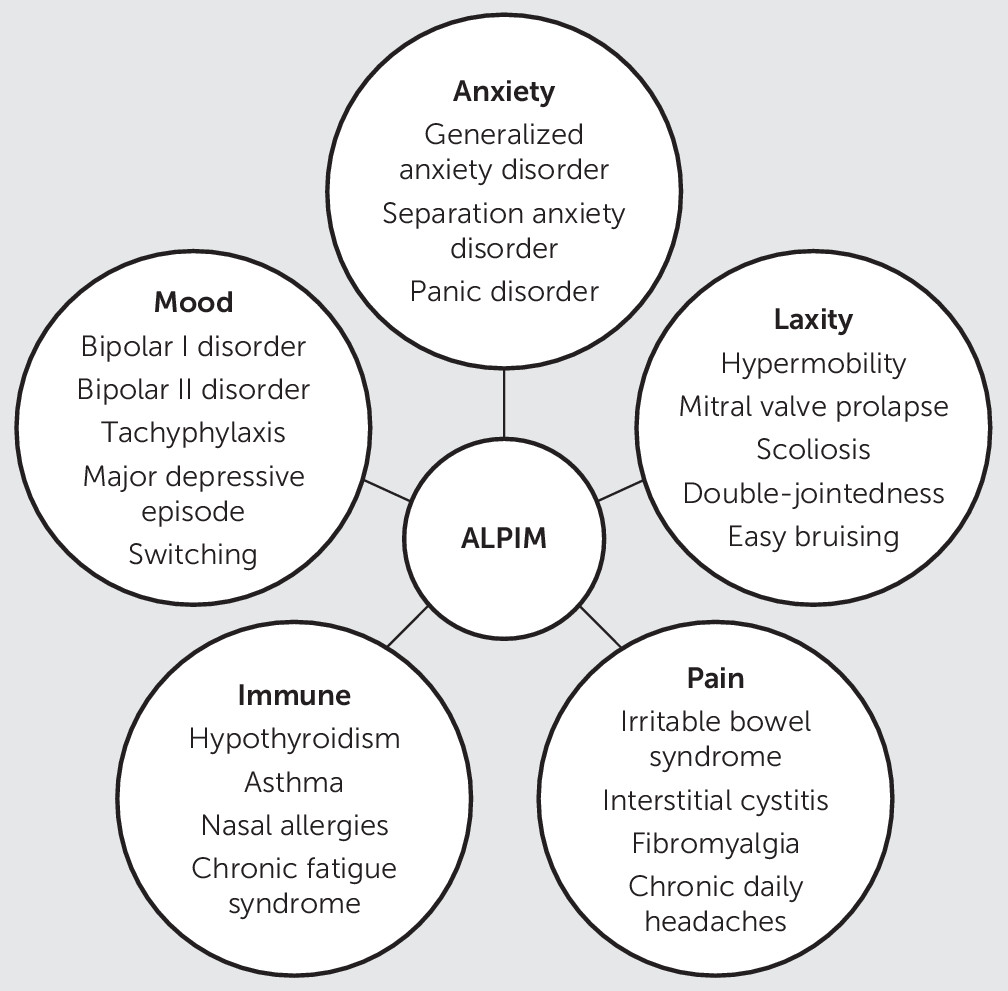
The ALPIM (anxiety, laxity, pain, immune, and mood) syndrome has been previously described by our group as an anxiety spectrum disorder that incorporates distinct and replicable medical comorbidities (
1). It has been proposed to have a core anxiety disorder with clusters of comorbid disorders within each of the following domains: joint laxity, chronic pain, autoimmune conditions, and mood disorders. The original description of the ALPIM syndrome included generalized anxiety disorder (GAD), social anxiety disorder, and panic disorder within the anxiety domain; joint laxity, easy bruising, scoliosis, and mitral valve prolapse (MVP) in the laxity domain; irritable bowel syndrome (IBS), interstitial cystitis (IC), and chronic daily headaches in the pain domain; chronic fatigue syndrome (CFS), asthma, rhinitis and sinusitis, and hypothyroidism in the immune domain; and major depressive episode, bipolar II disorder, switching, and tachyphylaxis in the mood domain. Switching was defined as hypomania or mania resulting from the use of antidepressant medications and tachyphylaxis, a reduction in the efficacy of antidepressant treatment following an initial response. The ALPIM syndrome was presented as a spectrum disorder, meaning not all individuals with the condition would show each of the associated comorbidities (
Figure 1).
