Worldwide, stroke is the third most common cause of disability.
10 Although the mortality rate and incidence of stroke has decreased in much of the world, the overall stroke burden has increased.
11,12 Most worrisome, the rates of stroke in younger adults (20–64 years of age) may actually be increasing.
10 Stroke-related disability burden is considerable due to long-term physical, cognitive, and psychological sequelae. Development of depression is one of the more common sequelae and is associated with multiple detrimental outcomes, making both prevention and prompt identification and treatment high priorities.
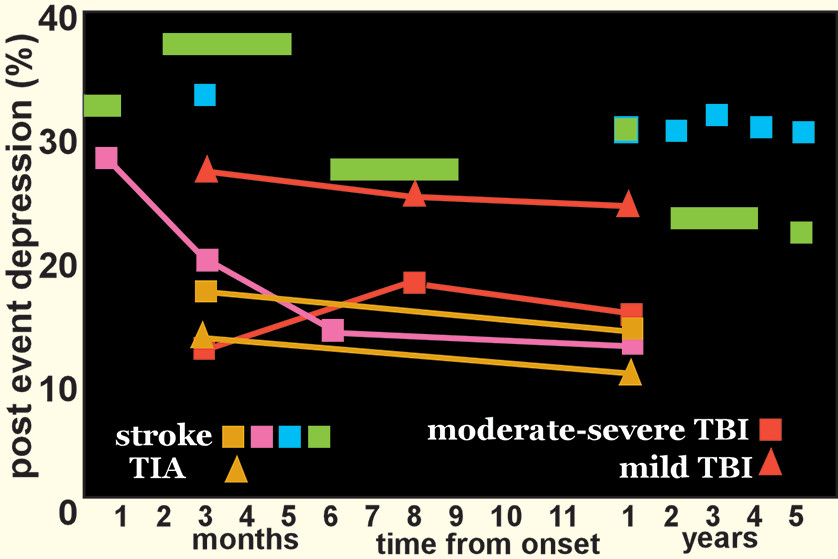
13,14A recent meta-analysis found that within the initial 5 years after a stroke, 31% of patients developed poststroke depression (PSD) (
Figure 1).
2 A similar prevalence (34%) of PSD was reported in a recent study at 2–5 years poststroke.
15 A longitudinal study found that one-third of cases of PSD developed within the first 3 months after stroke, and half of these remitted by 1 year.
1 A similar pattern was reported in a study of first-ever ischemic strokes (mostly mild) (
Figure 1).
3 It is noteworthy that two studies using data from stroke registries that included patients with transient ischemic attacks (TIAs) reported similar rates of depression following stroke and TIA (
Figure 1).
4,16 Relatively similar rates were also reported in a study limited to patients that were younger (18–50 years of age) at onset.
17 Overall, these studies indicate that severity of brain injury is not a primary pathophysiological mechanism for PSD. This parallels what has been reported on development of major depression (MDD) after traumatic brain injury (
Figure 1).
5,18 In addition to psychological morbidity, PSD is also independently associated with more detrimental functional outcomes.
13,19There is considerable debate regarding the effect of lesion location on risk of PSD. Two meta-analyses failed to find support for a relationship between lesion location and PSD.
20,21 Another reported a very weak correlation between right hemisphere lesions and PSD.
22 In contrast, two later meta-analyses reported slightly increased frequency of PSD with left hemisphere lesions, but in one study this was specific to the acute phase and in the other study it was specific to the subacute phase.
23,24 A smaller meta-analysis found an inverse correlation between severity of depression and distance from lesion to the frontal pole, but only for left hemisphere strokes.
25 Common methodological weaknesses identified in these studies include usage of many different instruments for identification of PSD, considerable range in time from event, visual analysis of lesion locations, and the systematic exclusion of patients with language dysfunction.
26Recent studies utilizing more advanced approaches to lesion-symptom mapping (e.g., statistical parametric mapping, multivariate lesion-symptom mapping) have not resolved the debate. In one study, injury to left putamen, right insula and right superior longitudinal fasciculus were associated with presence of major depression (Hamilton Rating Scale for Depression-24 [HAM-D-24] score ≥20) at 1 month.
27 In another, higher symptoms of depression (Hospital Anxiety and Depression Scale) in the acute-subacute stage correlated with injury to brainstem, left basal ganglia, and left ventrolateral prefrontal cortex.