Associations between many of the conditions overlapping with the ALPIM syndrome have previously been described by other research groups. Affective spectrum disorder demonstrated a significant co-occurrence of multiple psychiatric diagnoses (major depressive disorder, attention deficit hyperactivity disorder, bulimia nervosa, premenstrual dysphoric disorder, dysthymic disorder, GAD, obsessive-compulsive disorder, panic disorder, posttraumatic stress disorder, and social phobia) with four medical conditions: fibromyalgia, IBS, migraine, and cataplexy (
2). Joint hypermobility syndrome (JHS), an inherited connective tissue disorder that consists of joint laxity, easy bruising, scoliosis, fibromyalgia, and double-jointedness, has been shown to be related to anxiety disorders.
It is noteworthy that the terms “joint laxity,” “joint hypermobility syndrome,” and “Ehlers-Danlos syndrome, type III (hypermobility subtype)” are used interchangeably in the literature (
3,
4). Panic disorder syndrome is another mind-body association, linking panic disorder to bladder problems, severe headaches, MVP, and thyroid conditions (
5). Bladder pain syndrome, also known as IC, was shown to have significant associations with IBS, CFS, fibromyalgia, migraine, depression, and allergies (
6,
7).
The ALPIM syndrome differentiated itself from other spectrum syndromes by demonstrating an association not only between ligamentous laxity and panic disorder (
3) but also a broader comorbidity with other anxiety disorders, chronic pain disorders, immune disturbances, and mood disturbances, including bipolar disorder. No studies have been conducted to confirm the findings from the initial report on the ALPIM syndrome. Additionally, the presence of ALPIM syndrome among adolescents has not been explored previously.
A review of the literature revealed a plethora of research showing a link between the aforementioned ALPIM comorbidities in the child and adolescent population. Although most studies describe psychiatric comorbidity with JHS in adults (
3,
4,
8,
9), JHS has also been found to be linked with anxiety and depression among adolescents (
10,
11). Relationships across ALPIM comorbidities with JHS are seen in children—with MVP (
11), easy bruising (
9), fibromyalgia (
12), IBS (
13), urinary tract dysfunction (
14), and CFS (
15). In addition, two-thirds of adolescents with MVP show signs of anxiety disorders (
16). CFS and other comorbidities such as fibromyalgia, IBS, asthma, and IC have been described as functional somatic syndromes (
17,
18). Not only have functional somatic syndromes been described in adolescents, they have also shown an association between anxiety and headaches (
19). Chronic daily headaches are recognized in children and adolescents and often lead to a considerable effect on the quality of life, daily activities, social interactions, and school performance in combination with psychiatric symptoms (
20). Additionally, children and adolescents presenting with headaches report more internalizing symptoms (anxiety and depression) (
21). Mood and anxiety disorders are commonly comorbid with thyroid abnormalities (
22). There is a significant association of early childhood allergic rhinitis and allergic persistent wheezing with anxiety and depression (
23). Additionally, a recent meta-analysis demonstrated that youths with asthma have more than three times the prevalence rate of anxiety disorders when compared with healthy youths (
24). IC affects approximately 4–12 million people worldwide and can occur at any age, including during childhood, but is most commonly reported in adult women (
25).
The prevalence rate of any anxiety disorder as per the National Comorbidity Study-Adolescent Supplement (2010) among adolescents is 31.9% (
26). Because
DSM-IV-TR (
27) was in use when the initial ALPIM report was conducted, adult-onset separation anxiety disorder (SAD) was not included as part of the study as a result of its lack of recognition in the adult population. However,
DSM-5 emphasizes that it is not necessary to have a past childhood history of SAD to diagnose during adulthood (
28). This new position is based on findings of epidemiological studies revealing the high prevalence of the condition among adults, often in individuals with an onset of symptoms after adolescence (
29) According to the
DSM-5, SAD is excessive anxiety concerning separation from home or attachment figures. It is noteworthy that the
DSM-5 acknowledges that individuals with SAD present with repeated complaints of physical symptoms like headache or nausea (
28). SAD is the most frequently diagnosed childhood anxiety disorder, accounting for approximately 50% of referrals for mental health treatment of anxiety disorders (
30). Adults with SAD have strong fears that their attachments figures will be harmed, generating strenuous efforts to remain in close contact with them despite troublesome impracticalities (
31).
The literature is sparse on the co-occurrence of ALPIM comorbidities with SAD. One study found SAD to be the most common anxiety disorder experienced by young adults with CFS (
32) A study done in Puerto Rican children between 4 and 17 years old found that children with a history of asthma attacks had higher prevalence rates of any depressive disorder or anxiety disorder, including SAD, when compared with children who had no history of asthma attacks (
33).