28 In contrast, the study that focused on left hemisphere strokes in the chronic stage reported that greater symptoms of depression (Stoke Aphasic Depression Questionnaire) were associated with injury to left dorsolateral prefrontal cortex.
29 A fourth study reported that no areas were significantly associated with a diagnosis of PSD once correction for multiple comparisons was done.
30 Other recent studies have also reported a lack of association between either stroke location or volume and presence of PSD, indicating the importance of other factors.
6,8,31 As with other areas of PSD study, this remains an active area of inquiry.
Although there may not be a definitive relationship between lesion location and PSD, another growing area of research is alterations to non-lesion anatomical locations and alterations of connectivity networks outside of the discrete lesion. Recent studies have focused upon understanding the role of altered networks, determined by either structural or functional connectivity, especially in the setting of recovery from loss of brain parenchyma, as in stroke.
32–35 Alteration of the most richly connected areas (“hubs”) of the connectome have been implicated in numerous brain disorders, including stroke.
36–38 Structural (anatomic) connectivity is commonly assessed using diffusion tensor imaging (DTI) tractography based metrics that estimate strength of physical connections between areas (nodes).
39,40 Functional connectivity is commonly assessed using resting-state functional MRI (rs fMRI) metrics that are based on temporal correlation of spontaneous signal intensity changes within two areas (e.g., voxel, region of interest).
32,39–41 Network structure is most altered in the acute to subacute period following stroke.
33,34 Normalization of network structure has been shown to parallel recovery in the domains of language, memory and attention.
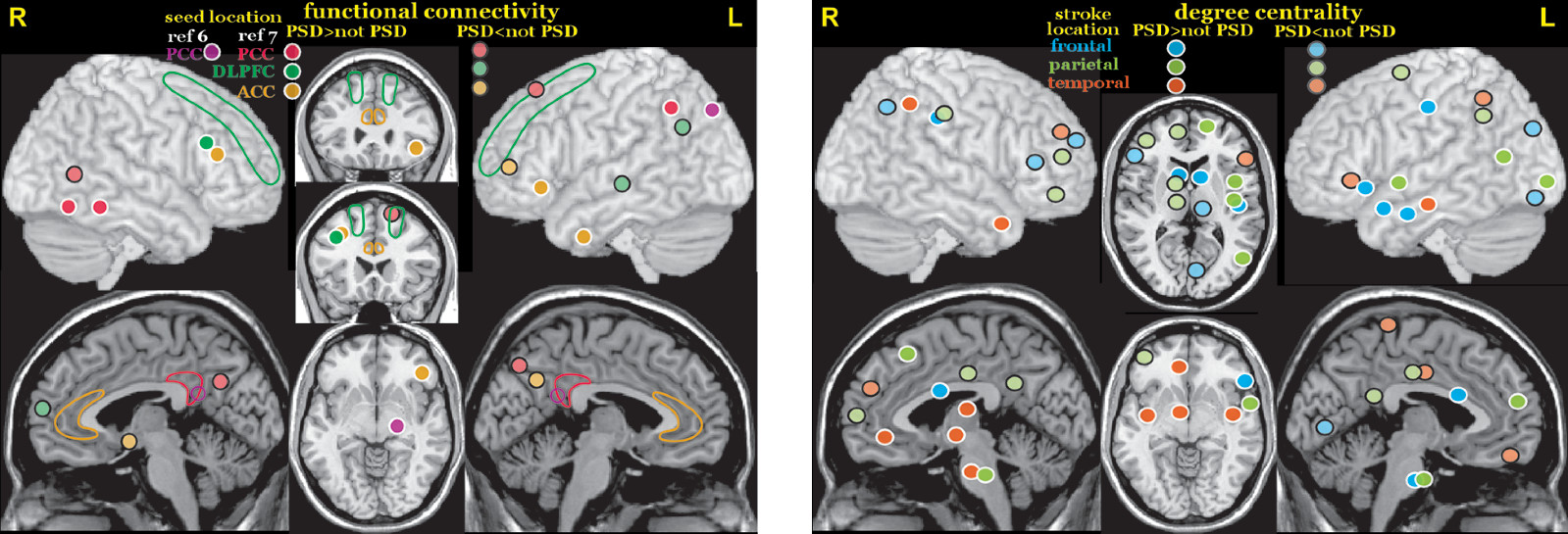
34Studies comparing connectivity metrics between stroke patients with and without PSD are considered the most useful for identifying symptom-related network changes.
42 A rs fMRI study that utilized bilateral seeds (posterior cingulate/retrosplenial, anterior cingulate and dorsolateral prefrontal cortices) to assess functional connectivity in three networks (chosen because they have been implicated in MDD) in the early subacute (<2 weeks) period reported multiple areas in which stroke patients with and without PSD differed (
Figure 2).
7 Another rs fMRI study in the subacute (<1 month) stage also reported higher functional connectivity between posterior cingulate/retrosplenial cortex and inferior parietal cortex in stroke patients with PSD compared with stroke patients without PSD (
Figure 2).
6 A rs fMRI study in the early chronic (3 months) stage that utilized the amplitude of low frequency fluctuations (ALFF) to assess regional activity level reported higher fractional ALFF (fALFF) in the left dorsolateral prefrontal cortex and right precentral gyrus in patients with PSD compared with patients without PSD.
31 One source of variance in these studies is that their groups encompassed all stroke locations. The other chronic stage (3–12 months) rs fMRI study compared patients with and without PSD grouped by stroke location (frontal, parietal, temporal).
8 This study assessed whole brain functional connectivity at the voxel level (degree centrality, number of connections). Of note, stroke location affected where differences in degree centrality between patients with and without PSD were located and in some instances the direction of differences (
Figure 2).
8A few studies have assessed relationships between connectivity metrics and severity of depression symptoms. A DTI study compared structural connectivity (node degree) of 90 nodes (regions of interest) derived by using the automated anatomic labeling (AAL) atlas to parcellate the brain.
27 Lower connectivity at one week correlated with higher severity of depression (HAM-D-24) at 1 month for 17 of the nodes (bilateral - superior frontal gyrus, posterior cingulate gyrus, fusiform gyrus, insula, caudate; left: inferior frontal gyrus, superior temporal gryus, olfactory cortex, precuneus; right: precentral gyrus, putamen).
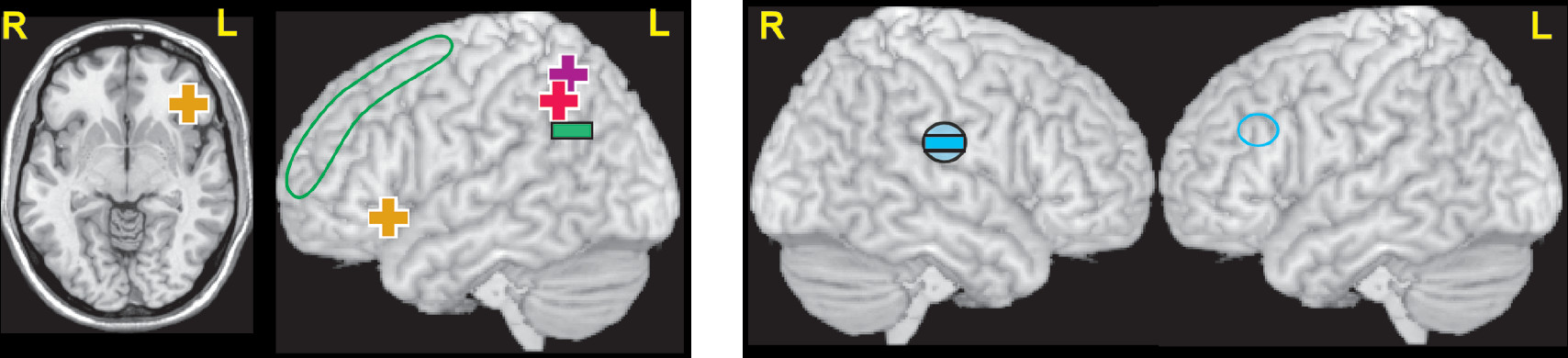
27 Both rs fMRI studies that utilized bilateral seeds reported that severity of depression (HAM-D-17; Beck Depression Inventory, BDI) in the PSD group was significantly positively correlated with increased functional connectivity between posterior cingulate/retrosplenial cortex (default mode network) and inferior parietal cortex (
Figure 3 and cover).
6,7 The study that assessed other seeds reported that the severity of depression (HAM-D-17) in the PSD group was also positively correlated with increased functional connectivity of the anterior cingulate cortex (affective network) to orbital inferior frontal gyrus, with a trend negative correlation with decreased functional connectivity of dorsolateral prefrontal cortex (cognitive control network) to angular gyrus (
Figure 3 and cover).