Given the above background, this study was designed to identify the occurrence of ALPIM syndrome among adolescents. In addition, by including young adults, this study attempted to establish a trajectory of the disease process in patients with ALPIM by analyzing differences in the clinical presentation between adolescents and adults. In order to further establish the diagnostic distinction of ALPIM syndrome as an anxiety-predominant phenomenon, a comparator group with major depressive disorder as the primary inclusion condition was assessed. Additionally, in an effort to enhance diagnostic specificity as compared with the initial study, only patients with comorbidities from each of the ALPIM domains were to be diagnosed as having ALPIM syndrome. Finally, given the recent recognition of SAD as a lifelong illness with evidence of somatic presentation, it was explored as a possible comorbidity within the ALPIM syndrome.
Methods
A retrospective chart review of all adolescents and young adults (ages 11 to 34) seen consecutively was conducted from general hospital consults and outpatient psychiatry visits during a contiguous year-long period. In all, 1,148 patient charts were reviewed. The medical records, including surgical, medical-pediatric, and psychiatric documentation of these patients, were reviewed. Of note, the psychiatric assessments documented in these charts were conducted by board certified psychiatrists familiar with the ALPIM syndrome. Patients diagnosed with a documented history of anxiety (anxiety cohort: GAD, social anxiety disorder, SAD, and panic attacks) or major depressive disorder were included. A lifetime rather than point prevalence of these conditions in the individual patients was considered for inclusion.
Patients were excluded from this study if age was less than 11 or more than 34 years old. The ages 11–34 years were chosen to include the generally accepted adolescent and young adult age groups. Patients with a diagnosis of autism spectrum disorder, Prader-Willi syndrome, and intellectual disability were excluded due to lack of reliable caregiver and self-report on physical symptoms. Patients with eating disorders or active substance use were excluded. Patients with established diagnoses of autoimmune inflammatory gastrointestinal conditions (i.e., inflammatory bowel diseases) were excluded due to symptomatic overlap with IBS. Established autoimmune arthritic conditions such as rheumatoid arthritis were also excluded due to restricted range of motion and difficulty obtaining a reliable joint exam. Finally, as a result of the prominent unique anxiety symptoms prevalent in posttraumatic stress disorder, patients with this diagnosis were not included in the study.
Out of the 1,148 patients with chart-reviewed data, 854 were excluded because they did not meet the age criteria and 109 were excluded due to the aforementioned exclusionary diagnoses. A total of 185 patients fulfilled the inclusion criteria. The charts were then further reviewed for the presence of ALPIM comorbidities. For the purposes of this study and analysis, ALPIM was considered present in a study subject only if he or she had one or more diagnoses from each of the four medical ALPIM domains (laxity, pain, immune, and mood). The ALPIM Inventory, Version 2, was used as the data collection tool during chart review. All individual conditions included within the ALPIM Inventory—such as JHS, double-jointedness, easy bruising, and MVP from the laxity domain; IBS, IC, fibromyalgia, and chronic daily headache from the pain domain; hypothyroidism, asthma, nasal allergies, and CFS from the immune domain; and bipolar disorder I and II, switching, tachyphylaxis, and major depressive episode from the mood domain—were considered positive if they were clearly documented as diagnoses in the reviewed charts. Documentation of a lifetime prevalence of the comorbidities in the individual patients was considered positive. It is noteworthy that a documented diagnosis of migraine headaches was considered positive for chronic daily headaches. Although hernia was assessed for in the previous ALPIM publication, given the heterogeneity in types of hernias (visceral, vertebral, etc.), the authors had not included it in their final tabulation of prevalence. The present study has excluded hernias for the same reasons from the ALPIM Inventory. To ensure reliability, joint hypermobility was considered positive only if the documentation stated a diagnosis based on using the Beighton scale (
34) or diagnosis by a rheumatological or orthopedic specialist.
This study was given exempt status from the institutional review board after appropriate application, given its retrospective methodology and lack of use of any identifying information.
Data Analysis
All analyses were done using SAS 9.4. p values<0.05 (two-tailed) were considered to be significant. Age was presented using mean and standard deviation. Gender was summarized using frequency and percentage. Statistical comparisons between groups were done using a two-sample t test and Fisher’s exact test. Binary logistic regression was used to find predictors of ALPIM syndrome.
Results
Overall, 185 patient charts were retrospectively enrolled in this study. Patients had a mean age of 17.5 years (SD=5.5), and 123 (66%) were female. Of these patients, 146 had one or more anxiety disorders (the anxiety cohort) and 39 patients had major depressive disorder without a primary anxiety disorder diagnosis (major depressive disorder cohort). In the anxiety cohort, 20 cases (10.8%) met criteria for having ALPIM syndrome with a 95% confidence interval (CI)=0.06–0.15. Patients in the major depressive disorder cohort were significantly younger than patients in the anxiety cohort (mean age, 15.8 years [SD=4.9] compared with 17.9 years [SD=5.6]). However, there was no gender difference between the two cohorts. The proportions of patients with joint hypermobility, double-jointedness, IBS, asthma, allergic sinusitis/rhinitis/pharyngitis, and chronic daily headaches were all significantly higher in the anxiety cohort as compared with the major depressive disorder cohort. An overall domain analysis showed that comorbidities from laxity, pain, and immune domains were significantly more prevalent in the anxiety cohort (
Table 1).
With age group categorized as younger than 18 years old versus 18 years of age or older, there were no differences in rates among any of the individual ALPIM-related comorbidities (
Table 2).
Multivariable model for prediction for the presence of ALPIM indicates that separation anxiety and GAD were independently associated with ALPIM. Our adjusted model includes patients’ demographics (age and gender) and significant anxiety subdomains (separation anxiety and GAD). After adjustment, patients with separation anxiety had increased odds of being diagnosed with ALPIM (odds ratio [OR]=7.14, 95% CI=2.48–20.54, p<0.001), whereas patients with GAD had decreased odds of being diagnosed with ALPIM (OR=0.43, 95% CI=0.12–0.94, p=0.037). No other variables were associated with ALPIM (
Table 3).
Discussion
The ALPIM syndrome has previously been described as a novel anxiety spectrum disorder that unites several seemingly unrelated physical conditions into one overlapping syndrome. Although this syndrome was described in adults as a case series, its existence in adolescents had not been examined (
1).
This study reestablished the syndromal association between the ALPIM comorbidities. Anxiety was again highlighted as the core domain; the occurrence of joint hypermobility, double-jointedness, IBS, asthma, allergic sinusitis/rhinitis/pharyngitis, and chronic daily headaches were all significantly higher in the anxiety cohort as compared with the major depressive disorder cohort of included patients. Our findings demonstrate that the ALPIM syndrome exists in adolescents and the likelihood of its presence appears independent of age. Finally, a diagnosis of separation anxiety significantly increased odds of meeting criteria for the ALPIM syndrome. No other individual disorder showed a similar predictive effect in this study.
Our findings may have important implications, as many of the included comorbidities such as IBS, migraines, and fibromyalgia lead to significant long-term distress and treatment costs (
35). An important replication of previous findings is the link of anxiety disorders with multiple medical conditions such as joint laxity, IBS, chronic daily headaches, asthma, and allergic rhino-sinusitis. It is noteworthy that MVP was not significantly associated with ALPIM syndrome in this study. This lack of association may be a result of more stringent diagnostic criteria required for clinically significant MVP than previously was the case, hence lowering the rates of its diagnosis (
36). Additionally, hypothyroidism was not significantly correlated with ALPIM syndrome. This could be due to the generally younger age of the adolescent and young adult subjects, thus possibly missing a later onset of hypothyroidism. ALPIM syndrome in the present study was more prevalent in women than in men. This may be a result of the higher prevalence of any anxiety disorder in women as compared with men (
37).
In this study, to be diagnosed as having ALPIM syndrome the patients had to present with one or more diagnoses from each of the ALPIM domains. Using major depressive disorder to define a separate cohort helped access a distinctive phenotype that was dissimilar from having a major depressive episode as part of the mood domain in the ALPIM syndrome. Of note, although the anxiety cohort displayed comorbid ALPIM features at statistically significant levels, this was not the case for the major depressive disorder group. The results of our analysis suggest that having major depression did not predict the presence of ALPIM syndrome, and a subject meeting criteria for the ALPIM syndrome was not more likely to have a mood disorder than those without ALPIM. Thus, to define ALPIM syndrome as a clinical diagnosis, the authors recommend that clinicians should diagnose the syndrome even in the absence of a mood component. This may increase the sensitivity and early detection of this syndrome. Further studies are recommended to clarify reliable diagnostic criteria for ALPIM syndrome.