7 In a set of rs fMRI studies in the early chronic stage (3 months) after mostly minor strokes, severity of depression symptoms (Patient Health Questionnaire, PHQ-9) correlated with higher fALFF in the left insula/superior temporal gyrus and with lower seed-based functional connectivity of the left dorsolateral prefrontal cortex to right supramarginal gyrus (
Figure 3).
9,31 Another rs fMRI study that evaluated functional connectivity between all voxels and the default mode network (identified by independent component analysis) reported functional connectivity at ten days correlated with symptoms of depression (HAM-D-17) at 3 months (but not at ten days) for three areas.
43 The correlation was positive for middle temporal cortex and precuneus, negative for neostriatum. As noted in many of these studies, these network changes are generally consistent with what has been reported for MDD.
41,44,45Despite the consensus regarding the prevalence and burden of PSD, there is substantial disagreement regarding the pathophysiology. Proposed biological contributors to PSD include alterations in neurotrophic factors, hypothalamic-pituitary-adrenal axis dysfunction, the inflammatory cascade and cell-mediated immune activation that follows stroke.
13,46–48 A study that correlated the proteomic profile with depressive symptoms at 3 months poststroke supported the presence of peripheral immunodepression due to neuroinflammatory processes.
49 The interaction of the inflammatory response with neurotrophic factors has become a promising avenue of study. The most important neurotrophin implicated thus far is brain-derived neurotrophic factor (BDNF), shown as early as 1995 to promote neuronal survival in vitro.
50 Low circulating BDNF levels have been associated with an increased risk of stroke.
51 Low levels of BDNF in the acute stage of stroke have been associated with poor functional outcomes at two-year and seven-year follow ups, independent of stroke severity.
52 A recent meta-analysis found that peripheral BDNF levels in the acute stage were lower in stroke patients who went on to develop PSD, suggesting potential as a biomarker.
53 Although a connection between polymorphisms in BDNF genotype and a propensity for PSD has been reported in some studies, a recent meta-analysis found a relationship to significantly lower risk of ischemic stroke, but no role in PSD.
54 Many of these factors have also been implicated in MDD.
46,55–57 For example, meta-analyses indicate elevations of multiple peripheral biomarkers of inflammation (e.g., cytokines, interleukins, chemokines) in MDD, as well as decreased peripheral levels of some immune mediators following treatment with antidepressants.
58–62 A recent meta-analysis that focused on BDNF found support for a link between polymorphisms in BDNF genotype and risk of late life depression, decreased peripheral levels of BDNF in patients with MDD, and increases in BDNF following treatment with selective serotonin reuptake inhibitors (SSRIs) or electroconvulsive therapy.
63 It is noteworthy serotonin-norepinephrine reuptake inhibitors did not increase BDNF levels.
Although multiple treatment modalities have been studied, there is considerable heterogeneity in key methodological aspects such as time from stroke and duration of treatment. Several meta-analyses of randomized control trials have determined that antidepressants were better than placebo for improving symptoms of depression in patients with PSD, although medications varied considerably in both efficacy and tolerability.
64–67 The potential of antidepressants to prevent development PSD in nondepressed stroke patients is also supported by several meta-analyses.
64,68,69 In addition, there is growing evidence that treatment with SSRIs in particular can improve functional recovery (e.g., dependence, disability, neurological impairment) after stroke, although the meta-analysis did not address whether neurological recovery occurred independently of improvement in depression.
65,70 A recent meta-analysis of randomized control trials in which SSRIs were initiated within the first month in stroke patients without PSD reported improved neurologic functioning (e.g., decreased disability, increased functional independence).
71 Contrary to expectations, SSRIs did not decrease incidence of PSD. Animal studies indicate multiple possible mechanisms of action (e.g., promoting neurogenesis, increasing neurotrophins including BDNF, decreasing inflammation).
70,72Conclusions
Understanding of the prevalence, influence, and pathophysiology of PSD have advanced over the previous two decades. An important advance has been the shift from a primary focus on lesion location to study of brain functional and structural network changes after stroke. The study of PSD has also led to possible interventions that may facilitate motor and cognitive recovery. Emerging insights into the connectome, BDNF, and the role of the poststroke inflammatory cascade are leading to better understanding of PSD and may, in time, identify new prophylactic or therapeutic options.