Perhaps most significant was the finding that separation anxiety differentiated itself from other anxiety disorders as a predictor of ALPIM syndrome. This study found that patients with SAD were more than seven times more likely to have ALPIM syndrome, whereas other anxiety disorders did not correlate with increased odds of having ALPIM syndrome. In fact, GAD was negatively correlated with meeting criteria for ALPIM. Thus, separation anxiety should be explored in adolescents as well as adults presenting with ALPIM-related physical conditions. These findings suggest that the ALPIM syndrome stands out as a distinct pathologic condition and identifies separation anxiety at its core, whether in adolescence or young adulthood.
This study has several limitations. The retrospective nature of the chart review makes it difficult to associate specific illnesses to the ALPIM syndrome; despite every effort made by the authors to exclude any incomplete or inconsistent documentation, the documented clinical diagnoses in the chart may have inaccuracies. This also made it very difficult to associate specific illnesses such as anxiety disorder to the symptoms of ALPIM. The psychiatric documentation review was done by psychiatrists familiar with the ALPIM syndrome who knew to look for seemingly unrelated medical comorbidities that might not otherwise have been explored by mental health providers without prior knowledge of the syndrome. Although an interdiagnostic grouping between anxiety disorders was analyzed and showed SAD as an independent predictor, a prospective study of patients with and without SAD may be required to further establish the correlation and potential causation. Given the stringent diagnostic criteria used for this study, the hypothesis of ALPIM being a spectrum disorder could not be tested. Future studies may explore the determination of severity or the possibility of partial ALPIM syndrome presentations.
An important limitation of this study was the absence of genetic analysis. The comorbidity of Ehlers-Danlos syndrome, especially type III (hypermobility subtype), and anxiety has been reported (
4), and it is possible that a subset of patients diagnosed with ALPIM have this genetic disorder. Future studies should test the genetic makeup of ALPIM patients to determine this and other potential genetic correlates. Finally, although tachyphylaxis was noted to be more prevalent in the ALPIM patients, bipolar disorder and switching with psychotropic medications were not significantly present in our study population. This may be a result of the delay in diagnosis of bipolar disorder (
38) and the lack of long-term exploration in our study. It is also possible that bipolar disorder was not diagnosed as frequently as in the first ALPIM study (
1) as a result of changes in the
DSM-5 that led to the inclusion of mixed features in major depressive disorder (
29). Additionally, the first ALPIM study involved a semistructured interview format as opposed to the retrospective chart review of the present study, which possibly contributed to greater recognition of bipolar disorders in the first study.
It is important to examine the possible etiological mechanisms of the ALPIM syndrome. The authors note that among the included diagnoses in ALPIM, most have an established monoamine hypothesis: disturbance in monoamine derivatives (serotonin, norepinephrine, and dopamine) has been implicated in anxiety, MVP, headaches (migraines), fibromyalgia (
39), IBS, IC, CFS, and mood disorders (
40). Thus, exploring the monoamine system as the underlying cause may be a potential starting point in determining etiopathogenesis. That, in turn, would also shed light on evidence-based treatments.
A self-report bias in patients with anxiety has long been a clinical concern (
41). Patients with anxiety presenting with physical complaints have often been dismissed as simply somatizing (
42). This bias was addressed in the present study, as the ALPIM group clearly differentiated itself from the larger group of subjects presenting with anxiety. This study highlights the importance of clinicians working collaboratively to avoid silos of specialties. It emphasizes that instead of being dismissive of patients presenting with seemingly unrelated symptoms, a collaborative review while keeping in mind the existence of multisystem conditions such as the ALPIM syndrome is needed.
Conclusions
The ALPIM syndrome has a heterogeneous presentation with anxiety at its core. In this retrospective chart review, the ALPIM syndrome was demonstrated in adolescents and adults in similar frequencies. Separation anxiety was determined to be an independent predictor of the ALPIM syndrome, differentiating itself from generalized anxiety, social anxiety, and panic attacks. Furthermore, mood disorders including depression were not noted to be a predictor of ALPIM. The results from this study suggest that the ALPIM syndrome is a distinct clinical entity that is diagnosable during adolescence and often presents with separation anxiety comorbid with distinct physical complaints within the laxity, pain, and immune domains. Future studies should explore etiology, diagnostic refinement, and treatment strategies for this condition.
Acknowledgments
Dr. Coplan has served on the speaker’s bureau for Allergan, Neurocrine, Otsuka-Lundbeck, and Sunovion; he has received research grant support from Corcept and Neurocrine; and he has served on the advisory board of Otsuka-Lundbeck. The other authors report no financial relationships with commercial interests.